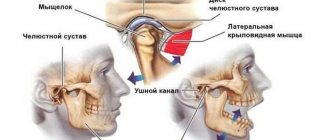
If a person feels pain in the jaw, radiating to the ear and temple, we may be talking about arthritis of the mandibular joint. The pathology is not just painful, but also dangerous. If not diagnosed in a timely manner, it can lead to severe complications, including paralysis of the facial nerves. Therefore, the first thing to do when such symptoms appear is to consult a specialist. In 10-18% of cases, diagnosis and treatment of TMJ arthritis is the responsibility of dentists and occurs in people from 25 to 45 years old.
Causes of temporomandibular joint arthritis
Arthritis does not show pronounced symptoms immediately; its development can be asymptomatic for a long time or with minor pain. Out of habit, a person reacts to pain by taking painkillers, which only makes the situation worse. Anesthetics relieve symptoms, but do not remove the cause. The disease “takes over” more and more healthy tissue and, as a result, instead of treatment, the patient receives disability. Let's figure out why TMJ arthritis can develop.
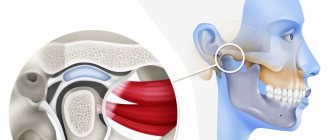
- 1. Mechanical injury. Impact, the habit of clenching teeth tightly, and active chewing of hard food can lead to damage to one or more components of the joint. Articular tissues respond to damage with pain and dilation of blood vessels. Simply put, blood enters from the vessels directly into the tissue, causing swelling, inflammation, and, if treatment is delayed, suppuration.
- 2. Infection. The inflammatory process develops as a result of pathogenic microorganisms entering the joint through the blood or through direct and contact routes. The direct route of infection involves inflammation of the TMJ as a result of an open wound (knife or gunshot wound). If microorganisms have penetrated into the cartilage from infected muscle or bone tissues, then the pathology of transmission is called contact. All diseases of the oral cavity (as well as ear, nose and throat) can lead to arthritis of the temporomandibular joint through the hematogenous route, through the blood.
- 3. Systemic inflammation. Some pathologies of an inflammatory nature (herpes, hepatitis, mycoplasmosis, chlamydia, lupus), if not treated in a timely manner, affect connective tissue throughout the body.
Risk factors
Main reasons:
- Injury. The cause in this case may be a bruise, a blow, or a sudden opening of the mouth.
- Infection of ENT organs. Arthritis of the maxillary joint can be caused by streptococci, chlamydia or tuberculosis.
- Osteomyelitis.
- Untreated caries.
- Periodontal diseases.
- Otitis.
In addition, the following conditions may also affect the development of jaw arthritis:
- Gout.
- Systemic lupus erythematosus.
- Diabetes.
- Thyroid diseases.
- Rheumatoid and reactive arthritis.
Sometimes inflammation can be caused by general hypothermia of the body.
Symptoms of TMJ arthritis
Depending on the cause of the disease and the nature of the inflammation, arthritis manifests itself with the following symptoms:
- sharp pain when moving the jaw. Increases in opening/closing of the mouth, strongly radiates to the temple, back of the head, tongue;
- when you try to open your mouth wider, the jaw moves to the side;
- inability to close teeth tightly;
- hearing loss, dizziness;
- crunching when moving the jaw.
If at least 2 signs are detected, we recommend that you do not wait for the consequences, but contact the dentist. Correct diagnosis ensures the necessary treatment and recovery in a short time. In the later stages, the dentist will not help. And treatment will cost much more.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Comprehensive treatment of TMJ
When the doctor has determined the cause of the joint pathology, or causes, he determines the patient's readiness for a comprehensive treatment plan. In addition to the orthodontist, an osteopath or chiropractor may be involved, or even an orthopedist if more complex correction of the musculoskeletal system is required.
The patient should be aware that it is possible to straighten the jaw using a splint or splint, but this will not solve the problem of malocclusion. Orthodontic treatment will be required to correct the bite. If you have already had orthodontic treatment before, then it is more difficult to decide on repeated treatment.
Therefore, first the problem with the joint is solved using a splint or joint splint, then bite correction is carried out, and, if necessary, prosthetics. In parallel, work is underway with an osteopath to restore the muscular corset of the back and neck.
It happens that a patient refuses treatment with braces after the problem with the joint has been resolved. In this case, we warn him about the need to wear a joint splint constantly in order to avoid the recurrence of old problems with the TMJ. After all, a relapse can happen quite quickly due to stress.
How is arthritis of the lower jaw joint treated?
If pain and stiffness symptoms occur, it is necessary to ensure the TMJ rests. Move your jaw less, take only liquid food, and do not clench your teeth tightly. Visiting the dentist is a must. Only a qualified specialist will be able to tell why the joint is inflamed and prescribe the optimal treatment. Diagnosis consists of blood tests and x-rays. Depending on the situation, we recommend:
- cold compresses;
- drug treatment (broad-spectrum antibiotics, painkillers);
- physiotherapy.
If conservative treatment is ineffective, surgery will be prescribed. Traditional methods of treatment are not only ineffective for arthritis of the temporomandibular joint, they are often dangerous. Decoctions, compresses and ointments according to grandmother's recipes can relieve pain and swelling, but they will not remove the cause of the disease; moreover, some of them can inflame the joint even more. The consequences are impossible to predict, especially with the hematogenous method of infection of the joint. 20% of patients who treated themselves develop joint paralysis.
How does the disease manifest itself?
- pain in the jaw area, radiating to other parts of the face and intensifying when opening the mouth;
- restrictions in joint movement;
- dizziness, chills;
- general weakness;
- increased body temperature (may be over 38 degrees);
- sleep problems;
- jaw clicks;
- joint pain on palpation;
- deformation of the oval of the face due to the fact that the chin begins to move to the side;
- hearing problems.
The important thing is that with arthritis of the jaw joint, purulent inflammation can begin! In such a situation, the joint turns red, swells and becomes very sensitive. A compaction is felt in the area of the mandibular joint. The skin changes its color, speech is impaired, and the process of chewing food becomes difficult.
Symptoms of arthrosis of the jaw in dynamics
Morning stiffness in a joint, crunching and clicking do not cause concern in a person at first. The problem worsens when dull pain appears during chewing, and when reactive synovitis occurs, constant aching pain occurs. Symptoms worsen in the evening, in cold weather and with excessive exercise.
After a few months, a person involuntarily notices limited movement of the lower jaw and its stiffness. But this is far from the limit. If the disease is not treated, the following are possible:
- displacement of the jaw to the problematic side and, as a result, asymmetry;
- numbness of the affected area;
- headache;
- eye problems;
- hearing loss, etc.
Often, with arthrosis of the jaw, patients mistakenly turn to an ENT or ophthalmologist: the pain radiates to the ear or eye
The most likely causes of arthrosis of the jaw joint
Before trying to determine the causes of arthrosis of the jaw joint, it is necessary to understand that the pathology is primarily multifactorial, which makes it likely that several prerequisites for its development exist at once.
The group of common causes of arthrosis of the jaw joint usually includes genetic factors and various diseases. Among the local ones there are:
- the presence of a chronic form of arthritis;
- partial absence of molars;
- pathologies of dental tissues (abrasion, etc.);
- violation of prosthetic technology/placement of fillings, especially on chewing surfaces;
- injuries and surgical interventions.
In addition, it is worth noting that among women, the risks of the causes of arthrosis of the jaw joint include a natural decrease and instability of hormonal levels, on which the effectiveness of metabolic processes occurring in tissues largely depends.
A combination of factors provokes difficulties in treatment.
Treatment method for TMJ dysfunction
1. Diagnosis of TMJ dysfunction.
- When diagnosing a joint in the clinic, a series of measurements and tests are carried out, all sensations in the joint area are recorded (discomfort, clicks, pain, deviation of the jaw when opening and closing), the difference in sensations in the right and left joint.
- The orthodontist also takes impressions of the jaws and takes photographs of the face and intraoral photographs, and also performs three-dimensional computed tomography of the face (3D CT); if necessary, the doctor can give a referral for an additional study - magnetic resonance imaging of the TMJ (MRI).
- Often, the orthodontist, in addition to manual functional analysis, conducts a visual assessment of: posture, symmetry of the shoulder girdle, shoulder blades, hip bone structures, etc., performs the necessary tests and photographs. Based on the results, it is possible to schedule a consultation with an osteopath or chiropractor to jointly manage the patient. Related specialists (orthopedist, surgeon, periodontist) can also be involved in drawing up a treatment plan.
What exercises are prescribed to patients to normalize the work and relax the masticatory muscles?
Exercise No. 1
Draw a vertical line on the mirror with a marker, stand opposite so that the line divides your face into the right and left halves, place your fingers on the area of the articular heads, lift your tongue up and back, open and close your mouth along the line (it may not work right away), 2-3 times /day 30 repetitions. There is no need to open your mouth wide (a comfortable width), the main thing is symmetrically (so that the jaw does not “move” in any direction). If there is a click, open until it clicks.
Exercise No. 2 (cycle)
Do it whenever possible, for example, in front of the TV, at the computer, or in a traffic jam while driving. Open and close your mouth without closing your teeth for 30 seconds, then alternately reach your right and left cheeks with your tongue for 30 seconds. Open - close your mouth again, then for 30 seconds move your tongue in a circle inside the vestibule (behind the lips), first in one direction, then in the other direction (clockwise - counterclockwise), open again - close your mouth, etc.. For this a half-hour cycle, the teeth should not touch, the lips should be closed. If you want to close your mouth or swallow, place your tongue between your teeth. Repeat the cycle for 20-30 minutes 2-3 times/day
Classification
Based on the results of an X-ray examination, in accordance with the diagnosed changes, it is customary to distinguish between two types of arthrosis:
- sclerosing - changes suggest sclerotic changes in bone surfaces, accompanied by a significant narrowing of the gap between the heads of the bones;
- deforming – there is a significant loss of texture and inherent forms of bone tissue, as well as a significant proliferation of osteophytes.
According to their origin, there are two types of pathology:
- primary – forms independently, without previous diseases/damages, mainly in old age;
- secondary - has a close connection with previous trauma, inflammation or metabolic disorders.
Treatment tactics for arthrosis of the mandibular joint
Ideally, starting treatment for TMJ arthrosis is optimal at stages 1 or 2. First of all, it is important to exclude risk factors - excessive mechanical stress, prolonged opening of the mouth, for example at a dentist appointment, etc. Therapy should be continuous and comprehensive - individual orthopedic measures or diet are not enough.
- Diet. To reduce the mechanical load, the patient is recommended to switch to soft foods, and during an exacerbation - to purees, juices, cereals and fermented milk products.
- Daily routine and lifestyle. It is very important to get enough sleep and limit stress, since any stress causes you to reflexively clench your teeth, which can aggravate the situation.
- Dentist consultation. Provoking factors include dental defects, missing teeth, and malocclusion. These problems are easily solved today, and patients with jaw arthrosis are primarily referred to the dentist and orthodontist.
A dentist and an orthopedist always take part in the treatment of jaw arthrosis.
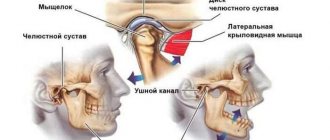
Pathogenesis
The study of the mechanisms of development of pathology allowed us to come to conclusions about their progression associated with a lack of physiological endurance of the joint.
The resulting injuries and the appearance of inflammation lead to improper distribution or excessive load on the tissue, which causes disruption of the synchronization of the joints, causing loss of functionality of the muscular system. The result of the development of such unpleasant processes is a disruption of the nutrition of cartilage tissue, as well as a gradual loss of their elasticity, which inevitably leads to destruction.
Simultaneously with all of the above, serious transformations of bone tissue develop, which provokes the formation of growths that modify the elements of the joint: the head of the lower jaw changes shape, and signs of osteoporosis are visible.
As a result of the uncontrolled course of pathological processes, severe deformation and serious disruption of the tissue structure occur.
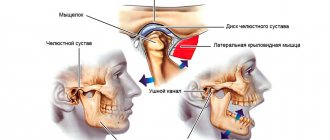
Stages of development of arthrosis of the jaw joint
Regardless of the type/type of disease present, several stages of its development are determined.
Stage I
Diagnosed as joint instability.
Based on the results of the X-ray examination, a moderate and uneven, but clearly noticeable narrowing of the joint space is observed, which is caused by the activation of degenerative-dystrophic changes in cartilage tissue.
Stage II
The clinical aspect assumes full compliance with the general symptomatic picture.
X-ray examination shows that all the changes that occur are characterized by the presence of sclerosis and ossification of the lower jaw.
Stage III
The active progression of pathological processes causes a limitation in the functionality of the jaw.
X-ray examination reveals signs of complete degeneration of cartilage tissue, as well as total sclerosis of the surfaces of articular tissues. In addition, the presence of multiple bone growths, as well as noticeable transformations, is noted.
IV stage
If left untreated, degenerative processes in combination with various types of neoplasms cause fibrous ankylosis of the affected joint.
Causes of TMJ damage
can be different - infectious, traumatic, most scientists agree that the main cause is a psycho-social factor. That is, during stress, the muscles of the maxillofacial and chewing apparatus become overstrained, which leads to tight clenching of the jaws - bruxism, especially at night. This leads to facial headaches and neck pain, excessive tooth wear and sensitivity.
Other possible causes of TMJ disorders include:
- joint injury,
- decreased bite height due to loss of teeth, especially chewing ones,
- excessive loads when playing athletic sports, malocclusion.
Most people do not notice the pathological changes occurring to them in the initial stages of this disease and consult a doctor when significant changes have already occurred. Therefore, it is very important to regularly visit the dentist in order to identify this problem at the initial stage, when treatment does not yet require surgical intervention. Treatment of TMJ diseases should be comprehensive with the involvement of specialists: dentists, neurologists, osteopaths, psychologists.
Diagnostic methods
Medical diagnosis is carried out using x-ray examination, the results of which make it possible to determine the type and stage of changes occurring.
In addition to radiographic diagnostics, in order to make the most accurate diagnosis, laboratory tests of urine and blood, as well as additional instrumental research methods, can be used.
Self-diagnosis reminder
Changes such as:
- the appearance of crunching/clicking sounds when performing various types of movements;
- decreased jaw mobility, manifested when eating, yawning, etc.;
- hearing impairment;
- decreased visual ability;
- pain of a pressing or bursting type, localized mainly in the temporal or parotid-masticatory region of the head;
- periodic convulsions accompanied by painful sensations;
- dysfunction of the vestibular apparatus;
- increased fatigue when chewing food, difficulty eating solid foods;
- partial loss of facial expression;
- numbness of the skin and mucous membranes in the area of the affected joint.
Prevention
Preventive measures require the fulfillment of such conditions as:
- maintaining proper and at the same time maximally balanced nutrition;
- optimization of the patient’s motor activity;
- rejection of bad habits;
- ensuring the proper level of oral hygiene;
- systematic attendance at preventive medical examinations.
Do not delay the treatment of arthrosis of the jaw joint, because in the first stages the disease is treatable, which allows us to talk about the complete restoration of jaw functionality.