There are many clinical conditions whose nature and distribution can be clarified by MRI.
To begin with, it is worth saying a few words about the development options, of which the most common are hypoplasia and aplasia of the sinuses.
Hypoplasia of the frontal sinus
Particularly noteworthy is such a development option as excessive pneumatization of the sphenoid sinus and posterior ethmoid cells in the form of developed upper lateral recesses, in the presence of which the internal carotid arteries and optic nerve canals can protrude into their lumen. As a result, during inflammatory processes in the mucous membranes of these sections (including subacute and chronic), a clinical picture of progressive atrophy of the optic nerves may develop. In addition, when performing surgical interventions in this anatomical area, the risk of damage to the carotid arteries and optic nerves increases many times.
Developed superolateral recesses, against which the optic nerves are identified
Inflammatory changes in the paranasal sinuses are the most common diseases of the upper respiratory tract. From 5 to 15% of the world's population suffers from various types of sinusitis. In addition, there is a trend towards an increase in chronic forms.
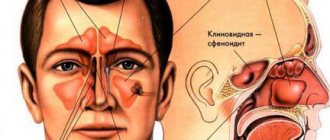
Facial pain with sinusitis is localized in the projection of the affected sinus. With frontal sinusitis and sinusitis, in addition to pain, there is pain on palpation. Ethmoiditis and sphenoiditis are characterized by constant pain in the eye and nose and nasal congestion. Diagnosis of chronic sinusitis is especially difficult. With mucoceles and tumors, swelling and displacement of the eyeball are observed: upward - with damage to the maxillary sinus, outward - with damage to the ethmoidal labyrinth, and downward - with damage to the frontal sinus.
Let's look at examples of pathology of the paranasal sinuses detected during an MRI examination.
Swelling of the mucous membrane of the right maxillary sinus with fluid level
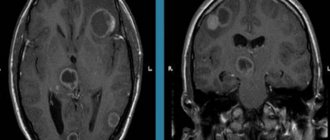
MR picture of polysinusitis with a total disturbance of pneumatization of the cells of the ethmoid bone, moderate, sometimes uneven, local disturbance of pneumatization of the right half of the main sinus and the upper parts of the left maxillary sinus, without an exudative component.
What does a sinus x-ray show?
An x-ray shows the human skull with bone structures, cavities and septa. The method is used at the preparatory stage in surgery.
What can be seen on a sinus x-ray:
- Foreign object in the nasal passages.
- Inflammatory process, thickening of the mucous membrane of the infected area.
- Consequences of injuries to the face and head.
- The presence of exudate (mucous, blood, purulent) in the paranasal and frontal cavities.
- "Airiness" of the sinuses.
- Neoplasms: polyps, tumors, cysts.
- Anomalies in the structure of the facial skeleton.
X-rays help to correct the diagnosis in case of fever or headache of unknown etiology.
X-ray methods for examining the nose and paranasal sinuses
An ENT disease similar to inusitis
is currently the most common ENT pathology.
Patients with inflammatory processes of the paranasal sinuses (SNS) currently make up about 40% of all patients hospitalized in ENT hospitals. The main method for diagnosing diseases of the urinary tract is radiological.
This is due to the fact that the air-containing sinuses of the nose are located deep in the bones of the facial skull, communicating with the nasal cavity only through small openings - anastomoses.
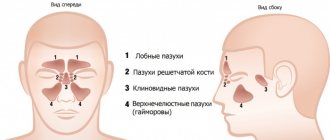
It is customary to distinguish the following paired SNPs located in the bones of the same name (Fig. 1):
- maxillary;
- frontal;
- lattice;
- front and rear;
- wedge-shaped.
In some cases, the paranasal sinuses also include air cavities, which are rare in some patients and located in the thickness of the nasal septum of the nasal concha (turbinate bullae). These cavities, lined with epithelium, almost never communicate with the nasal cavity and therefore cannot be considered true sinuses.
In a newborn child, only the maxillary and ethmoid sinuses are developed (Fig. 3), which are cavities with a volume of less than a milliliter. By 2–3 years the sphenoid sinus becomes pneumatized, and by 5–6 years the frontal sinus becomes pneumatized. The final development of the sinuses is achieved by the age of 20.
Underdevelopment of the frontal sinuses or their hypoplasia occurs in every 10th person. Underdevelopment of other sinuses is observed quite rarely. There may be unilateral hypo- and aplasia of the maxillary, sphenoid and frontal sinuses, which must be noted in the description of the radiograph. This creates difficulties in diagnosing sinusitis and puncture of such a sinus (Fig. 4). Excessive pneumatization of the SNP is possible, most often the frontal and sphenoid.
An X-ray of the skull does not allow us to assess the condition of all SNPs. To obtain a high-quality image of the SNP, it is necessary to conduct the study in a special projection.
The following types of projections are distinguished:
- nasomental;
- nasofrontal;
- mental or axial.
These projections are needed to shift the image of the pyramids of the temporal bones and the entire base of the skull below the bottom of the maxillary sinuses (nasomental position) or above them into the orbit (nasofrontal position). If this condition is not met, the pyramids of the temporal bones simulate fluid levels in the maxillary sinuses.
Nasomental projection
performed with the patient in an upright position (sitting, standing). The patient is asked to open his mouth and press it against the screen (Fig. 5). The central ray is directed perpendicular to the cassette and passes in the sagittal direction at the level of the outer corners of the orbits. All anterior sinuses (frontal, ethmoid, maxillary) are clearly visible. In the projection of the open mouth, you can see the sphenoid sinus (Fig. 1).
Sometimes, in this position, the pyramids of the temporal bones still overlap the lower parts of the maxillary sinuses and it is recommended to perform a chin (anterior semi-axial) projection, when the sitting patient touches the cassette with his chin.
The line connecting the external auditory canal and the chin (mental) is perpendicular to the plane of the cassette. The central ray runs through the wings of the nose parallel to the mental line. The ethmoid sinus in this case is poorly visible due to the layering of the anterior cells on the posterior cells and on the slopes of the nose. The frontal sinuses appear enlarged.
Nasofrontal projection
used to study the frontal and ethmoid sinuses. The patient presses his forehead and tip of his nose against the cassette. The central beam passes perpendicular to the cassette through the back of the head.
Currently, the nasomental projection is most often used.
A survey radiography of the skull in a lateral projection allows one to assess the depth and condition of the walls of the frontal, sphenoid sinuses, maxillary and nasopharynx (Fig. 6).
Sometimes special installations are used for targeted examination of a specific sinus: X-ray according to G.M. Zemtsov to identify the sphenoid sinus in the projection of the open mouth (nasochin position with maximum tilting of the head), according to Ya.A. Fastovsky targeted examination of the ethmoid labyrinth and others.
There are difficulties in performing X-ray examinations on mobile and excitable patients and young children. It is necessary to hold them in the desired position or conduct the examination under anesthesia. In this case, the attending physician must determine how much X-ray examination is necessary in making a diagnosis.
Sometimes the required projection is prevented by stiffness of the joints (spine, temporomandibular) or muscle rigidity (for example, stiffness of the neck muscles with meningitis).
Normally, during X-ray examination, air-containing SNPs appear as light areas with a clearly defined dark outline corresponding to their bony border. Typically a negative X-ray image is described, so areas containing more white are called darker. Pneumatized SNPs correspond to orbital transparency. If the contents of the sinuses are darker than the contents of the orbits, then they speak of darkening, which means the presence of a pathological process
. In this case, it is necessary to characterize the darkening according to several parameters. The first of these is the size or degree of filling of the sinus with a pathological process.
They are distinguished (Fig. - Scheme 8):
- total (complete) darkening of the sinus
, almost complete -
subtotal
(Fig. 8 a), which correspond to the complete filling of the sinus with contents, which can be either exudate or edematous soft tissue. - darkening in the lower sections with an upper horizontal level
means the presence of liquid, exudate (Fig. 8 b). - parietal darkening
, following the contour of the sinus walls, corresponds to thickening of the mucous membrane (Fig. 8 c).
If normally the thickness of the mucous membrane in the SNP is 120 - 1000 microns and is not visible on an x-ray, then with inflammation and allergic edema it can increase tens and hundreds of times, giving parietal darkening.
- In the sinus there may be limited darkening
emanating from one or two walls (Fig. 10 a).
In this case, it must have a designated shape
(round, oval, irregular),
size
(in centimeters or millimeters) and
contours
(smooth or uneven).
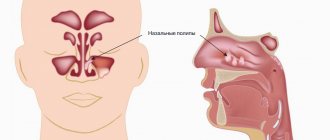
Such limited processes correspond to polyps, cysts, tumors
.
The second mandatory characteristic of darkening is intensity
, which means the degree of delay of the X-ray beam when passing through the sinus. There are three degrees: small, medium and high.
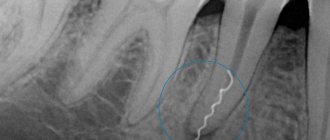
High intensity
means complete absorption of x-rays in tissue and corresponds to bone structures and radiopaque foreign bodies. In the sinus, high-intensity darkening is compared with the intensity of nearby bone formations: teeth, nasal bones. High intensity darkening in the sinuses can be caused by additional (superset) teeth, osteomas, bone fragments and foreign materials (shot, bullets, filling material that got into the maxillary sinus during the treatment of pulpitis of molars or premolars of the upper jaw, etc.).
Low intensity dimming
corresponds to serous exudate, swelling of the mucous membrane and appears on the radiograph only slightly darker than the orbits.
Medium dimming
delays the X-ray beam less than the surrounding bone structures, and corresponds to soft tissue formations (they can be tumors, cysts, polyps) or thick exudate (purulent or mucosal).
Different sinuses may have different pathological processes and varying degrees of their severity. For example, left-sided purulent maxillary sinusitis and a cyst of the right frontal sinus.
Sinusitis
characterized by thickening of the sinus mucosa, the presence of exudate in it, which determines the form of the disease (purulent, catarrhal, serous). During the catarrhal process, a parietal darkening is noted in the sinus; an increase in edema can lead to a uniform total darkening. In the exudative form of sinusitis, darkening is detected in the lower sections with an upper horizontal level (Fig. 9). This level does not reach the bony walls of the sinus with severe swelling of its mucous membrane.
The intensity of the darkening can help to differentiate the nature of the exudate: medium intensity corresponds to a purulent process, low intensity to a serous one. When a large amount of exudate accumulates, the level is not determined - the darkening is total homogeneous. This may indicate the formation of a sinus empyema. Total homogeneous darkening of the sinus of low and medium intensity may correspond to severe swelling of the mucous membrane.
To correctly interpret the X-ray picture, it is important to know the clinical examination data: the presence of purulent secretion in the nasal cavity, body hyperthermia, and the severity of pain. The pain syndrome may be more pronounced with swelling in the sinus than with its empyema, when compression and death of nerve endings occurs. In such difficult cases, they resort to computed tomography
or
diagnostic puncture of the sinuses
.
Drainage of exudate is radiologically manifested by the restoration of transparency, starting from the superomedial angle of the maxillary sinus and the upper part of the frontal and sphenoid sinuses. After resorption or removal of exudate, thickening of the mucous membrane is determined in the form of residual wall deposits that persist for several weeks. This is especially true for the maxillary sinuses, in which the fluid level may be due to the injected medication during their previous drainage.
In everyday clinical practice, it is advisable to carry out control X-ray examinations immediately after the end of treatment only to determine the condition of the frontal sinuses.
Chronic sinusitis
has no characteristic manifestations, but more often there are productive forms in the form of rounded darkenings emanating from different walls of the sinuses, corresponding to polyps, cysts (Fig. 10 a), granulomas. The latter may be of odontogenic (dental) nature.
Large cysts can cause a total darkening of the sinus, simulating its empyema. Mucocele of the sinus should be distinguished from a cyst
, which does not have its own membrane and leads to stretching of the walls of the sinus due to obliteration of its natural anastomosis (Fig. 10 b).
When the sinus is stretched with air as a result of the valve mechanism, stretching and thinning of the walls are also noted, but the pneumatization of the sinus is increased. When foreign bodies (filling material) get into the sinus, a fungal body may form around them - mycetoma
, which has a rounded outline on an x-ray (Fig. 11).
How is a sinus x-ray performed?
The procedure is not painful and does not require preparation. Receive a referral at an appointment with an otolaryngologist, infectious disease specialist or surgeon.
How to do a sinus x-ray:
- The patient removes metal jewelry, glasses, and dentures.
- To protect against radiation, he wears a lead apron or vest with a collar.
- The laboratory assistant indicates how to position yourself correctly relative to the apparatus. Depending on the required projections, the position is changed at the command of a specialist.
- While taking the photo, you should not move and hold your breath.
- After development and decoding, the film with the description is given to the patient.
The conclusion is not considered a final diagnosis, but provides clarifying information for the treating specialist.
Darkening of the sinuses on x-ray
The method is based on the different permeability of hard and soft tissues by electromagnetic waves. Bones block radiation and appear white in the picture. Specialists are interested in blackouts, which determine the nature of the disorder.
Darkening of the sinuses on an x-ray indicates fluid accumulation. This is a sign of inflammation with the release of mucous or purulent secretion. Sometimes, the picture shows thickening of the walls of the mucous membrane lining the sinuses.
New growths stand out as clear dark spots with shadows. Polyps look like peas on a “pedicle”, and cysts have a cavity filled with fluid inside.
conclusions
1. High-tech methods of radiological diagnostics (MSCT or CBCT) are a necessary component of the complex diagnosis of HFRS.
2. The use of computed tomography (MSCT or CBCT) makes it possible to determine the cause of AHF and, thus, choose the correct tactics for patient management.
3. MSCT or CBCT should be recommended to patients before and after endodontic treatment of teeth and dental implantation, as well as during surgical interventions on the upper jaw in order to timely identify possible pathological changes in the maxillary sinuses (including asymptomatic ones).
Conflict of interest: The authors of the article have confirmed that they have no financial support/conflict of interest to report.
X-ray of the sinuses during pregnancy
The radiation dose during the study is 20 μSv and is considered safe even when performed repeatedly for an adult. The fetus is susceptible to ionizing radiation, which causes intrauterine developmental defects. Carrying a child is a contraindication to the procedure.
X-rays of the nasal sinuses during pregnancy and breastfeeding are done exclusively for health reasons. The potential benefit of the research must outweigh the harm to the child. After the procedure, a pregnant woman needs an ultrasound of the fetus, and a nursing woman needs to transfer the baby to artificial nutrition for a day.
The harm of self-medication
The most obvious harm of self-medication is the lack of positive results. People often take medications until they feel better. However, this approach is wrong. Antibacterial drugs should be taken only as prescribed by a doctor. Strictly in the volumes and within the time frame that he announced at the reception. Otherwise, the symptoms will go away, but the source of infection will remain. Inflammation in the maxillary sinus will become chronic.
Or, if the drugs were chosen incorrectly, there may be no improvement at all. The disease will become advanced, the pain due to overcrowded sinuses will become unbearable, and inflammation will have a chance to spread to the organs and tissues closest to the sinuses, causing all sorts of complications.
Another risk of self-medication is the medications that must be taken for sinusitis. If the dosage is incorrect, taken too often, or if there are problems with internal organs, antibacterial drugs can do more harm than good. Cases of drug-induced liver damage from uncontrolled use of antibiotics are not so rare. What can we say about gastrointestinal tract disorders, dysbacteriosis, and so on.
X-ray of the sinuses for children
Pediatricians try to protect preschool children from the harm caused by X-ray radiation to the fragile skeletal system. The procedure is allowed to be performed on patients over 7 years of age.
Before this period, a clear justification for the importance of intervention is necessary - for example, severe facial trauma or severe sinusitis with a risk of inflammation of the meninges.
It is difficult for a young child to sit or stand still during an x-ray. To distract him, they use toys, sedatives, and in emergency cases, anesthesia. At an older age, you can captivate your child with a game in which you should freeze for a short time.
Sign up for the study