Does your jaw click when chewing or when at rest? This is an alarming symptom that indicates certain pathologies of the dental system. It is imperative to consult a dentist, since wasting too much time can lead to inflammation of the joints, loss of teeth and other negative consequences that will have to be treated surgically.
What problems do 70% of dental patients face?
- jaw crunch
- difficulty opening
- pain and discomfort
- clicking sound when chewing
Unfortunately, more and more people are beginning to experience problems with the TMJ (temporomandibular joint) and seek help from a gnathologist. How does the joint work, what problems can arise and what needs to be done in order to protect the health of your teeth and the dental system as a whole.
There are three main problems associated with TMJ:
- Sound or clicking sound in one or both jaw joints
- Significant restriction in opening and closing the jaws
- Pain in the joint and area around it
This triad of symptoms follows each other, occurring one after the other. And in order to understand the essence of solving these problems, it is very important to know the structure of the joint itself.
Why do jaw joints click differently?
This depends on the nature of the disease. Here are the most common types of clicks:
- intense - a sound that is heard by others;
- clicks that only the patient hears when talking or chewing food;
- clicks in a calm state, when a person does not move the jaw at all;
- clicks that only a specialist can hear using special equipment. The person does not hear them.
Types of clicks, depending on the moments of playback:
- with the mouth wide open;
- when the mouth is slightly open;
- in a calm state;
- when chewing;
- when talking;
- when yawning;
- when the patient closes his mouth;
- when closing the jaws, etc.
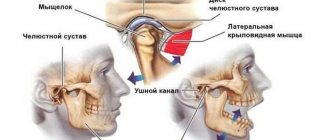
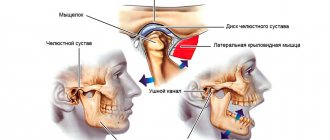
Structure of the TMJ (temporomandibular joint)
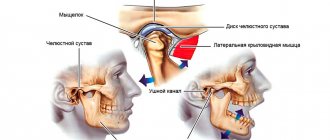
The temporomandibular joint consists of the following elements:
- head of the mandible
- mandibular fossa
- articular tubercle
- articular disc
- capsule and ligaments
The articular head is an ellipsoidal bone formation at the end of the condylar processes of the lower jaw.
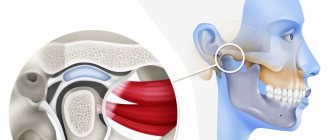
An articular disc is a biconcave plate consisting of coarse fibrous connective tissue. It has an oval shape. Located between the articular surfaces, it isolates the articular head from the mandibular fossa, dividing the joint cavity into two floors (upper and lower), the disc is fused at the edges with the joint capsule.
Preventive measures
The main preventive measure against the development of TMJ diseases is careful attention to the condition of the body as a whole.
Regarding the prevention of clicking in the jaw, experts recommend the following:
- treat dental diseases at the initial stages of their development;
- removed or damaged teeth should be immediately replaced with artificial analogues;
- After receiving an injury, immediately consult a doctor;
- treat ear, nose and throat diseases in a timely manner;
- Do not eat too hard and hard foods.
These simple tips will help you maintain healthy jaw joints for life.
The video provides additional information on the topic of the article.
What to do if your jaw starts to crack?
If, when opening the mouth, the patient hears a clicking sound, this means that the articular disc is deformed and displaced from its position to the side. The question is why did the disk "lose" its place and become misaligned? The TMJ has only one support - the bite, the teeth. Correct closure and uniform load on the teeth “save” our joint from the triad of symptoms mentioned above.
The next stage after a crunch or click, patients note difficulties in opening the mouth or problems in closing it.
The reason why such problems arise is due to the fact that the disc is not fixed “in its place”, it either jumps onto the condyle, then slides off it, and then at one point the jaw simply jams. The patient cannot open or close his mouth. At this moment, a protective reflex is triggered, the person begins to panic, the muscles work in an enhanced maximum mode to help the jaw return to its usual initial state, but such an effort, on the contrary, only leads to aggravation of the situation.
And now we are talking about the third stage, when pain is observed in the joint and around it.
The pain occurs as a result of the fact that the articular disc has become deformed and slipped, has ceased to share the space between the skull and the condyle, the bones simply begin to rub against each other, as a result, the head of the TMJ wears off and loses its shape.
Also, one of the causes of pain is that without articular cartilage, the nerves and blood vessels in the joint are compressed, hence the sharp pain that radiates to the head and temporal region, dizziness and nausea appear. The pain begins to cover all surrounding tissues, muscles and teeth. At this stage, patients may complain of hearing loss, tinnitus, and ear congestion.
Why does my jaw click when I open my mouth?
Most often, such clicking is caused by jaw arthritis. This pathology affects the cartilage layer of the joint or meniscus. Accordingly, the meniscus becomes thinner, the fibers become looser, and the cartilage can partially fuse with the articular head. As a rule, the clicks in this case are multiple, resembling a crunch.
The sound is formed as a result of the movement of the articular heads, which overcome the boundary in the form of folds of the cartilage disc. This crunch can be muffled, and therefore only audible to the person himself. Very often the jaw crunches when the mouth is opened sharply, when subluxation of the joint occurs. With some difficulties, but the jaw can be returned to its place. But sometimes this is impossible on your own - the patient is diagnosed with a dislocation, and here the help of a surgeon will be required.
TMJ dysfunction syndrome
This entire triad of symptoms is called “TMD syndrome (temporomandibular joint dysfunction). This syndrome is too difficult to treat; unfortunately, one doctor alone cannot cope with such a situation. A comprehensive treatment is required, in which doctors such as a gnathologist, orthopedist, orthodontist, and sometimes a surgeon will take part. That is why it is very important to consult a doctor with the first signs in order to prevent the disease in time.
How effective is therapeutic exercise?
After eliminating the causes of the disease, the doctor prescribes restorative exercises to the patient, or rather a set of exercises that will help improve the functionality of the masticatory muscles.
Joint exercises are performed after thermal preparation of muscle structures with a warm compress. The duration of the manipulation is no more than 10 minutes.
Good results can be achieved with the following exercises:
- Move your movable jaw forward and backward 10 times in each direction.
- Move your jaw first to the right and then to the left with your lips parted. Repeat at least 10 times.
- Press the chin area with your hand and try to forcefully lift your jaw up. The duration of the movement is at least 1 minute.
- Try pushing your jaw forward for 1 minute, pressing with your fingers on both sides of the chin.
Crunching jaw: how to treat and which doctor to contact
The first question that arises for people who are faced with crunching and discomfort in the jaw is what should be done, which doctor should they contact, should they do anything at all? It all depends on how long ago the jaw began to crunch, what caused this unpleasant phenomenon, whether the crunch is accompanied by other symptoms, and whether it limits the movement of the jaw. It is important that in no case should you self-medicate, which can aggravate the situation, and postpone a visit to the doctor.
Treatment of TMJ by our experienced gnathologists who:
- are able to carry out accurate diagnostics and apply their results in practice
- high-quality diagnostics using more than 50 parameters
- know how to treat so that the first result is noticeable within 7 days
- can prove their experience with successful results of more than 524 satisfied patients with TMJ problems
- quality treatment at prices in the residential area of Yasenevo
Treatment methods
The method of eliminating problems with TMJ directly depends on the causes of the development of the pathology and the characteristics of its course. In combination with therapeutic measures, the patient may be prescribed anti-inflammatory drugs, muscle relaxants, and anti-stress drugs.
In some cases, to eliminate the problem, they resort to the use of fixing orthopedic structures, such as splints, plates, and mouthguards.
In case of serious problems, joint surgery is performed in the Department of Maxillofacial Surgery. Today, doctors use a number of techniques for the surgical treatment of TMJ disorders.
Minimally invasive technique
The surgeon injects a special solution into the joint structure, which will help remove the affected hard tissue cells.
Also, the effect of the drug is aimed at smoothing cartilage tissue and normalizing the production of synovial fluid for rapid restoration of the joint.
The essence of the procedure is the elimination of inflammation and stimulation of fluid production in the joint. The technique is effective for mild disorders.
Jaw arthroscopy
Jaw arthroscopy is a minimally invasive procedure performed in maxillofacial surgery to treat damaged parts of the joint.
It is performed using a thin tube (arthroscope) that is inserted into the jawbone through a small hole in the soft tissue. A microscopic camera is attached to the device, which transmits a close-up image of the surgical field to the monitor.
Instruments for surgical procedures are inserted through the arthroscope. During the operation, the doctor may do the following:
- excise scars and thickened cartilage tissue;
- “model” the shape of the jaw bone;
- wash the joint and strengthen it;
- inject an anti-inflammatory agent into the area of inflammation.
After such an operation, the treated tissues are quickly restored.
Open operation
Open operations on the jaw bone are performed in case of serious traumatic injuries, the presence of a tumor and degenerative changes in the structure of hard tissues.
Of the existing methods of opening access to the joint, the Rauer incision is considered the most aesthetic. Although it is technically difficult to implement. The length of the incision, passing along the lower part of the zygomatic arch slightly short of the tragus of the ear, is about 3 cm.
The same incision is made from the end of the first cut perpendicularly downwards. As a result of using a scalpel, a triangular-shaped flap of soft tissue is obtained. It is retracted, part of the masticatory muscles is cut off from the zygomatic bone and free access to the joint is opened.
The procedure allows you to start regenerative processes.
Prosthetics – head replacement
The deformed area is replaced only after open surgery . During the manipulation, the head of the affected joint is completely replaced.
The correct distribution of the bone end parts is ensured by the laying of muscle and cartilaginous elements. The technique is used for advanced pathologies and disorders.
Retroalicular technique
The technique involves fixing the joint with special internal screws. The incision is made behind the ear. This approach is very convenient due to a good inspection of the required area.
After surgery, the joint can be loaded immediately, but only slightly.
The human jaw is a complex machine, and the problems that can arise are not limited to tooth decay, periodontal disease, malocclusions, or frenulum frenulums.
One of the most common diseases, along with those listed, are lesions of the temporomandibular joint (TMJ). Let's talk about how to understand that the jaw has suddenly stopped being friends with us, and what to do about it.
The temporomandibular joint is an extremely mobile paired joint that connects the base of the skull with the lower jaw: intra-articular cartilage is located between the surface of the head of the mandible and the articular surface of the temporal bone. Normally, joints are involved in all movable processes simultaneously.
Some symptoms of dysfunction or disease of the TMJ are observed in at least 40% of people - this is due to the fact that we rarely use which joint in the body more often. Yawning, chewing, speaking, chattering teeth when we are cold - all this requires a certain muscle tension and coordinated work of all parts of the TMJ.
Normally, a person moving his jaw should not feel any discomfort - any unpleasant sensation, sounds, pain will be a reason to consult a doctor.
Symptoms that you should pay close attention to:
- spasms of the facial and jaw muscles, pain;
- headache, dizziness, pain and pressure in the ears and eyes;
- uncharacteristic sounds when moving: clicking, crunching, grinding;
- jamming: the jaw seems to be stuck, cannot move, or, conversely, is actively moving to the side;
- sudden change in bite;
- enlarged lymph nodes.
The main causes of TMJ diseases:
- mechanical trauma - bruises, cracks, fractures of the jaw bones;
- Bruxism - with severe stress or excessive physical activity, a symptom of involuntary clenching of teeth occurs, grinding teeth in sleep. Such loads have a bad effect on the condition of the joint;
- metabolic disorders, endocrine system dysfunction;
- previous inflammatory processes in the joint, in particular complications after the flu;
- prolonged absence of teeth or prolonged use of incorrectly selected dentures;
- habits: one-sided chewing, holding the telephone receiver with the shoulder, etc.
Of the variety of TMJ dysfunctions, the most common are the following:
- ARTHRITIS . This is an inflammatory process that develops during injuries, local infections and allergic reactions. Accordingly, a distinction is made between traumatic arthritis, non-infectious and infectious. In the acute stage, the pain is severe and becomes even more intense with the slightest movement - it is impossible to open the mouth completely, the jaw shifts. The parotid areas become swollen and edema occurs. With chronic arthritis, pain becomes moderate and occurs spontaneously. The joint becomes stiff, the parotid area becomes sensitive.
Treatment is usually conservative. For all types of disease, immobilization is used for 2–3 days using a sling bandage and a semi-liquid diet. Further on the specifics: traumatic ones are treated with cold compresses, analgesics, physiotherapy, massage and myogymnastics; acute - non-steroidal anti-inflammatory drugs (NSAIDs) and chondoprotectors, physiotherapy. For chronic cases, in addition to medications, massage courses, physiotherapy and rational dentures are prescribed. In case of purulent arthritis, the surgeon performs an emergency opening and drainage of the joint cavity.
- ARTHROSIS . This is a dystrophic disease in which the relationships of the masticatory muscles are disrupted, as they are rebuilt to overcome occlusal obstacles, for example, with low-quality and poorly fixed dentures. In such cases, a situation may arise with the appearance of unnatural chewing - due to an unevenly distributed load, one part of the joint receives excessive pressure, the other - stretching; cracks appear in the articular cartilage and it becomes deformed; bone tissue undergoes osteoporosis. The complaints characteristic of arthritis include crunching and clicking, pain during inactivity, which can radiate to the palate, throat, tongue and even shoulder.
Balance treatment. In addition to the necessary pharmaceutical prescriptions (NSAIDs, chondoprotectors) and physiotherapy, the doctor does a lot of work to find and eliminate factors leading to imbalance in the functioning of the joint and uneven load: malocclusion, poor-quality dentures - any little thing, even replacing fillings and selective grinding can help to the patient. In the later stages of arthrosis, surgical intervention may be indicated - meniscectomy, resection of the head of the lower jaw, transplantation of the articular head or complete prosthetics.
- ANKYLOSIS . It can often be a consequence of advanced arthrosis. This is a fusion of joint surfaces - fibrous (more often in adults) or bone (more often in children): the joint is partially or completely deprived of mobility in the horizontal plane. Ankylosis can appear due to chronic joint diseases, osteomyelitis, fractures, or untimely treated purulent arthritis. In addition to the fact that the jaw hardly moves, the shape of the face changes, pain and clicking occur, and the muscles quickly tire.
Treatment of fibrous ankylosis in the initial stages can be conservative - physiotherapy, intra-articular injections of hydrocortisone, redressing (separating the jaws, carried out under anesthesia; dissection of adhesions inside the joint). In complex cases and with bone ankylosis, only surgical intervention under conduction anesthesia or general anesthesia is indicated to restore the functions of the jaw and eliminate deformities of the facial bones. The surgeon performs osteotomy with arthroplasty and plastic surgery of the lower jaw using a bone autograft. During the rehabilitation period, in order to avoid relapse, the lower jaw is fixed with special splints. Patients often require mentoplasty in the future.
- DISLOCATION . The result of a violation of the position of the jaws relative to each other, usually manifests itself in muscle disorders. Many different conditions fall into this category: hypermobility of the head of the mandible, sprains and TMJ capsules. In case of subluxation or dislocation of the head of the lower jaw, in the first case the patient can restore the blocked joint himself, in the second case the help of a doctor is required.
Treated by reduction. The surgeon returns the articular heads to the articular capsules, then the lower jaw is fixed with a bandage for a period of 5–7 days, and the patient is prescribed a gentle diet. The main condition for successful rehabilitation is the time when the patient presented with the problem, since old dislocations are quite difficult to correct. In these cases, the surgeon may prescribe resection of the heads of the lower jaw.
- LESIONS OF THE ARTICULAR DISC : displacement with reduction (the disc clicks into place if you open your mouth); displacement without reduction, in which it is impossible to fully open the mouth; displacement without reduction and without restrictions. In this case, patients complain of muscle pain and tension, strange sounds, and limited mobility. Also, patients with an already established diagnosis may have no complaints at all. This condition must be monitored as it can subsequently lead to more complex lesions of the disc and the TMJ as a whole.
The condition of the jaw is very important for a person’s overall health - the inability to eat well leads to dysfunction of other organs and systems of the body, and psychological stress from ringing in the ears and clicking joints will only aggravate the problem. If you notice at least one of the symptoms, consult a doctor and solve the problem at an early stage.
Pain after dental implantation, tooth implant hurts
During dental implantation, the trigeminal nerve and its branches, the alveolar nerve plexus, may be damaged as a result of:
- Screwing the implant into the canal where the trigeminal nerve or its branches lies;
- Inflammation in the implant area (infection and/or implant rejection).
Some pain during the implant healing process is normal. If the pain after dental implantation lasts too long, is very severe, or is accompanied by numbness of the lip or cheek, we can check the condition of the trigeminal nerve using electromyography and a neurological examination based on the characteristic loss of facial sensitivity and the spread of pain along the trigeminal nerve system.
The rejection reaction and inflammatory processes in the implant area are usually clearly visible with CORRECT X-ray examination and computed tomography.
Implants in the lower and upper jaw. Pain after dental implantation
There may be direct pressure from the implant on the nerve or inflammation in the implant area with tissue swelling, edema and subsequent pressure on the nerve.