Publication date: March 13, 2022.
Date the information on this page was updated: February 01, 2022.
TMJ dysfunction is a fairly common pathology these days, as it is largely caused by stress factors. Here it can be difficult to understand what is primary and what is secondary, because people with joint dysfunction usually come with bite pathology, pathology of the musculoskeletal system (curvature of the spine, neck). Therefore, joint treatment is a complex story. It happens that the primary pathology is a pathology of the joint, and sometimes it is the musculoskeletal system.
Comprehensive treatment of TMJ
When the doctor has determined the cause of the joint pathology, or causes, he determines the patient's readiness for a comprehensive treatment plan. In addition to the orthodontist, an osteopath or chiropractor may be involved, or even an orthopedist if more complex correction of the musculoskeletal system is required.
The patient should be aware that it is possible to straighten the jaw using a splint or splint, but this will not solve the problem of malocclusion. Orthodontic treatment will be required to correct the bite. If you have already had orthodontic treatment before, then it is more difficult to decide on repeated treatment.
Therefore, first the problem with the joint is solved using a splint or joint splint, then bite correction is carried out, and, if necessary, prosthetics. In parallel, work is underway with an osteopath to restore the muscular corset of the back and neck.
It happens that a patient refuses treatment with braces after the problem with the joint has been resolved. In this case, we warn him about the need to wear a joint splint constantly in order to avoid the recurrence of old problems with the TMJ. After all, a relapse can happen quite quickly due to stress.
How dangerous is the disease?
Often, arthrosis of the jaw in the first stages is asymptomatic, which leads to prolonged inactivity in the treatment of the pathology. However, ignoring the disease is dangerous. If you notice at least one of the symptoms, you should visit a doctor. In advanced forms of pathology, medications, orthopedics and even surgery are used.
The risk group includes persons:
- over 50 years old;
- females who have reached menopause;
- those who have had injuries and surgeries of the jaw;
- with malocclusion, diseases in the jaw area;
- with damaged or missing teeth;
- with chronic inflammatory diseases;
- with arthrosis of other joints;
- whose family members suffer from jaw joint dysfunction.
What may be the symptoms of TMJ dysfunction?
- Tenderness or pain in the area of one or both TMJs at rest or when opening the mouth.
- Crunching, clicking, crepitation and other noises in the area of one or both TMJs when opening the mouth.
- History of TMJ injuries (previous), incl. dislocation, subluxation, chronic subluxation.
- Restrictions in the mobility of the TMJ, restrictions in opening the mouth.
- Excessive tone of the masticatory muscles, bruxism (“grinding” of teeth in sleep, at rest).
- Asymmetry of the chin, lips, lip frenulum, asymmetry of mouth opening, S-shaped opening.
- Suspicion of a forced position of the lower jaw.
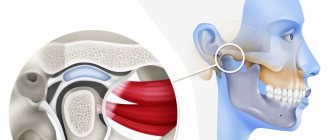
Structure of the TMJ
The presence of one or more of the above symptoms may indicate TMJ dysfunction.
Traditional orthodontic treatment does not address TMJ dysfunction. During orthodontic treatment, the severity of dysfunction may not change, decrease or increase. At the moment, in the world scientific orthodontic literature there is no convincing data on the connection between orthodontic treatment and the condition of TMJ. Deterioration of the joint after treatment may have nothing to do with this treatment.
Note! Even in the absence of visible clinical manifestations of joint dysfunction, hidden disorders may occur that require special diagnostics to identify them.
If there is a forced incorrect position of the lower jaw, its position may change during the treatment process with changes and complication of the treatment plan (the need to remove individual teeth, increasing the duration of treatment). A reliably forced position cannot be diagnosed by traditional orthodontic methods; to verify its presence, as a rule, a special analysis is required (manual functional analysis, determination of the central relationship of the jaws), the use of a special articular splint for a period of several months, which, however, does not give 100 % guarantees.
To conduct a detailed articular diagnosis, explain the specifics of your case, and further manufacture an articular splint, you can make an appointment with an orthodontist who deals with the issue of TMJ dysfunction.
TMJ dysfunction is a chronic condition that can be compensated, but not cured (i.e., it is possible to eliminate symptoms, however, pathological changes in the joints, if they have already occurred, will most likely persist).
Accurate diagnosis
Since the jaw joint has a complex structure, there are many possible causes for the development of arthrosis. This significantly complicates the process of diagnosing and identifying the problem causing it. The dentist questions and examines the patient for facial asymmetry, sunken lips, cracks in their corners, palpates the muscles, determining the stiffness of movements. The doctor will determine arthrosis of the jaw joint immediately after these actions.
To determine the stage of development of the disease and its localization, radiography is most often used. An x-ray allows you to see the resulting deformations, bone growths, and changes in their shape. Less commonly used are CT scans, electromyography, contrast radiography, or braces (orthodontic brackets).
What happens if TMJ dysfunction is not treated?
If the dysfunction is not treated, the compensatory capabilities of the body may sooner or later be exhausted, the symptoms will worsen, the pathology will begin to progress, causing greater discomfort (sometimes for several years), thereby affecting the deterioration of the function of the dental system.
In order to try to prevent this and carry out treatment taking into account the individual characteristics of the structure and functioning of the temporomandibular joints, patients are usually offered the following approach.
Treatment method for TMJ dysfunction
1. Diagnosis of TMJ dysfunction.
- When diagnosing a joint in the clinic, a series of measurements and tests are carried out, all sensations in the joint area are recorded (discomfort, clicks, pain, deviation of the jaw when opening and closing), the difference in sensations in the right and left joint.
- The orthodontist also takes impressions of the jaws and takes photographs of the face and intraoral photographs, and also performs three-dimensional computed tomography of the face (3D CT); if necessary, the doctor can give a referral for an additional study - magnetic resonance imaging of the TMJ (MRI).
- Often, the orthodontist, in addition to manual functional analysis, conducts a visual assessment of: posture, symmetry of the shoulder girdle, shoulder blades, hip bone structures, etc., performs the necessary tests and photographs. Based on the results, it is possible to schedule a consultation with an osteopath or chiropractor to jointly manage the patient. Related specialists (orthopedist, surgeon, periodontist) can also be involved in drawing up a treatment plan.
What exercises are prescribed to patients to normalize the work and relax the masticatory muscles?
Exercise No. 1
Draw a vertical line on the mirror with a marker, stand opposite so that the line divides your face into the right and left halves, place your fingers on the area of the articular heads, lift your tongue up and back, open and close your mouth along the line (it may not work right away), 2-3 times /day 30 repetitions. There is no need to open your mouth wide (a comfortable width), the main thing is symmetrically (so that the jaw does not “move” in any direction). If there is a click, open until it clicks.
Exercise No. 2 (cycle)
Do it whenever possible, for example, in front of the TV, at the computer, or in a traffic jam while driving. Open and close your mouth without closing your teeth for 30 seconds, then alternately reach your right and left cheeks with your tongue for 30 seconds. Open - close your mouth again, then for 30 seconds move your tongue in a circle inside the vestibule (behind the lips), first in one direction, then in the other direction (clockwise - counterclockwise), open again - close your mouth, etc.. For this a half-hour cycle, the teeth should not touch, the lips should be closed. If you want to close your mouth or swallow, place your tongue between your teeth. Repeat the cycle for 20-30 minutes 2-3 times/day
Folk remedies
With the permission of a doctor, non-traditional methods of treating arthrosis of the jaw joint can be used. There are both simple and complex traditional medicines to prepare. For example, warming with salt or sand is a great way to cope with pain. They need to be warmed up, poured into a textile bag and applied to the affected jaw for 1.5-2 hours until completely cooled. Another simple recipe is to use raw egg whites. At night, apply it to the entire jaw and the area behind the ears.
Among the more labor-intensive, but also more effective folk remedies, the following can be distinguished:
Drops based on celandine
- Mix crushed and squeezed celandine through cheesecloth with honey in a 1:1 ratio.
- When the honey is completely dissolved, the medicine is ready.
- Place 1 drop in each nostril before bedtime. In the first few days, this treatment may cause discomfort, but over time the effect will be noticeable.
Solution for compresses
- Mix 5 g of the following components: rhizomes of elecampane, burdock and horseradish, leaves and flowers of mint, St. John's wort, lemon balm, celandine, calendula, eucalyptus, plantain, juniper fruits.
- Grind the raw materials and pour in hot corn oil.
- After cooling, the solution is freed from all solid ingredients.
- Add 5 g of bee bread and propolis to the resulting liquid.
- Infuse the medicine in a warm place for about 20 minutes.
- At this time, mix 100 g of gum turpentine with 15-20 g of gum rosin.
- After 20 minutes, mix both solutions.
- Use the resulting mixture as compresses at night.
Occlusive therapy for TMJ dysfunction
After diagnosis, the patient is scheduled for an appointment with the orthodontist to determine the central relationship of the jaws (“true” position of the lower jaw, the position in which your joint and chewing muscles will be most comfortable).
In order to more accurately establish and fix this position, an occlusal splint (splint) will be individually made for the patient from a special plastic, which is erased as it is worn. The splint must be worn constantly (sleeping, talking, eating in it if possible) - this is the meaning of occlusion therapy, which will help the joint and masticatory muscles rebuild into the most comfortable functional state.
Cleaning and caring for the splint is very simple - after eating (as well as while brushing your teeth), brush with a soft brush with toothpaste or soap.
Installation of a brace system for a patient with TMJ dysfunction
Installation of a brace system on the upper jaw is carried out on average after 3 months of occlusion therapy. The splint is adjusted once every 1-2 weeks, or at the discretion of the doctor, until the main complaints from the TMJ are eliminated (in parallel with the alignment of the teeth in the upper jaw), then a brace system is installed on the lower jaw with partial reduction (grinding) of the interfering parts of the occlusal tires, or complete removal. Here the patient needs to be patient - the process may take several months.
At the same time, the new position of the lower jaw is monitored: repeated manual functional analysis, photometry, bite registration is possible, computed tomography of the face during treatment, continuation of orthodontic treatment with a brace system.
Upon completion of orthodontic treatment, final monitoring of the position of the lower jaw follows (manual functional analysis, photometry, bite registration, 3D CT scan of the face upon completion (after) treatment).
Joint splint
Joint splint with braces