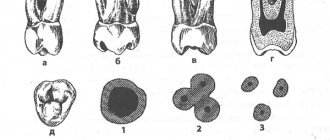
Central upper incisor
Average age of eruption: 7-8 years
Average age of root formation: 10 years
Average length: 22.5 mm
The crown of the central upper incisor, close to rectangular on the vestibular side and wedge-shaped on the proximal side, allows for convenient endodontic access and is ideally positioned for direct examination using a mirror. The tooth is especially suitable for the novice doctor, since in it the canal is directly visible for a third of its length. With fiber optic illumination, the view of the channel can be improved.
Primary opening using a fissure bur is made immediately above the enamel palatal tubercle of the equatorial third of the crown on the lingual surface of the tooth. The instrument is directed along the long axis of the root. Based on the final shape of the access cavity, a triangular hole is made. Trephination of the tooth cavity often occurs during the first implantation. After the feeling of “falling” into the pulp chamber, the fissure bur is replaced with a spherical bur No. 4-6 with an extended shank.
A ball bur is used to widen the hole towards the incisal edge. You need to make sure that the pulp cavity is completely open. A fissure bur may again be required to widen the access cavity and give it its final shape. At this time, all carious dentin, which has significantly changed its color and pulp calcifications, is removed. It is necessary to remove leaking fillings and treat proximal carious cavities with adequate temporary filling.
The root is quite characteristically cone-shaped and sharply tapering towards the apex. The cross-section of the root canal approaches triangular in the cervical part, gradually becoming rounded closer to the apical foramen. Multiple canals in the root are rare, but accessory and lateral canals are common. The apical foramen is rarely located exactly at the apex, but is usually within 2 mm laterally.
Lateral upper incisor
Average age of teething: 8-9 years
Average age of root formation: 11 years
Average length: 22.0 mm
The crown of the upper lateral incisor, approximating an oval shape, is almost ideal for endodontic access, as is the case with the central incisor. Fiber optic illumination is also helpful when accessing this tooth.
The initial opening using a fissure bur is made immediately above the enamel tubercle in the equatorial third on the palatal surface of the tooth. The access cavity is oval in shape. When performing the initial opening, the fissure bur often occupies the entire narrow cavity of the coronal pulp. After removing the roof of the pulp chamber, a ball-shaped bur No. 4 or 6 is used to clean it from carious dentin, pigmented areas and calcifications.
A fissure bur may again be required to finalize the oval shape of the access cavity.
Adequate expansion is then created using spherical burs. Care must be taken to ensure that probes, endodontic cutting instruments and condensation instruments do not come into contact with the walls of the access cavity.
To ensure the cleanliness of the canal walls and their hermetically sealed filling, all carious tissues and leaky fillings must be removed and replaced with temporary filling materials.
The cross-section of the canal varies from oval in the cervical part to round in the apical foramen. The root is slightly cone-shaped and can bend at the apical part, usually in a distal direction. The apical foramen is often located closer to the anatomical apex than the central incisor, but can be located laterally within 1-2 mm of it.
In rare cases, access is complicated by the presence of a “tooth-in-tooth” developmental anomaly, invagination of part of the lingual surface of the tooth into the crown. This creates a space in the tooth that is surrounded by enamel and communicates with the oral cavity. Tooth-in-tooth is most common in the upper lateral incisors, but can occur in other teeth. Due to anatomical developmental defects, these teeth are prone to caries and the pulp may die before the apex is fully formed. This formation (“tooth within a tooth”) is localized in the crown; it must be processed mechanically and removed or bypassed.
Structure
The anatomical structure of the crest includes the base of the process with alveoli, separated by septa. This is where teeth develop and grow. The ridge consists of two walls - the outer one on the side of the cheek and the inner one, turned towards the tongue. The surface is lamellar, it is adapted to support row units of different types, differing in structure and loads.
The process of the maxilla is located between the plates, it acts as an integral part of the cancellous bone. Between the individual alveoli of the structure there are partitions that separate the tooth sockets. At the same time, the cells of the area constantly take part in the formation and resorption of bone, this process is compensatory, in this case it proceeds normally. The features of the ridge allow it to adapt to different conditions, which makes the functioning of the dentition correct.
The crest of the lower jaw has an unpaired and symmetrical structure. Externally, the site forms an arc with a main center and two branches. Alveolar axons are located on each side in an amount of 8 pieces. The sockets can have different shapes and sizes, depending on the position of the units, but most often they are cone-shaped alveoli. For areas where teeth with multiple roots develop, there are partitions that separate the canals.
Upper canine
Average age of teething: 10-12 years
Average age of root formation: 13-15 years
Average length: 26.5 mm
As the longest tooth, the canine has an imposing shape designed to withstand strong occlusal forces. Its long crown with a thick layer of enamel is subject to abrasion by the cutting edge. As she ages, she often has deep cervical erosions.
The access cavity corresponds to the shape of the lingual surface of the crown and is oval. To obtain direct access, the cavity must be expanded incisally, but not so much as to weaken the actively functioning cusp. The initial access is made in the middle part of the crown from the palate. If the pulp cavity is deeper, a No. 4 or 6 ball-shaped extended bur may be required. A sweeping motion with this bur will open up the oval pulp cavity.
As it moves through the cervical portion and down apically, it remains oval. Thorough cleaning of this oval-shaped canal is difficult, so attention must be paid to targeted file processing.
The root canal is quite straight and long. Most canines require instruments 25 mm or longer in length. The last 2-3 mm of the top often bends in some direction.
The morphology of the canines rarely changes radically, and lateral and accessory canals are less common than in the upper incisors.
The vestibular cortical plate over the apex of the tooth root is often destroyed to form a fenestration. The apical foramen is usually located close to the anatomical apex, but can be located laterally, especially if there is an apical bend of the root.
Upper first premolar
Average age of teething: 10-11 years
Average age of root formation: 12-13 years
Average length: 20.6 mm
The first upper premolar is a transitional tooth between the incisor and molar and most often has two roots.
When molars are lost, the main chewing load falls on the premolars. In removable prosthetics, these teeth are used as supporting teeth, which increases the impact of torque on them. Additional torque forces, together with deep carious lesions, can cause severe calcification of the pulp cavity. Early molar loss often causes rotation of the premolars, which can make identification of the pulp chamber difficult.
The mouths of the canals are located below and somewhat to the center of the tops of the mounds. The initial opening is made in the central fissure, giving it an oval shape in the bucco-palatal direction. After identifying the mouth, the doctor must accurately determine the presence of an anastomosis leading to the mouth of another canal. The direction of the roots can be determined using an endodontic probe. Root bifurcation visible on a routine periapical photograph may indicate tooth rotation. With divergent roots, less expansion of the occlusal approach is required, and with parallel roots, on the contrary, it may be necessary to remove the crown tissue towards the tops of the cusps. All infected dentin and leaking fillings should be removed and replaced with suitable temporary fillings.
Options for root anatomy include fused roots with separate canals, interconnecting canals or a “web,” a common apical foramen, and the possible presence of three roots, which is rare but should always be kept in mind. In the latter case, the mouths of the buccal canals will not be clearly visible using a dental mirror. An endodontic probe or a thin file will help determine the structure of the canal. Cams and Skidmore report that maxillary premolars with three roots and three apical foramina are found in 6% of cases. The length of the root is much shorter than that of the canine, and a distal bend is not common. The apical foramen is usually located close to the anatomical apex. The length of the roots when using intact tubercles as reference points is usually the same. The apical part of the roots often tapers sharply, ending in very narrow and curved tips.
Given the possibility of vertical mesial-distal fractures of the crown or root of the first premolar, before endodontic treatment, all fillings should be removed and the crown should be carefully examined under fiber light.
To prevent vertical fractures of the crown or root after endodontic treatment, it is necessary to completely close the occlusal access cavity.
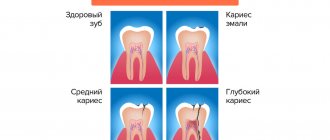
Features of the clinical picture of chronic fibrous periodontitis
This form is rare in children. In the apical zone of the roots, coarse fibrous connective tissue is formed, replacing the periodontium. Such fibrosis occurs after acute periodontal inflammation or after injury. Sometimes it develops after pulpitis or other forms of chronic periodontitis. The gap sometimes narrows due to excess cementosis.
The disease is also asymptomatic, without pain. The tooth can be intact or filled, with painless percussion. On an x-ray, the periodontal fissure is unevenly widened or narrowed. To clarify the diagnosis, the age of the child is taken into account.
Second upper premolar
Average age of teething: 10-12 years
Average age of root formation: 12-14 years
Average length: 21.5 mm
Similar to the first premolar in crown shape, the second premolar differs mainly in its root shape. Its crown is narrower in the bucco-palatal direction and somewhat wider in the mesial-distal direction. The mouth of the canal is located in the center, but it is more slit-like than oval. In the presence of a slit-like orifice, the physician should assume the presence of two canals until proven otherwise.
The external shape of the tooth is slightly oval, but wider in the mesial-distal direction than that of the first premolar.
All infected dentin and leaking fillings should be removed and replaced with temporary fillings.
The root may have two separate channels connecting into one, or two channels interconnecting in the form of a “web”. Accessory or lateral canals are possible but are less common than in incisors. Vertucci et al found that 75% of upper second premolars had one foramen at the apex, 24% had two foramina, and 1% had three foramina. Of all the teeth studied, 59.5% had additional canals. These investigators reported that when two canals are joined into one, the palatine canal is often directed toward the apex in a straight line. They further stated that “if, on a direct periapical photograph, the root canal sharply narrows or even disappears, this means that at this point it is divided into two canals, which either remain separate (type V) or, before reaching the apex, merge again (type II)".
The length of the root of the second upper molar is comparable to that of the first premolar. Apical bending is common, especially with a large volume of the maxillary sinus.
To prevent vertical coronal or crown-root fractures after endodontic treatment, complete closure of the occlusal access cavity is necessary.
How does the chronic form of granulating periodontitis occur?
A problem tooth always has a filling or a pathological carious cavity, which causes pain when probed. There is no reaction to high or low temperatures, and painless percussion is also observed. Sometimes granulation tissues grow from the source of destruction in the peri-apical region into the root canals, which causes bleeding and slight pain upon probing.
A mandatory sign is a fistula through which granulations bulge and pus is released. The mucous membrane is swollen, hyperemic, and has a cyanotic tint. One of the most dangerous complications is the death of the growth plate and stopping further bone formation.
X-ray signs
X-ray images clearly show the destruction of the cortical alveolar plate and a noticeable focus of resorption of spongy bone tissue with unclear contours at the apex. Destruction also occurs in the area of bifurcation of molars. Pathological root resorption in permanent teeth is much less common than in temporary teeth.
Differential diagnosis
It is important to distinguish the disease from such diseases with similar symptoms:
- chronic fibrous and gangrenous pulpitis;
- deep chronic caries;
- pulpitis, with a history of complicated focal periodontitis.
Upper first molar
Average age of teething: 6-7 years
Average age of root formation: 9-10 years
Average length: 20.8 mm
The largest in size, with a complex anatomy of the root and root canal system, the so-called “6-year molar” is the most frequently treated, while presenting the greatest difficulties in treatment among the posterior teeth. During its treatment, the largest number of endodontic errors and complications arise, and it is undoubtedly one of the functionally important teeth.
The three separate roots of the maxillary first molar form a trifurcation: the palatal root is the longest, and the distal buccal and mesiobuccal roots are approximately the same length.
The palatal root in the apical third often curves in a buccal direction. Of the three channels, it has the largest diameter and is the easiest to access. Its mouth is shifted to the palatal wall of the crown. The root deviates sharply from the median axis of the tooth. In cross section, the root is flattened and has a ribbon-like shape, which requires special attention when cleaning and instrumenting it. Fortunately, it rarely has more than one apical foramen.
The distal buccal root is conical and usually straight. It always has one channel.
The mesiobuccal root of the first molar has generated more research, clinical inquiry, and frustration than any other root in the oral cavity. Green showed that 14% of the mesiobuccal roots of the maxillary first molars studied had two apical foramina, and 36% of the roots had two orifices. Pineda reported that 42% of these roots had two canals and two apical foramina. Slowey confirmed Pineda's data within a few percent difference. The fact that nearly half of these roots have two canals, whether they end in a single opening or not, is reason enough to always assume two canals until careful examination proves otherwise.
The additional orifice lies centrally, between the orifices of the mesiobuccal and palatine canals. The search is facilitated by using fiber optics and by identifying the anastomosis between the orifices of the mesiobuccal and palatal canals. The second canal in the mesiobuccal root will always be narrower than the other canals, so it is more difficult to clean and shape. Access to the main mesiobuccal root canal is easier when a straight entry is properly created.
All carious tissue, leaking fillings and denticles must be removed before endodontic treatment begins.
After treatment, complete closure of the approach is necessary to prevent vertical coronal or crown-root fractures. If indicated, internal reinforcement with intraradicular pins is recommended.
Diagnostics and correction
The pathological condition can be detected during a routine examination. In this case, the doctor prescribes an x-ray, which allows you to clarify the diagnosis and determine what the treatment regimen will be. Various methods are used to restore the structure; indications for correction are:
- atrophic processes affecting the ridge;
- defects caused by injuries, chronic diseases, surgical interventions.
Treatment is prescribed depending on the degree and severity of the pathology, tissue condition and other factors. The correction process usually includes the following steps:
- administration of anesthesia (conduction is used);
- surface treatment using antiseptic agents;
- removal of bone tissue particles, including fragments, if the cause of the intervention was injury or gradual destruction of the ridge;
- eliminating remaining sharp edges;
- closing the wound, applying sutures and dressings.
The exact procedure depends on the reason for the surgery, for example, you want to reduce a dislocation rather than remove sections of bone. To do this, a complete study is first carried out. After completing treatment measures, the Patient is required to comply with certain actions:
- exclude physical activity during rehabilitation;
- cessation of smoking, alcoholic beverages, and other bad habits;
- correction of the diet, exclusion of solid and spicy foods for the period of healing and recovery;
- observe the rules of personal hygiene, take care of the oral cavity;
- rinse your mouth after every meal using antiseptic agents.
Correction of the appendix is a complex stage of prosthetics or elimination of various pathologies caused by injuries or developmental disorders. Treatment should only be carried out by a qualified doctor with experience in this field.
Second upper molar
Average age of teething: 11-13 years
Average age of root formation: 14-16 years
Average length: 20.0 mm
The shape of the crown of the second upper molar is very similar to the first upper molar, although it is not as rectangular and massive. Adequate access on both teeth can usually be achieved without disturbing the transverse enamel ridge. The second molar is often easy to prepare due to the straightforward approach to the orifices.
A distinctive feature of the morphology of the upper second molar is the closely spaced and sometimes fused three roots. The shadows of parallel root canals often overlap on the radiograph. Its roots are usually shorter than those of the first molar and not as curved.
The three orifices may form a blunt triangle, and sometimes they are located almost in a straight line. The floor of the pulp chamber is noticeably convex, creating a slightly funnel-shaped shape of the canal orifices. Sometimes the canals extend from the bottom of the pulp chamber at an acute angle, resulting in the need to remove the edge of the dentin in order to create a straight line of access.
Complications during access occur if the molar is tilted distally. Initial exposure is performed with a fissure bur with a cutting tip, and then a short ball-shaped bur is used, which is best suited for opening the pulp chamber and forming an access cavity. Then, small hand instruments are used to establish the patency of the canal and its working length. After this, the bulk of cleaning and shaping can be done by machining the files in the endodontic handpiece.
To improve radiographic visibility, especially when layering the shadow of the process of the zygomatic bone, photographs can be taken in perpendicular and distal projections at an angle.
All infected dentin, leaking fillings and denticles must be removed before endodontic treatment begins. To prevent vertical coronal or crown-root fractures, it is necessary to completely close the access cavity. If indicated, immediately after endodontic treatment it is necessary to apply internal reinforcement with intraradicular pins.
Acute periodontitis of permanent teeth
Acute periodontitis in children often occurs after a tooth injury or due to incorrect treatment of pulpitis.
- Serous acute periodontitis.
The pain in the causative tooth increases, but the general condition of the child is not disturbed. The tooth is intact or has a fractured crown. If periodontitis is of toxic origin, there are signs of carious cavity preparation. If the pulp is dead, probing is painless, there is no reaction to temperature. On the mucous membrane of the gums there are symptoms of minor inflammation. There are no signs on the X-ray yet. A day later, the serous phase turns into a purulent phase.
- Acute purulent periodontitis.
Accompanied by constant throbbing pain and sharp pain even with a slight touch. Body temperature rises and intoxication begins. The tooth is intact, previously treated or with a carious cavity, mobile due to the accumulation of pathological exudate in the periodontal gap. An abscess forms under the periosteum, and sometimes facial asymmetry develops. X-ray also does not show anything concrete, except for a lower clarity of the picture.
It is important to distinguish acute purulent periodontitis from the following diseases:
- acute diffuse pulpitis, with a history of perifocal periodontitis (painful probing);
- acute purulent pulpitis, complicated by perifocal periodontitis (pain intensifies with hot stimuli and calms down with cold stimuli);
- exacerbation of periodontitis (changes in the periapical zone);
- acute odontogenic periostitis and another no less insidious disease - osteomyelitis.
Exacerbation of chronic periodontitis in molars with incomplete root growth is more common than the acute form. The tooth constantly hurts, percussion is also painful. The mucous membrane of the alveolar process swells and turns red, the crown changes color, and sometimes a fistula appears. The X-ray shows destruction of the cortical alveolar plate, a segment of bone clearing and deformation of the periodontal fissure.