Causes of candidal stomatitis
The most common cause of candidiasis stomatitis is a fungus of the Candida albicans group. It is worth noting that these fungi are always present on the mucous membranes of the mouth, and do not cause any harm to the body until they begin to multiply.
The causes of the development of candidal stomatitis are the following factors and diseases:
- Weak immunity;
- People with Sjögren's syndrome;
- Neglect of general rules of oral hygiene;
- Constant stress;
- Various diseases of the oral cavity;
- Taking antibiotics or corticosteroids;
- Having a disease such as diabetes. This is all due to the fact that the blood contains a large amount of sugar, and this serves as an excellent environment for the development of fungus of the genus Candida.
It is also worth noting that adults who suffer from excessive dry mouth can get candidal stomatitis. The most common cause of such dryness is the abuse of dental elixirs.
Another factor that can cause the development of candidal stomatitis is pregnancy. After all, it’s no secret that it is during this period that significant hormonal changes occur in a woman’s body, which, in turn, greatly affect the bacterial balance in the mouth.
Contraindications for use
Medical contraindications for taking Fluconazole capsules are pathological and physiological processes in the patient’s body, which include:
- Simultaneous use of the drug terfinadine, astemizole, as well as other drugs that lead to prolongation of the QT interval on the electrocardiogram (especially when using Fluconazole capsules in a daily dosage exceeding 400 mg).
- Children up to 4 years old.
- Individual intolerance to the main active ingredient or additional substances of this medication.
The drug is used with caution in case of concomitant liver or renal failure, the appearance of a skin rash in patients with generalized systemic fungal infections, simultaneous use of the drug in a daily dosage of less than 400 mg with terfenadine, chronic alcoholism, in the case of the use of drugs that have a hepatotoxic effect, and also in patients with a high risk of developing arrhythmia (disturbance in the rhythm and frequency of heart contractions) against the background of organic heart pathology, electrolyte imbalance in the body. The drug is also used with caution in pregnant women. Before prescribing Fluconazole capsules, the doctor makes sure that the patient has no contraindications.
Symptoms
A number of symptoms are characteristic of candidal stomatitis:
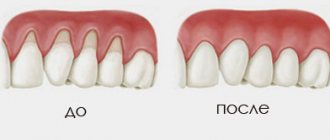
- The appearance of a white or yellowish coating on the tongue, cheeks or palate. When trying to eliminate it, bleeding wounds may appear on the mucous membrane.
- Constant metallic taste.
- Feeling of heartburn on the tongue.
- Painful sensations from touching plaque.
- Later, as plaque spreads, difficulty swallowing occurs.
- Deterioration of tongue sensitivity and poor taste perception.
Side effects
Side effects are possible when using the drug Fluconazole
- From the immune system: hypersensitivity (cross with all azoles), other anaphylactic, anaphylactoid and allergic reactions (including Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria).
- From the nervous system: headache, dizziness, peripheral neuropathy, paresthesia, excessive fatigue, rarely - convulsions.
- From the digestive system: loss of appetite, dryness of the oral mucosa, changes in taste, abdominal pain, vomiting, nausea, diarrhea, flatulence, rarely - impaired liver function (jaundice, hepatitis, hepatonecrosis, hyperbilirubinemia, increased activity of alanine aminotransferase, aspartate aminotransferase, increased alkaline phosphatase activity, hepatocellular necrosis), including severe.
- From the hematopoietic organs: rarely - leukopenia, thrombocytopenia (bleeding, petechiae), neutropenia, agranulocytosis.
- From the cardiovascular system: increased duration of the QT interval, ventricular fibrillation/flutter, torsades de pointes.
- Metabolism: hypercholesterolemia, hypertriglyceridemia, hypokalemia, hyperglycemia.
- From the musculoskeletal system: myalgia.
- Other: weakness, asthenia, peripheral edema, neutropenia, itching, pulmonary edema, fever, excessive sweating, vertigo.
Forms of the disease
Candidal stomatitis is a fairly common disease that manifests itself in various forms. The symptoms can determine how much it is progressing. Treatment depends on the severity of the disease.
In the earliest stages, a mild form of the disease appears. It is characterized by the formation of single small white spots on the tongue or cheeks.
In the next middle stage, ulcers may form, and white spots themselves cover most of the tongue and mouth.
And at the most severe stages, plaque cannot be removed - it completely covers the entire oral cavity and forms a white film. Also, candidal stomatitis is classified separately depending on the location:
- Candidal stomatitis of the corners of the mouth. Very small cracks appear at the corners of the mouth, which cause pain. This is especially evident when opening the mouth.
- Yeast glossitis usually occurs on the surface of the tongue. It is characterized by a white coating and even swelling of the tongue.
- Thrush - the so-called yeast stomatitis - is a disease in which plaque forms on the cheeks and gums. The mucous membrane itself becomes reddened.
Fluconazole
Single or multiple doses of fluconazole at a dose of 50 mg do not affect the metabolism of phenazone (Antipyrine) when taken simultaneously.
Concomitant use of fluconazole with the following drugs is contraindicated:
Cisapride
: with the simultaneous use of fluconazole and cisapride, adverse reactions from the heart are possible, incl.
ventricular tachysystolic arrhythmia of the “pirouette” type ( torsade de pointes
). The use of fluconazole at a dose of 200 mg once a day and cisapride at a dose of 20 mg 4 times a day leads to a marked increase in plasma concentrations of cisapride and an increase in the QT interval on the ECG. The simultaneous use of cisapride and fluconazole is contraindicated.
Terfenadine
: When azole antifungals are used concomitantly with terfenadine, serious arrhythmias may occur as a result of prolongation of the QT interval. When taking fluconazole at a dose of 200 mg/day, an increase in the QT interval has not been established; however, the use of fluconazole at doses of 400 mg/day and above causes a significant increase in the concentration of terfenadine in the blood plasma. Concomitant use of fluconazole in doses of 400 mg/day or more with terfenadine is contraindicated (see section “Contraindications”). Treatment with fluconazole in doses less than 400 mg/day in combination with terfenadine should be carried out under close monitoring.
Astemizole
: simultaneous use of fluconazole with astemizole or other drugs whose metabolism is carried out by the cytochrome P450 system may be accompanied by an increase in serum concentrations of these drugs.
Elevated concentrations of astemizole in blood plasma can lead to prolongation of the QT interval and, in some cases, to the development of ventricular tachysystolic arrhythmia of the “pirouette” type ( torsade de pointes
). The simultaneous use of astemizole and fluconazole is contraindicated.
Pimozide
: Although appropriate
in vitro
or
in vivo
, the simultaneous use of fluconazole and pimozide may lead to inhibition of the metabolism of pimozide.
In turn, an increase in plasma concentrations of pimozide can lead to a prolongation of the QT interval and, in some cases, the development of ventricular tachysystolic arrhythmia of the “pirouette” type ( torsade de pointes
). The simultaneous use of pimozide and fluconazole is contraindicated.
Quinidine
: Although adequate
in vitro
or
in vivo
, concomitant use of fluconazole and quinidine may also lead to inhibition of quinidine metabolism.
The use of quinidine is associated with prolongation of the QT interval and, in some cases, with the development of ventricular tachysystolic arrhythmia of the “torsade de pointes
. The simultaneous use of quinidine and fluconazole is contraindicated.
Erythromycin
: Concomitant use of fluconazole and erythromycin potentially leads to an increased risk of cardiotoxicity (QT prolongation,
torsade de pointes
) and, consequently, sudden cardiac death. The simultaneous use of fluconazole and erythromycin is contraindicated.
Amiodarone
: Concomitant use of fluconazole and amiodarone may result in inhibition of amiodarone metabolism. Amiodarone use has been associated with QT prolongation. The simultaneous use of fluconazole and amiodarone is contraindicated (see section "Contraindications").
Caution and possible dosage adjustments should be used when the following drugs are used concomitantly with fluconazole:
Drugs affecting fluconazole
:
Hydrochlorothiazide
: repeated use of hydrochlorothiazide simultaneously with fluconazole leads to an increase in the concentration of fluconazole in the blood plasma by 40%. An effect of this severity does not require a change in the fluconazole dosage regimen in patients receiving concomitant diuretics, but the doctor should take this into account.
Rifampicin
: Concomitant use of fluconazole and rifampicin leads to a decrease in AUC by 25% and the half-life of fluconazole by 20%. In patients concomitantly taking rifampicin, it is necessary to consider the advisability of increasing the dose of fluconazole.
Drugs Affected by Fluconazole
:
Fluconazole is a potent inhibitor of the cytochrome P450 isoenzyme CYP2C9 and CYP2C19 and a moderate inhibitor of the CYP3A4 isoenzyme. In addition, in addition to the effects listed below, there is a risk of increased plasma concentrations of other drugs metabolized by the isoenzymes CYP2C9, CYP2C19 and CYP3A4 when taken simultaneously with fluconazole. In this regard, caution should be exercised when using these drugs simultaneously, and if such combinations are necessary, patients should be under close medical supervision. It should be taken into account that the inhibitory effect of fluconazole persists for 4-5 days after discontinuation of the drug due to the long half-life.
Alfentanil
: There is a decrease in clearance and volume of distribution, an increase in the half-life of alfentanil. This may be due to inhibition of the CYP3A4 isoenzyme by fluconazole. Alfentanil dosage adjustment may be required.
Amitriptyline, nortriptyline:
increase in effect. Concentrations of 5-nortriptyline and/or S-amitriptyline can be measured at the start of combination therapy with fluconazole and one week after initiation. If necessary, the dose of amitriptyline/nortriptyline should be adjusted.
Amphotericin B:
In studies in mice (including those with immunosuppression), the following results were observed: small additive antifungal effect in systemic infection with
C. albicans
, no interaction in intracranial infection with
Cryptococcus neoformans
and antagonism in systemic infection with
A. fumigatus
. The clinical significance of these results is unclear.
Anticoagulants
: like other antifungal agents (azole derivatives), fluconazole, when used simultaneously with warfarin, increases prothrombin time (by 12%), and therefore bleeding may develop (hematomas, bleeding from the nose and gastrointestinal tract, hematuria, melena). In patients receiving coumarin anticoagulants, prothrombin time must be constantly monitored during therapy and for 8 days after simultaneous use. The advisability of adjusting the warfarin dose should also be assessed.
Azithromycin
: with simultaneous oral use of fluconazole in a single dose of 800 mg with azithromycin in a single dose of 1200 mg, no pronounced pharmacokinetic interaction has been established between both drugs.
Benzodiazepines (short-acting):
After oral administration of midazolam, fluconazole significantly increases midazolam concentrations and psychomotor effects, and this effect is more pronounced after oral administration of fluconazole than when administered intravenously. If concomitant therapy with benzodiazepines is necessary, patients taking fluconazole should be monitored to assess the appropriateness of an appropriate reduction in the benzodiazepine dose. When taking a single dose of triazolam simultaneously, fluconazole increases the AUC of triazolam by approximately 50%, Cmax by 25-50% and T1/2 by 25-50% due to inhibition of triazolam metabolism. Triazolam dose adjustment may be necessary.
Carbamazepine
: fluconazole inhibits the metabolism of carbamazepine and increases the serum concentration of carbamazepine by 30%. The risk of carbamazepine toxicity must be taken into account. The need for carbamazepine dose adjustment based on concentration/effect should be assessed.
Calcium channel blockers
: Some calcium channel antagonists (nifedipine, isradipine, amlodipine, verapamil and felodipine) are metabolized by CYP3A4. Fluconazole increases the systemic exposure of calcium channel antagonists. Monitoring for the development of side effects is recommended.
Cyclosporine
: In patients with a transplanted kidney, the use of fluconazole at a dose of 200 mg/day leads to a slow increase in cyclosporine concentrations. However, with repeated doses of fluconazole at a dose of 100 mg/day, no changes in cyclosporine concentrations were observed in bone marrow recipients. When using fluconazole and cyclosporine simultaneously, it is recommended to monitor the concentration of cyclosporine in the blood.
Cyclophosphamide
: with simultaneous use of cyclophosphamide and fluconazole, an increase in serum concentrations of bilirubin and creatinine is observed. This combination is acceptable given the risk of increased bilirubin and creatinine concentrations.
Fentanyl
: There has been a report of one death possibly related to the concomitant use of fentanyl and fluconazole. The disturbances are believed to be related to fentanyl intoxication. Fluconazole has been shown to significantly prolong the clearance time of fentanyl. It should be borne in mind that an increase in the concentration of fentanyl can lead to depression of respiratory function.
Halofantrine
: Fluconazole may increase plasma concentrations of halofantrine due to inhibition of the CYP3A4 isoenzyme. When used simultaneously with fluconazole, as well as with other azole antifungal drugs, the development of ventricular tachysystolic arrhythmia of the “pirouette” type is possible, so combined use is not recommended.
HMG-CoA reductase inhibitors:
When fluconazole is used concomitantly with HMG-CoA reductase inhibitors metabolized by the CYP3A4 isoenzyme (such as atorvastatin and simvastatin) or the CYP2D6 isoenzyme (such as fluvastatin), the risk of developing myopathy and rhabdomyolysis increases. If simultaneous therapy with these drugs is necessary, patients should be monitored to identify symptoms of myopathy and rhabdomyolysis. It is necessary to monitor the concentration of creatinine kinase. If there is a significant increase in creatinine kinase concentrations or if myopathy and rhabdomyolysis are diagnosed or suspected, therapy with HMG-CoA reductase inhibitors should be discontinued.
Losartan
: Fluconazole inhibits the metabolism of losartan to its active metabolite (E-3174), which is responsible for most of the effects associated with angiotensin-I receptor antagonism. Regular monitoring of blood pressure is necessary.
Methadone
: Fluconazole may increase plasma concentrations of methadone. Methadone dose adjustment may be necessary.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
: Flurbiprofen Cmax and AUC increased by 23% and 81%, respectively. Similarly, the Cmax and AUC of the pharmacologically active isomer [S-(+)-ibuprofen] increased by 15% and 82%, respectively, when fluconazole was administered simultaneously with racemic ibuprofen (400 mg).
With simultaneous use of fluconazole at a dose of 200 mg/day and celecoxib at a dose of 200 mg, the Cmax and AUC of celecoxib increased by 68% and 134%, respectively. In this combination, it is possible to reduce the dose of celecoxib by half.
Although there are no targeted studies, fluconazole may increase the systemic exposure of other NSAIDs metabolized by CYP2C9 (eg, naproxen, lornoxicam, meloxicam, diclofenac). NSAID dose adjustment may be necessary.
When NSAIDs and fluconazole are used concomitantly, patients should be closely monitored medically to identify and monitor NSAID-related adverse events and toxicities.
Oral contraceptives:
with simultaneous use of a combined oral contraceptive with fluconazole at a dose of 50 mg, no significant effect on hormone levels has been established, while with daily administration of 200 mg of fluconazole, the AUC of ethinyl estradiol and levonorgestrel increases by 40% and 24%, respectively, and when taking 300 mg of fluconazole 1 time per week, the AUCs of ethinyl estradiol and norethindrone increased by 24% and 13%, respectively. Thus, repeated use of fluconazole at the indicated doses is unlikely to affect the effectiveness of the combined oral contraceptive.
Phenytoin
: Concomitant use of fluconazole and phenytoin may be accompanied by a clinically significant increase in phenytoin concentrations. If concomitant use of both drugs is necessary, phenytoin concentrations should be monitored and the dose adjusted accordingly to ensure therapeutic serum concentrations.
Prednisone
: There is a report of the development of acute adrenal insufficiency in a patient after liver transplantation upon discontinuation of fluconazole after a three-month course of therapy. Presumably, discontinuation of fluconazole therapy caused an increase in the activity of the CYP3A4 isoenzyme, which led to increased metabolism of prednisone. Patients receiving combination therapy with prednisone and fluconazole should be under close medical supervision when discontinuing fluconazole to evaluate the condition of the adrenal cortex.
Rifabutin
: simultaneous use of fluconazole and rifabutin can lead to an increase in serum concentrations of the latter by up to 80%. Cases of uveitis have been described with the simultaneous use of fluconazole and rifabutin. Patients receiving rifabutin and fluconazole concomitantly should be monitored closely.
Saquinavir
: AUC increases by approximately 50%, Cmax by 55%, clearance of saquinavir decreases by approximately 50% due to inhibition of hepatic metabolism of the CYP3A4 isoenzyme and inhibition of P-glycoprotein. Dose adjustment of saquinavir may be necessary.
Sirolimus
: increased plasma concentrations of sirolimus, presumably due to inhibition of sirolimus metabolism through inhibition of the CYP3A4 isoenzyme and P-glycoprotein. This combination can be used with appropriate dose adjustment of sirolimus depending on the effect/concentration.
Sulfonylureas:
Fluconazole, when administered concomitantly, leads to an increase in the half-life of oral sulfonylureas (chlorpropamide, glibenclamide, glipizide and tolbutamide). Patients with diabetes mellitus can be prescribed the combined use of fluconazole and oral sulfonylureas, but the possibility of hypoglycemia should be taken into account, in addition, regular monitoring of blood glucose is necessary and, if necessary, dose adjustment of sulfonylureas.
Tacrolimus
: simultaneous use of fluconazole and tacrolimus (orally) leads to an increase in serum concentrations of the latter by 5 times due to inhibition of the metabolism of tacrolimus occurring in the intestine through the CYP3A4 isoenzyme. No significant changes in the pharmacokinetics of the drugs were observed when tacrolimus was administered intravenously. Cases of nephrotoxicity have been described. Patients receiving oral tacrolimus and fluconazole concomitantly should be monitored closely. The dose of tacrolimus should be adjusted depending on the degree of increase in its concentration in the blood.
Theophylline
: When used simultaneously with fluconazole at a dose of 200 mg for 14 days, the average rate of plasma clearance of theophylline is reduced by 18%. When prescribing fluconazole to patients taking high doses of theophylline or to patients at increased risk of developing theophylline toxicity, monitor for symptoms of theophylline overdose and, if necessary, adjust therapy accordingly.
Vinca alkaloid
: Although focused studies are lacking, it is suspected that fluconazole may increase plasma concentrations of vinca alkaloids (eg, vincristine and vinblastine) and thus lead to neurotoxicity, which may be due to inhibition of CYP3A4.
Vitamin A:
There is a report of one case of the development of adverse reactions from the central nervous system (CNS) in the form of pseudotumor cerebri with the simultaneous use of all-trans retinoic acid and fluconazole, which disappeared after discontinuation of fluconazole. The use of this combination is possible, but one should remember the possibility of adverse reactions from the central nervous system.
Zidovudine
: When used simultaneously with fluconazole, an increase in Cmax and AUC of zidovudine is observed by 84% and 74%, respectively. This effect is probably due to a decrease in the metabolism of the latter to its main metabolite. Before and after therapy with fluconazole at a dose of 200 mg/day for 15 days in patients with AIDS and ARC (AIDS-related complex), a significant increase in the AUC of zidovudine (20%) was found.
When zidovudine was administered to HIV-infected patients at a dose of 200 mg every 8 hours for 7 days in combination with fluconazole at a dose of 400 mg/day or without it with an interval of 21 days between the two regimens, a significant increase in the AUC of zidovudine (74%) was found at simultaneous use with fluconazole. Patients receiving this combination should be monitored for side effects of zidovudine.
Voriconazole (inhibitor of CYP2C9, CYP2C19 and CYP3A4 isoenzymes):
simultaneous use of voriconazole (400 mg 2 times a day on the first day, then 200 mg 2 times a day for 2.5 days) and fluconazole (400 mg on the first day, then 200 mg per day for 4 days) leads to to increase the concentration and AUC of voriconazole by 57% and 79%, respectively. It has been shown that this effect persists when the dose is reduced and/or the frequency of administration of any of the drugs is reduced. Concomitant use of voriconazole and fluconazole is not recommended.
Studies of the interaction of oral forms of fluconazole when taken simultaneously with food, cimetidine, antacids, as well as after total body irradiation in preparation for bone marrow transplantation showed that these factors do not have a clinically significant effect on the absorption of fluconazole.
Tofacitinib
: The exposure of tofacitinib is increased when it is co-administered with drugs that are both moderate inhibitors of the CYP3A4 isoenzyme and strong inhibitors of the CYP2C19 isoenzyme (for example, fluconazole). Dose adjustment of tofacitinib may be necessary. The listed interactions were established with repeated use of fluconazole; There are no known drug interactions resulting from a single dose of fluconazole.
Ivacaftor
When coadministered with ivacaftor, a cystic fibrosis transmembrane conductance regulator (CFTR) stimulator, there was a 3-fold increase in ivacaftor exposure and a 1.9-fold increase in hydroxylmethyl-ivacaftor (M1) exposure. For patients concomitantly receiving moderate CYP3A inhibitors such as fluconazole and erythromycin, a dose reduction of ivacaftor to 150 mg once daily is recommended.
Doctors should note that interactions with other drugs have not been specifically studied, but are possible.
Treatment
First of all, when treating candidal stomatitis, you need to determine and eliminate the cause, adhere to the principles of proper nutrition and strengthen the body's immune system. And, of course, it is necessary to monitor oral hygiene. In most cases, this is quite enough for recovery.
If the disease is in a moderate or severe stage, the doctor often prescribes special medications for oral administration and antifungal ointments. Taking medications continues until the symptoms in the oral cavity are completely eliminated, in order to exclude possible relapses.
Treatment of mild forms of candidal stomatitis is carried out at home and does not require special conditions. Antifungal elixirs and lozenges are used. On average, the treatment course takes no more than two weeks.
More severe forms are characterized by the fact that the infection enters the digestive tract. Antifungal drugs are used to combat the disease. The course of treatment lasts from 2 to 4 weeks.
Recurrent forms of candidal stomatitis require much more time and money. Treatment is carried out until all symptoms disappear completely. Various antifungal agents are used.
Treatment of candidal stomatitis must be combined with a special diet. First of all, you should stop eating foods that are rich in starch and various confectionery products, minimize the consumption of cereals, baked goods, potatoes, etc.
When treating candidal stomatitis, other concomitant diseases should be eliminated, in particular:
- Caries;
- Periodontal disease;
- Chronic diseases of internal organs.
Pharmacodynamics
Antifungal agent. A triazole derivative exhibits an antifungal effect by blocking the biosynthesis of ergosterol in the cell membrane of fungi. The “target” for the action of the drug is the enzyme 14-α-demethylase.
14-α-demethylase is part of a group of enzymes known collectively as cytochrome P450. All enzymes of the cytochrome P450 group contain hematinic iron-containing pigment. Fluconazole binds to the iron atom of the hematin group and inactivates 14-α-demethylase, which leads to disruption of ergosterol synthesis and accumulation of lanosterol and other sterols. Their inclusion in the membrane instead of ergosterol significantly disrupts the structure and function of the fungal cell membrane.
A decrease in ergosterol synthesis, as well as the accumulation of 14α-methylsterols, destroys the tightly packed acyl chains of fungal membrane phospholipids. Destabilization of the fungal membrane leads to dysfunction of membrane enzymes, including those involved in the electron transport chain, and ultimately to cell death.
Used for systemic mycoses: candidiasis, cryptococcosis, blastomycosis, histoplasmosis, coccidioidomycosis, as well as dermatomycosis. The relatively low toxic profile and high penetration into the cerebrospinal fluid make fluconazole the drug of choice for systemic candidiasis and cryptococcal meningitis. Because of complications associated with intrathecal amphotericin B, fluconazole is the first-line drug for coccidioidal meningitis. Although fluconazole is active against the causative agents of blastomycosis, histoplasmosis, and sporotrichosis, it is inferior in effectiveness against the causative agents of these infections to itraconazole. Fluconazole is not effective against aspergillosis.
Prevention
To ensure that candidal stomatitis never bothers you, you should follow a few simple but very useful rules:
- Follow basic hygiene rules. Namely: wash your hands well with soap, especially when returning from the street, brush your teeth, use dental floss at least once a day, and also rinse your mouth with special means.
- You should definitely buy a new toothbrush. For those who have dentures, it is recommended to place them in a disinfectant solution overnight.
- After consuming liquid antibiotics, you should immediately rinse your mouth with water.
- When using spray corticosteroid drugs, you should wear a special nozzle.
Use during pregnancy and lactation
There have been no adequate and controlled studies of the use of fluconazole in pregnant women. Several cases of multiple congenital defects have been described in newborns whose mothers received high-dose fluconazole therapy (400-800 mg/day) for most or all of the first trimester. The following developmental disorders were noted: brachycephaly, impaired development of the facial part of the skull, impaired formation of the cranial vault, cleft palate, curvature of the femurs, thinning and elongation of the ribs, arthrogryposis and congenital heart defects. Currently, there is no evidence of a connection between the listed congenital anomalies and the use of low doses of fluconazole (150 mg once for the treatment of vulvovaginal candidiasis) in the first trimester of pregnancy.
During pregnancy, the use of fluconazole should be avoided, except in cases of severe and potentially life-threatening fungal infections when the expected benefit of treatment to the mother outweighs the possible risk to the fetus. Women of childbearing age should use contraception.
Since the concentration of fluconazole in breast milk and plasma is the same, the use of the drug during breastfeeding is contraindicated.