The temporomandibular joint is a complex paired anatomical formation that provides horizontal and vertical movement of the lower jaw relative to the lower jaw. The load on the joint is determined not only by the quality of the food that needs to be chewed, but also by the condition of the dental system. The condition of the temporomandibular joint (TMJ) in turn affects our well-being and overall health.
According to data provided in the reports of the World Health Organization for 2022, musculo-articular dysfunction of the TMJ is detected in approximately every second person aged 20 to 50 years. And these are only those cases that are recorded in medical documentation. A fairly large number of people do not associate persistent headaches, clicking in the joints when chewing, difficulty opening the mouth with a painful condition of TMJ and are in no hurry to seek medical help.
Often, the pathology of the temporomandibular joint is detected during an examination performed for another reason, for example, in preparation for prosthetics. At the same time, the variants of joint diseases can be very different from dysfunctional syndrome to habitual joint dislocation.
Structure and functions of the temporomandibular joint
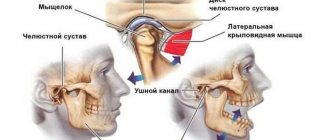
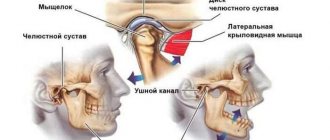
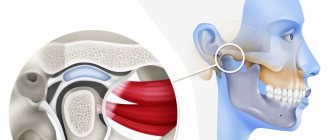
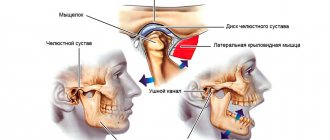
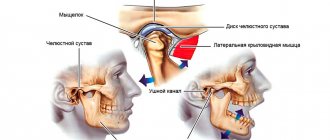
The joint is formed by the head of the horn of the lower jaw and the articular surface (fossa) of the temporal bone. Between these bone formations there is a fibrous intra-articular disc, which is fused on all sides with the joint capsule. Ligaments and muscles help keep the joint in the correct position. They limit the range of motion in the joint. Attempting to exceed this functional limitation causes pain and prevents damage to the TMJ.
The main function of the joint is to ensure movement of the lower jaw in three directions:
- vertical: opening and closing the mouth;
- horizontal: lateral displacements of the lower jaw relative to the upper;
- sagittal: movement of the lower jaw back and forth relative to the upper.
The combination of movements of one jaw relative to the other allows us to chew, speak, and express emotions through facial expressions.
Indications for surgery for osteoarthritis
The most common indication is severe pain and/or dysfunction of the TMJ of articular origin, which is aggravated by activity of the lower jaw. The more severe the pain and dysfunction, the better the prognosis for surgical intervention. The lack of effectiveness of arthrocentesis (sampling fluid from the joint) also became an indication for further surgical treatment. This low effectiveness of the procedure is explained by adhesions, which, in the absence of bone deformation, are not visible on an x-ray.
Causes of dysfunction of the masticatory joints
A gnathologist specializes in the diagnosis and treatment of TMJ diseases. In fact, this is a dentist with a narrow specialization. Factors that can lead to temporomandibular joint disease include:
- vascular pathology, which leads to impaired blood supply to the joint;
- increased tone of the muscles of the face and neck (increased tone, spasms);
- violation of occlusion;
- manifestations of psychosomatics.
Occlusion disorders underlie the largest number of cases of TMJ disease. Normally, the antagonist teeth of the upper and lower jaws contact their chewing surfaces in a certain way. The cusps and depressions on the upper surface of the antagonist teeth should contact according to the “pestle and mortar” principle. If the teeth on the jaw are positioned incorrectly and their correct contact is impaired, compensatory mechanisms are activated. In particular, the tone of the chewing muscles changes and the lower jaw shifts in such a way as to achieve full contact of all chewing surfaces of the teeth.
This displacement eliminates the occlusal obstacle, but creates additional stress on the temporomandibular joint. Habitual displacement of the jaw over time leads to damage to the anatomical structures of the joint. Increased tone of the masticatory muscles provokes hemodynamic disturbances in the TMJ area, which does not contribute to rapid regeneration.
If the cause of unpleasant symptoms in the TMJ area is a violation of occlusion, a gnathologist may recommend orthodontic treatment. This is the only way to get rid of the problem, since if the teeth are incorrectly positioned on the jaw, only symptomatic treatment of TMJ problems can be carried out, which will only lead to a temporary improvement in the condition.
Causes
Risk factors for developing osteoarthritis:
- people aged 40-60 years;
- injuries;
- bite defects;
- partial or complete loss of teeth;
- genetic predisposition;
- infectious processes of the ears.
It is difficult to determine the exact cause of the development of the disease, since the cause may be minor injuries that are left unattended.
Pathology can occur in adolescents with rapid growth, which is associated with anatomical features and accelerated growth of bone tissue against the background of underdevelopment of cartilage and muscles. Joint deformity can be diagnosed due to a lack of vitamins and an improper diet. If the body does not receive sufficient trace elements, this leads to deterioration of the cartilage.
Intense load on weakened temporomandibular muscles entails various microtraumas, the consequences of which are difficult to predict.
Symptoms and prevention of TMJ dysfunction
Pain in the masticatory joint is an extremely rare occurrence. In this regard, patients rarely associate the existing pathological manifestations with the condition of the TMJ. Let's see what symptoms you need to make an appointment with a gnathologist:
- Headache. There are a great many causes of headaches, but the “contribution” of the temporomandibular joint is most often “forgotten” by specialists. Elimination of TMJ pathology often relieves a person of headaches.
- Clicking in the joint. The characteristic sound when opening the mouth is a consequence of dislocation or subluxation of the masticatory joint, which usually resets on its own.
- Limitation of mouth opening. This may be a consequence of swelling of the joint tissue as a result of the development of an inflammatory process or dislocation of the joint.
- Pathological abrasion of tooth enamel.
Measures to prevent the development of TMJ dysfunction include regular visits to the dentist, rational prosthetics, timely treatment and restoration of damaged teeth, and orthodontic treatment as indicated.
Clinical picture
Symptoms primarily depend on the stage of development of arthrosis. The main symptom is a constant dull aching pain. When the jaw moves, the joint begins to crunch and click.
In addition, the patient may feel stiffness in the movement of the joint (most often manifests itself after sleep). The pain occurs when eating, so you have to chew on only one side.
In advanced cases, the patient has great difficulty opening his mouth at all. The jaw moves to the side, the asymmetry of the face is disrupted. To avoid irreversible consequences, it is necessary to treat the disease at an early stage.
Diagnostics
In order to make a diagnosis, the doctor conducts an examination according to the following scheme:
- Questioning the patient. Of interest to the specialist are complaints, conditions for the appearance of unpleasant symptoms, duration of the disease, previous treatment and its effectiveness.
- External examination and palpation. The gnathologist examines the patient’s face, paying attention to the area where the TMJ is located. By feeling the joints, you can get an idea of its structure and the state of its tissues.
- Dental examination. Anomalies of occlusion and the degree of their severity are identified.
- X-ray examination. The photographs show the bone formations that form the joint. By their relative position one can determine the presence of dislocations and subluxations, and by the thickness of the joint space one can judge the condition of the cartilaginous disc.
Treatment of TMJ: what is effective?
Modern medicine gives preference to organ-preserving, atraumatic and minimally invasive methods of therapy. If there is no effect from conservative treatment, taking into account the severity of the TMJ pathology, surgery may be prescribed.
Doctors at the Sechenov University Clinic help improve the quality of life and relieve clinical manifestations of functional disorders of the jaw joint by performing the following manipulations:
- Installation of special caps or splints. This helps to level out jaw closure disorders and helps correct the bite.
- Conducting pharmacotherapy. The patient is prescribed muscle relaxants (Mydocalm, Kalmirex, Tizalud, Sirdalud) intramuscularly and/or orally, psychotropic drugs (Fluoxetine), painkillers and anti-inflammatory drugs from the NSAID group (Nimesil, Dexalgin, Ketanov, Ketonal), chondroprotectors, calcium preparations, etc.
- Intra-articular injections. Patients are injected with Botox or its analogues in this way. solution, sodium hyaluronate. This helps to relax the masticatory muscles, move the articular disc to its normal position, and replace synovial fluid.
- Physiotherapy for TMJ. This can be phonophoresis, for example, with hydrocortisone, treatment with currents of various amplitudes and strengths, myogymnastics. These methods help relieve pain, swelling, inflammation, and muscle spasms.
- Surgical intervention. It is a last resort, but effective and final. Chondroplasty of the TMJ disc and the head of the lower jaw joint is performed. Sometimes suturing of the intra-articular ligaments and capsule is required.
The level of diagnostic and therapeutic measures in the clinics of Sechenov University can be considered unprecedentedly high. Almost no one can repeat what they can do here outside the center, since they either do not have the appropriate training or equipment.
Treatment
A gnathologist can carry out treatment either independently or with the involvement of specialists from other fields. This is especially true when the cause of the development of TMJ pathology has been identified and can be eliminated. The help of an orthodontist is necessary for patients with malocclusion. Wearing a brace system or aligners to correct occlusion has a beneficial effect on the condition of the entire dental system.
Detection of arthrosis or ankylosis of the temporomandibular joint also requires the involvement of specialized specialists. The doctor's specialty will be determined by the cause of the development of degenerative-dystrophic processes in the tissues of the TMJ. Metabolic disorders, injuries, infections will require additional examination and the development of an individual treatment plan.
Surgical treatment of TMD
Surgical intervention in the treatment of TMD does not play a major, but very important role. Surgery is indicated for approximately 5% of patients suffering from TMD. Moreover, the range of surgical interventions is very wide. Despite the many supporters of each individual surgical method, there are currently no strict clinical data substantiating the indications for a specific operation in a specific clinical case. Therefore, when deciding on any surgical intervention, the doctor uses criteria to assess the stability of the patient's condition.
First aid
A joint dislocation or subluxation that occurs for the first time can cause severe pain. Joint dysfunction can also cause pain of the same intensity. Regardless of the cause of the discomfort, you must do the following:
- provide rest to the joint: do not eat, talk as little as possible;
- take a pain reliever;
- Consult a doctor as soon as possible and undergo the necessary examination.
Experts categorically do not recommend heating a sore joint if the cause of the pain is unknown. In case of dysfunction, heat exposure can lead to some relief of the condition, but in case of dislocation, on the contrary, it will cause harm. Under the influence of heat, blood flow to the tissue increases, which contributes to the development of edema and makes reduction difficult. Thus, when trying to help yourself or a loved one, you can unknowingly cause serious harm.
Non-surgical treatment of TMD
Nonsurgical treatments for painful and dysfunctional TMD include patient education, joint stress reduction, medications, and physical therapy. Of course, the patient cannot control nighttime chewing activity, which is precisely the main source of excess load on the TMJ. To control this activity and reduce the load on the joint, various occlusal devices (for example, mouthguards) are used. According to research, they can reduce the load on the TMJ when clenching teeth in 82% of patients. During the daytime, the load on the joint is reduced by increasing the patient’s attention to his condition, switching to soft foods, and taking anti-inflammatory painkillers. A physical therapist can teach the patient specific exercises to increase mobility in the TMJ and relieve pain and stress on the joint.
Treatment of TMJ arthrosis
If TMJ arthrosis is diagnosed, treatment is carried out by an orthopedist. Only a modern approach and comprehensive procedures will help you quickly get rid of the disease. At the first stage, the specialist will determine the main reasons that resulted in overload of the jaw joint. Based on these data, an effective treatment method will be determined.
The basis of successful treatment is the primary elimination of factors that result in joint overload and the development of TMJ arthrosis. To immobilize the jaw, doctors use a set of orthopedic measures.
Next, the doctor grinds the teeth, which helps normalize the occlusion. Normalization of occlusion is necessary for proper contact between teeth in order to reduce their wear, remove pressure on the joint and ensure proper chewing of food and speaking. If grinding the teeth alone is not enough, doctors make and subsequently install dental crowns; in severe cases, it may be necessary to install dentures.
For dental anomalies, as a result of which tooth wear becomes pathological and the interalveolar height decreases, the treatment is long-term and consists of wearing a special mouth guard for 2-4 months.
After eliminating all dental anomalies, including correcting the bite and installing dentures or crowns, the specialist prescribes a set of physiological exercises that will help normalize the chewing ability of the jaw. Quite often, during physiotherapy, electrophoresis, mud treatment, paraffin therapy, massage, etc. are prescribed. The maximum effect is obtained by carrying out such procedures comprehensively. After the treatment has been completed and the acute pain has gone, the patient remains under constant supervision by a specialist for 1 year (minimum).
Diagnosis of TMJ pathologies
The initial examination begins with a detailed analysis of the patient’s complaints, collection of a detailed history and external examination. The doctor pays attention to the symmetry and relationship of facial proportions , evaluates the appearance of the articular area for the presence of swelling or hyperemia, which may indicate the presence of edema and an acute inflammatory process. The specialist also examines the oral cavity and analyzes the degree of mouth opening , assesses the mobility of the lower jaw , determines the type of bite and looks at defects in the dentition (sometimes even poorly applied fillings or unsuccessful dentures can affect the condition of the TMJ, causing its overload).
This is followed by palpation and auscultation of the problem area. The doctor examines the condition of the masticatory muscles and tissues in the TMJ area, assesses pain , and looks at the position of the articular heads . Listening to the sounds accompanying the movement of the joint is also an important part of the diagnosis, since crepitus often accompanies TMJ pathologies. In some cases, impressions are taken to make diagnostic plaster models of the jaws, allowing the closure of the dentition and bite to be assessed, and occludograms are made (a relief impression of the occlusal contacts of the dentition on a wax plate).
The variety of clinical manifestations of pathologies of the temporomandibular joint in some cases requires special x-ray studies. To assess the condition of the joint, X-rays of the TMJ, CT, or MRI may be performed. These studies, together with the results of examination and analysis of models, make it possible to obtain detailed data on the degree of destructive changes and the nature of pathological processes in the joint.
Ankylosis of the TMJ: why does it occur and can it be treated conservatively?
Direct blows to the jaw, purulent-inflammatory diseases in the facial area, intrauterine development disorders, neonatal sepsis, and birth injuries can lead to the growth of connective tissue and fusion of the joint with the bone. This inevitably leads to the fact that the TMJ stops moving as it should, up to complete immobilization. As a result, the patient cannot eat normally, speak, breathe, or sleep. And when vomiting there is a danger of asphyxia. Therefore, ankylosis requires immediate treatment. In the initial stages, the disease is amenable to conservative therapy:
- the use of ultrasound;
- using a device that emits magnetic waves;
- carrying out electrophoresis;
- injection of hyaluronidase, which destroys connective tissue;
- intra-articular injections;
- forced jaw extension under anesthesia.
However, if we are talking about bone fusion, then no medications, devices or gymnastics will help. To ensure a normal life, a patient with ankylosis requires surgery. Typically this involves osteotomy and the use of implants. But the treatment does not end there. This is followed by a rehabilitation period, an orthodontic stage and, if necessary, mentoplasty.
Patients with ankylosis are complex and need professional help like no one else.
Treatment methods
Physiotherapy of TMJ
The method of treating arthrosis of the temporomandibular joint depends on the cause that caused the destruction of cartilage and bone deformation, as well as on the stage of the disease and the rate of progression of the process.
Typically used:
- drug treatment;
- physiotherapy;
- massage and exercise therapy;
- surgical intervention in severe advanced cases;
- folk remedies or homeopathy.
In all cases, it is necessary to follow a special diet to reduce the risk of inflammation, relieve stress on the digestive organs, strengthen the immune system and relieve the intestines. Postoperative diet 1a, 1b is used, then diet No. 15.
Conservative treatment
To relieve pain, non-steroidal anti-inflammatory drugs are used, for example, ketoprofen, ibuprofen, paracetamol.
Antibiotics are used to eliminate the infection. Antibacterial therapy helps to cope with pathogenic microorganisms if joint surgery is planned.
Immobilization of the jaw - creating conditions under which the muscles are least involved in work - the patient needs to be silent more, eat soft food that does not require chewing.
If necessary, bite correction methods are used - installation of braces or plates, selective grinding of teeth, replacement of dentures.
Chondroprotectors are additional concentrated nutrients that, at the initial stage, help grow new cartilage tissue in the joint if it is partially damaged. If the layer is completely destroyed, this cannot be done.
Traditional recipes for restoring cartilage tissue
It is recommended to consume birch ash internally to replenish the supply of microelements.
Birch ash is considered the most useful of all. It was used to treat many diseases in ancient times. Due to the rich composition of microelements and the properties of removing toxins from the body and cleansing the intestines, ash is recommended to be taken for arthritis and arthrosis to restore cartilage tissue.
To prepare the medicine, you need:
- Take 3 tablespoons of birch ash (the tree should not be older than 50 years).
- Pour half a liter of water into the powder and leave for 2 hours.
Take 4 tablespoons twice a day. The infusion also helps with atherosclerosis and coronary heart disease.
Traditional recipes can be used in addition to the main therapy and only at the initial stage.
TMJ replacement surgery
TMJ prosthesis
Depending on the severity of the patient’s condition, several types of surgical intervention are performed:
- introduction of hyaluronic acid into the joint cavity, which softens friction;
- removal of excess joint fluid;
- prosthetics using the body’s own tissues;
- endoprosthetics – removal of one’s own and implantation of an artificial prosthesis.
If the problem is the condition of the ligament, the surgeon shortens the ligament to stabilize the head in the fossa.
The danger of the disease is that it is asymptomatic for a long time, but when a pronounced clinical picture appears, it can be difficult to cope with arthrosis. If a person also has a metabolic disorder and the body does not absorb certain nutrients, the joint gradually degrades, despite taking expensive chondroprotectors and enzymatic drugs.
Diagnostic measures
Differential diagnosis with arthritis
The diagnosis can be made on the basis of X-ray examination, functional testing of the joint and clinical factors.
If arthrosis is suspected, consult the following doctors:
- orthopedic dentist or orthodontist;
- traumatologist, if the hospital does not have a highly specialized doctor;
- rheumatologist;
- endocrinologist or infectious disease specialist for consultation.
During the examination, the functionality of the joint, the degree of opening of the joint is assessed, and the activity of the masticatory and temporal muscles is checked using an electromyography device.
The most accurate in terms of visualization of hard and soft tissues are MRI and CT.
During diagnosis, a differential diagnosis is made with the following diseases:
- The contracture of the lower jaw is cicatricial. May restrict movement, but cartilage destruction is not observed.
- Benign tumors – osteoma, chondroma, osteochondroma, odontoma and others.
- BSD is a pain syndrome of dysfunction, which is characterized by joint pain and clicking, but the symptoms are temporary.
- Arthritis of the TMJ, which is characterized by sharp shooting pains, redness of the skin, and increased local temperature.
Arthritis is supported by the fact that the person previously suffered an infectious disease in nearby structures.
TMJ pathologies
The temporomandibular joint (articulatio temporomandibular) is a paired joint at the junction of the skull and lower jaw. The TMJ is formed by the articulation of the mandibular fossa of the temporal bone and the head of the mandible. This is the only movable element of the skull that performs a large number of complex functions . As mentioned above, the joint allows the lower jaw to move down and up, right and left, forward and backward, allows a person to close and open the mouth, and is responsible for speech formation, singing, chewing and swallowing.
Today, TMJ diseases occur in a fairly large number of patients. Since the jaw joint is a complex functional system, its pathology can be multidisciplinary in nature and in some cases requires the collaboration of specialists from different fields, from maxillofacial surgery to neurology.
Let's look at the main types of TMJ diseases
- Musculo-articular dysfunction of the TMJ . It is a disorder of the function of the masticatory muscles of the joint and a violation of the relative position of the elements of the TMJ.
- Arthrosis of the TMJ . A disease of a dystrophic nature, expressed in progressive degenerative changes in the joint, narrowing of the joint space and disruption of the activity of the masticatory muscles.
- Arthritis of the TMJ . An inflammatory disease of the temporomandibular joint that develops due to injuries, allergic reactions, and infections. The picture includes various destructive changes in the form of widening or narrowing of the joint space, osteoporosis.
- Dislocation and subluxation of the head of the joint . It is expressed in the exit of the articular head beyond the limits of the articular fossa of the temporal bone as a result of a violation of the relative position of the elements of the TMJ.
- Articular disc lesions . A common pathology of the TMJ, manifested in deviation of the position of the articular disc from the norm, its displacement.
- Ankylosis of the TMJ . Severe impairment of TMJ mobility, which can be either congenital or acquired. With ankylosis, fusion of the articular surfaces occurs, leading to a partial or even complete lack of mobility in the joint.
Among the causes of the listed pathologies, various factors can be indicated, including the effects of infections, autoimmune diseases and connective tissue diseases (in the case of arthritis). Endocrine disorders and injuries (arthrosis) can also affect the health of the TMJ. Acute and chronic diseases of the TMJ, purulent processes, osteomyelitis, rheumatoid disease and joint fractures can lead to ankylosis. Occlusal disorders, psycho-emotional factors, unsuccessful prosthetics and even unsuccessful eruption of wisdom teeth or other dentition pathologies can cause muscular-articular dysfunction. Bite pathologies, poor-quality prosthetics and mechanical injuries to the joint can also lead to displacement of the articular disc and dislocations.
Prevention of cartilage destruction
People who have a family history of joint disease should pay more attention to their own feelings. According to statistics, most cases of arthrosis occur in old age, but with poor heredity the disease may appear earlier.
To avoid the destruction of cartilage tissue, it is necessary to eat rationally, take complex vitamin supplements or natural calcium. In summer, exposure to the sun's rays is of great importance, because the synthesized vitamin D promotes the proper absorption of calcium and strengthens bone tissue.