Have questions?
Viral stomatitis is an inflammation of the soft tissues of the oral cavity caused by a virus.
The disease itself is a reaction of the human body to certain factors. So, most often the cause of the disease is infection with chickenpox, herpes, measles, and influenza.
Typically, infectious stomatitis is manifested by damage to the corners of the lips and mucous membrane of the mouth. Such symptoms are characteristic of the herpes virus and are most often found in children under three years of age. If a person’s immunity is strong and can resist the virus, the disease passes without a trace. In weakened patients, the disease can develop into a chronic form.
Causes of viral stomatitis
The occurrence of the disease is caused by a complication of the primary disease (chickenpox, herpes, etc.). The following may cause signs of the disease:
- poor oral hygiene;
- untreated caries;
- gingivitis, periodontal disease;
- unbalanced diet;
- avitaminosis;
- general weakening of the body;
- long-term antibiotic therapy.
Inflammation in other organs and systems of the body also causes viral stomatitis in children and adults.
Is aphthous stomatitis contagious?
Canker sores can be contracted if the condition is caused by a virus, fungus, or infection. The pathogen is easily transmitted through shared objects and airborne droplets.
Children are especially susceptible to infectious stomatitis - due to their age, the mucous membranes of the oral cavity have not yet formed the required level of protection. Aphthous stomatitis is especially severe in infants, including those with damage to internal organs. Adults have a chance of getting sick only when they have microcracks or abrasions in the mouth.
Fungal stomatitis is transmitted through water, dishes, and food.
Stomatitis that develops as a result of vitamin deficiency, stress or mechanical trauma is not contagious.
Features of the clinical picture
The symptoms of viral stomatitis at the initial stage of its development are easily confused with the symptoms of a common cold. The patient's body temperature rises and a headache appears. Gradually, the oral mucosa becomes very swollen and red, making it difficult for the patient to chew and swallow.
A few days after the onset of the inflammatory process, rashes characteristic of the disease appear:
- ulcers on the inside of the cheeks, palate, gums and tongue;
- groups of bubbles with clear liquid inside;
- “cold” on the lips, on the mucous membranes of the cheeks and in the nose;
- erosions that itch and hurt.
A whitish coating appears in the mouth of a sick person. The patient is concerned about general malaise, lack of appetite, bad breath and swollen lymph nodes.
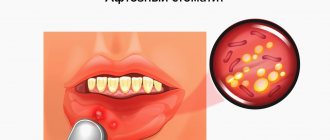
What is aphthous stomatitis
The exact mechanisms of development of aphthous stomatitis are still unknown.
It is generally accepted that with aphthous stomatitis, the infection enters the oral cavity, but does not cause a protective reaction in the body's immune cells. They simply do not recognize the pathogen. The infection changes the composition of saliva, this causes the activity of lymphocytes and the immune system attacks areas of the oral mucosa as a foreign chemical agent.
As a result of this confrontation, erosions form on the mucous membrane.
Aphthae have a round or oblong shape with a diameter of up to 5 mm. Outwardly, they resemble ulcers, covered with a white or gray coating and outlined with a red rim. On the mucous membrane, aphthae are located in groups or separately.
If more than three canker sores have formed in the mouth, this is a severe form of stomatitis. Despite their small size, the ulcers are painful and interfere with eating and talking. With stomatitis, the temperature may rise and weakness may appear.
If a person's immune system is weak, it will continue to interpret the presence of foreign chemicals in the mouth as a danger and canker sores will become chronic. Therefore, it is important to start treatment of aphthous stomatitis on time and carry it out under the supervision of a doctor.
How is viral stomatitis treated?
Often, treatment of viral stomatitis is based on local exposure to damaged areas of the mucous membrane and skin. Ulcers and erosions are treated with an antiseptic and painkillers, the dentist prescribes applications (application of the drug) with anti-inflammatory and wound-healing compounds. To strengthen the immune system, the patient is prescribed medications based on echinacea and vitamins.
It is also important to follow a diet during therapy. All products consumed must be neutral in taste, pureed, and not hot.
You cannot self-medicate: without the help of a doctor, the disease can develop into a chronic form.
It is advisable to reduce home treatment of viral stomatitis in adults and children only to procedures that will speed up the healing process of lesions. The doctor will recommend rinsing with decoctions of herbs and oak bark.
Ways of transmission of stomatitis
Let's summarize. Viral, bacterial and herpetic forms of stomatitis are contagious. Knowing how the disease is transmitted, you can protect yourself and your loved ones. Ways of transmission of infection:
- airborne - sneezing, coughing;
- household items - common dishes, linen, personal items;
- toys, raw pacifiers, rattles;
- dirty hands;
- unwashed food;
- biological fluids - through saliva, blood, breast milk;
- Pets can carry the virus.
It is possible to catch the infection anywhere – from the street to your own home. You can get infected from both a child and an adult.
Incubation period
When any virus enters the human body, there is an incubation period during which symptoms do not appear or do not indicate a specific type of virus. It is impossible to predict the incubation period of the virus before the onset of stomatitis, because:
- The type of virus itself is not known.
- It is not known whether stomatitis will occur at all or whether it can be avoided.
However, in cases of stomatitis, it is noticed that the virus is activated within a period of several days (herpes, measles, adenoviruses) to two weeks (chickenpox). And with proper treatment it goes away in about a week or two.
In cases of herpes, the virus most often remains dormant in the host’s body after treatment. At the same time, others can become infected, and the person himself, until the level of immunity sharply decreases against the background of other diseases, will feel completely healthy.
How the disease is transmitted
Any virus can be picked up in three possible ways: airborne, contact and directly through the blood. Thus, you can become infected anywhere - at work, in a cafe through poorly washed dishes, in children's groups (kindergartens, clubs and schools through toys and common objects), in entertainment centers (slot machines), in large supermarkets (pen carts and baskets), in public transport (handrails), in clinics and hospitals.
It is impossible to avoid transmission of the virus, but you can prevent it from getting inside by observing basic hygiene rules: wash your hands after going outside and before eating, before leaving home during epidemics, and also in the autumn-winter period use special antiviral ointments (oxolinic, viferon and etc.), always have sanitary napkins or hand sanitizer gel with you.
Clinic, diagnosis and treatment of acute herpetic stomatitis in children
- What is the clinical picture of acute herpetic stomatitis?
- What are the new treatment regimens?
The problem of diseases of the oral mucosa is one of the most important in dentistry.
Acute herpetic stomatitis occupies a special place here, primarily because it accounts for more than 80% of all diseases of the oral mucosa in children. The combined use of virological, serological and immunofluorescence research methods confirms that acute herpetic stomatitis is one of the clinical forms of primary herpetic infection.
The spread of the disease in 71% of cases among children aged 1 to 3 years is explained by the fact that at this age, antibodies received from the mother interplacentally disappear in children, as well as the lack of mature specific immune systems. Among older children, the incidence is significantly lower due to acquired immunity after a herpes infection in its various clinical manifestations.
Great importance in the pathogenesis of the disease is attached to the lymph nodes and elements of the reticuloendothelial system, which is quite consistent with the pathogenesis of the sequential development of clinical signs of stomatitis. The appearance of lesions on the oral mucosa is preceded by lymphadenitis of varying severity. Most often they are observed in severe and moderate stomatitis. As a rule, lymphadenitis is bilateral, submandibular. However, with moderate and severe forms of the disease, simultaneous involvement of the cervical lymph nodes in the process is also possible. Lymphadenitis accompanies the entire period of the disease and persists for 7-10 days after complete epithelization of the elements.
The body's resistance to the disease is determined by its immunological defense. Both specific and nonspecific immune factors play a role in immunological reactivity. Violation of nonspecific immunological reactivity determines the severity of the disease and the periods of its development. Moderate and severe forms of stomatitis led to a sharp suppression of natural immunity, which was restored 7-14 days after the child’s clinical recovery.
The severity of acute herpetic stomatitis is assessed by the severity and nature of toxicosis and damage to the oral mucosa. The development of the disease goes through five periods: incubation, prodromal, period of disease development, extinction and clinical recovery.
| Elements of herpetic stomatitis |
The mild form of acute herpetic stomatitis is characterized by an external absence of symptoms of intoxication; the prodromal period is clinically absent.
The disease begins suddenly with an increase in temperature to 37-37.5°C. The general condition of the child is quite satisfactory. In the oral cavity there are signs of hyperemia and slight swelling, mainly in the area of the gingival margin (catarrhal gingivitis). In most cases, against the background of increased hyperemia, single or grouped lesions appear in the oral cavity, the number of which usually does not exceed six. The rashes are one-time only. The duration of the disease development is 1-2 days.
The period of extinction of the disease is longer. Within 1-2 days, the elements acquire a marble-like color, their edges and center are blurred. They are already less painful. After epithelialization of the elements, the phenomena of catarrhal gingivitis persist for 2-3 days, especially in the area of the anterior teeth of the upper and lower jaw.
In children suffering from this form of the disease, as a rule, there are no changes in the blood, sometimes only towards the end of the disease a slight lymphocytosis appears (in children 1-3 years old, the number of lymphocytes is normally up to 50%). Herpetic complement-fixing antibodies are not often detected during convalescence. In this form, the protective mechanisms of saliva are well expressed: pH 7.4±0.04, which corresponds to the optimal state. At the height of the disease, the antiviral factor interferon appears in saliva from 8 to 12 units/ml. The decrease in lysozyme in saliva is not pronounced.
The moderate form of acute herpetic stomatitis is characterized by fairly clearly defined symptoms of toxicosis and damage to the oral mucosa during all periods of the disease. Already in the prodromal period, the child’s well-being worsens, weakness, loss of appetite appear, the child is capricious, there may be catarrhal tonsillitis or symptoms of an acute respiratory disease. The submandibular lymph nodes enlarge and become painful. The temperature rises to 37-37.5°C.
As the disease progresses (catarrhal phase), the temperature reaches 38-39°C, headache, nausea, and pale skin appear. At the peak of the rise in temperature, increased hyperemia and severe swelling of the mucous membrane, elements of the lesion appear both in the oral cavity and on the skin of the face in the perioral area. In the oral cavity there are usually from 10 to 20-25 lesions. During this period, salivation increases, saliva becomes viscous and viscous. Severe gingivitis and bleeding gums are noted.
Rashes often recur, as a result of which, when examining the oral cavity, one can see elements of the lesion that are at different stages of clinical and cytological development. After the first eruption of lesions, body temperature usually drops to 37-37.5°C. However, subsequent rashes are usually accompanied by a rise in temperature to the previous levels. The child does not eat, sleeps poorly, and symptoms of secondary toxicosis increase.
An ESR of up to 20 mm/hour is observed in the blood, often leukopenia, sometimes slight leukocytosis. Band and monocytes within the higher limits of normal, lymphocytosis and plasmacytosis. An increase in the titer of herpetic complement-fixing antibodies is detected more often than after suffering a mild form of stomatitis.
The duration of the period of extinction of the disease depends on the resistance of the child’s body, the presence of carious and damaged teeth in the oral cavity, and irrational therapy. The latter factors contribute to the fusion of lesion elements, their subsequent ulceration, and the appearance of ulcerative gingivitis. Epithelization of the lesion elements takes up to 4-5 days. Gingivitis, severe bleeding and lymphadenitis last the longest.
With a moderate course of the disease, the pH of saliva becomes more acidic, reaching 6.96 ± 0.07 during rashes. The amount of interferon is less than in children with a mild course of the disease, but does not exceed 8 units/ml and is not detected in everyone. The content of lysozyme in saliva decreases more than in mild forms of stomatitis. The temperature of the unchanged oral mucosa is in accordance with the child’s body temperature, while the temperature of the affected elements in the degeneration stage is 1.0-1.2°C lower than the temperature of the unchanged mucosa. With the beginning of regeneration and during the period of epithelization, the temperature of the affected elements rises to 1.80 and remains at a higher level until complete epithelization of the affected mucosa.
The severe form of acute herpetic stomatitis is much less common than the moderate and mild form.
During the prodromal period, all the signs of an incipient acute infectious disease occur: apathy, adynamia, headache, musculocutaneous hyperesthesia and arthralgia, etc. Symptoms of damage to the cardiovascular system are often observed: bradycardia and tachycardia, muffled heart sounds, arterial hypotension. Some children experience nosebleeds, nausea, vomiting, and pronounced lymphadenitis of not only the submandibular, but also the cervical lymph nodes.
During the development of the disease, the temperature rises to 39-40°C. The child has a mournful expression on his lips and painfully sunken eyes. There may be a mild runny nose, coughing, and the conjunctivae of the eyes are somewhat swollen and hyperemic. Lips are dry, bright, parched. In the oral cavity, the mucous membrane is swollen, clearly hyperemic, with pronounced gingivitis.
After 1-2 days, lesions up to 20-25 begin to appear in the oral cavity. Often, rashes in the form of typical herpetic blisters form on the skin of the perioral area, the skin of the eyelids and conjunctiva of the eyes, the lobes of the ears, on the fingers, like a panaritium. Rashes in the oral cavity recur, and therefore at the height of the disease in a seriously ill child there are about 100 of them. The elements merge, forming extensive areas of mucosal necrosis. Not only the lips, cheeks, tongue, soft and hard palate are affected, but also the gingival margin. Catarrhal gingivitis turns into ulcerative-necrotic. A sharp putrid odor from the mouth, profuse salivation mixed with blood. Inflammation in the mucous membranes of the nose, respiratory tract, and eyes worsens. Streaks of blood are also found in secretions from the nose and larynx, and sometimes nosebleeds are observed. In this condition, children need active treatment from a pediatrician and dentist, and therefore it is advisable to hospitalize the child in a boxed ward of a children's or infectious diseases hospital.
In the blood of children with severe stomatitis, leukopenia, a band shift to the left, eosinophilia, single plasma cells, and young forms of neutrophils are detected. In the latter, toxic granularity is very rarely observed. Herpetic complement-fixing antibodies are, as a rule, always detected during the period of convalescence.
Saliva has an acidic environment (pH 6.55±0.2), which can then be replaced by more pronounced alkalinity (8.1-8.4). Interferon is usually absent, the content of lysozyme is sharply reduced.
The diagnosis of acute herpetic stomatitis is made based on the clinical picture of the disease. The use of virological and serological diagnostic methods, especially in practical healthcare, is difficult. This is primarily due to the difficulty of conducting special research methods. In addition, with these methods, results can be obtained at best towards the end of the disease or some time after recovery. Such a retrospective diagnosis cannot satisfy the clinician.
It should be emphasized that in recent years the immunofluorescence method has been increasingly used. The high percentage of coincidences (79.0±0.6%) of the diagnosis of acute herpetic stomatitis, according to immunofluorescence data, with the results of virological and serological studies make this method the leading one in diagnosing the disease.
The doctor’s tactics when treating patients with acute herpetic stomatitis should be determined by the severity of the disease and the period of its development.
Due to the peculiarities of the course of acute herpetic stomatitis, rational nutrition and proper organization of feeding the patient occupy an important place in the complex of therapeutic measures. Food must be complete, that is, contain all the necessary nutrients, as well as vitamins. Therefore, it is necessary to include fresh vegetables, fruits, berries, and juices in your diet. Before feeding, the oral mucosa should be anesthetized with a 2-5% solution of anesthetic emulsion.
The child is fed predominantly liquid or semi-liquid food that does not irritate the inflamed mucous membrane. It is necessary to give the child enough fluids. This is especially important during intoxication. During meals, natural gastric juice or its substitutes should be given, since when there is pain in the mouth, the enzymatic activity of the stomach glands reflexively decreases.
Local therapy for acute herpetic stomatitis has the following objectives:
- relieve or reduce painful symptoms in the oral cavity;
- prevent repeated eruptions of lesions (reinfection) and promote their epithelization.
From the first days of the disease, given its etiology, in local treatment, serious attention should be paid to antiviral therapy. For this purpose, it is recommended to use 0.25% oxolinic, 0.5% tebrofen ointments, Zovirax, solutions of interferon and neoferon.
It is recommended to use the listed medications repeatedly (3-4 times a day) not only when visiting a dentist, but also at home. It should be borne in mind that antiviral agents must be applied to both the affected areas of the mucosa and areas that do not contain elements of the lesion, since they have more of a preventive effect than a therapeutic one.
During the period of extinction of the disease, antiviral drugs can be discontinued.
Particular importance should be attached to keratoplasty agents at this time. These are primarily oil solutions A and B, sea buckthorn oil, caratoline, rosehip oil, ointments with methyluracil, and an oxygen cocktail.
A study of the state of local immunity in children with acute herpetic stomatitis revealed that it correlates with the nature of the pathological process, therefore we consider it pathogenetically justified to include measures aimed at their elimination in a comprehensive treatment regimen.
At the Department of Pediatric Therapeutic Dentistry of the Moscow State Medical University, the drug imudon from Solvay pharma was prescribed to 80 children aged 2 to 4.5 years in the complex treatment of acute herpetic stomatitis. 40 children were diagnosed with mild, 38 children with moderate and 2 with severe forms of stomatitis.
Imudon is a mixture of lysates: 0.050 g (dry product) Lactobassillus acidophilus, fermentatum, helveticus, lactis Streptococcus pyogenes (2 var.), faecalis, faecium, sanguinis Staphilococcus aureus Klebsiella pneumoniae, Corynebacterium pseudodiphteriticum, Fusiformis fusiformis, Candida albicans.
Preservative: Sodium mercurothiolate: 0.0125 mg.
Excipients: lactose, mannitol, saccharin, sodium bicarbonate, anhydrous citric acid, precirol fine, magnesium stearate, polyvinylpyrrolidone.
pharmachologic effect
Imudon is intended for local specific immunotherapy of diseases of the oral cavity and pharynx. The effect of the drug on the immune system is expressed in an increase in the phagocytic activity of macrophages, an increase in the content of lysozyme in saliva, as well as an increase in the number of immunocompetent cells and the content of local antibodies (class A immunoglobulins). Thus, imudon has a therapeutic specific antimicrobial and anti-inflammatory effect, and also, by increasing the immune local protective barrier, ensures the prevention of relapses.
The first group consisted of children treated with 0.5% tebrofen ointment, the second group included children treated with interferon solution. In the third group, on the day of treatment, in addition to 0.5% tebrofen, imudon was prescribed, and in the fourth group, imudon + interferon. Children took Imudon tablets 5-6 times a day, no earlier than 30-40 minutes after treating the oral cavity with antiviral ointment, and dissolved it in the oral cavity.
Criteria for clinical and laboratory assessment of the therapeutic effectiveness of the drug imudon:
- The therapeutic effect is the average recovery time.
- Analgesic effect.
- General and local reactions to the drug.
- Influence on the state of local immunity.
Recovery was considered to be the epithelization of the lesion elements without a complete cure of the child from acute herpetic stomatitis, the duration of which is determined not only by the end of the epithelization of the lesion elements, but also by the duration of gingivitis and lymphadenitis, as well as deviations in the general well-being of the child.
As can be seen from table. 1, timely correction of local immunity increases the effectiveness of ongoing treatment measures and allows for faster recovery of children with AHS.
The effectiveness of the drug was manifested in groups 3 and 4 on the second day in case of contacting a doctor on the first day of the disease: erosions did not develop into aphthae, and the surrounding mucous membrane was not infiltrated.
Table data 1 indicate the advantage of complex therapy for OGS over generally accepted methods of treatment, its high efficiency, confirmed by a reliable reduction in the time of epithelization of elements and recovery of children.
The more effectively the drug stops the disease, the faster it normalizes the pathological infectious process, the more actively the factors of local immunological defense are restored. (Table 2).
We have given a high assessment of the effectiveness of the new regimen of complex therapy for AHS using stimulating immunotherapy, in particular imudon; It was concluded that there is a fundamental need for an integrated approach to the treatment of acute herpetic stomatitis with the mandatory inclusion of imudon, both a stimulating and a replacement agent for the correction of local immunity.
Thus, the high effectiveness of imudon in the treatment of AHS due to the immune correction of saliva has been established. Imudon has a therapeutic, anti-inflammatory effect, reduces the time for epithelization of lesions. There were no complications or side effects when using the drug imudon. Children used the drug with pleasure, as it has a pleasant, minty taste that does not irritate the mucous membrane. Apparently due to the mint aroma there is a weak analgesic effect.
All this allows us to recommend imudon in the complex therapy of acute herpetic stomatitis in children.
In conclusion, it should be noted that acute herpetic stomatitis, occurring in any form, is an acute infectious disease and requires in all cases the attention of a pediatrician and dentist in order to provide comprehensive treatment, eliminate contact of a sick child with healthy children, and take measures to prevent this diseases in children's groups.
How to avoid getting stomatitis again
To avoid getting stomatitis again, you need to follow 3 rules:
- Maintain hygiene.
- Treat teeth, check and change orthopedic structures in a timely manner.
- Monitor your general health.
The first rule for preventing recurrent stomatitis is hygiene. It is best to have your teeth professionally cleaned by a dental hygienist after the symptoms of the disease have disappeared. A specialist will use ultrasonic equipment to remove tartar and old plaque and advise on further dental care tactics in each specific case. The professional cleaning procedure should be carried out 2 times a year to remove accumulated dirt that regular cleaning cannot remove. This is especially true for patients with braces or dentures - the presence of foreign structures in the mouth requires regular professional cleaning.
It is necessary to treat teeth so that there are no putrefactive processes in the mouth, and there are as few pathogenic bacteria in the microflora as possible. And if the cause of stomatitis or contributing factors were disturbances in the functioning of the body, then you need to closely monitor your health and maintain your immunity.
Preventive measures
A very important part of prevention is timely treatment of dental and ENT diseases.
Stomatitis can occur in anyone, regardless of age and lifestyle, but compliance with the following preventive measures can reduce this risk:
- Maintaining oral hygiene and timely treatment of dental diseases.
- Providing a balanced diet to supply the body with the necessary amount of vitamins and nutrients.
- Taking vitamin complexes in spring and autumn.
- Timely treatment of diseases of the ENT organs and digestive system.
- Rejection of bad habits.
Treatment
In addition to the day after the discovery of symptoms, the parents went to the doctor, important factors for drawing up the correct therapy are the age and immunity of the child. In general terms, the course of treatment will be as follows.
- Rinse.
The dentist prescribes anti-inflammatory drugs that are used to treat the mucous membrane daily. For children, you can also prepare decoctions of calendula or chamomile.
- Use of medications.
After rinsing, the sores are usually treated with ointments or oils, as well as antiviral ones. To do this, you can use and constantly change cotton swabs.
- Antipyretic and painkillers.
If there is an elevated temperature and severe pain, the doctor may prescribe appropriate medications.
If all recommendations are followed and depending on the severity of the disease, therapy can last up to several weeks. Parents need to remember that self-treatment can only worsen the situation. The doctor will not only prescribe an effective treatment, but most importantly, correctly determine the type of disease.
Diagnostics
If there is a suspicion of damage to the mucous membrane in the mouth, only a doctor, pediatrician or pediatric dentist should make a diagnosis and examine a child. It is important to identify the cause of the disease in order to prescribe effective treatment. Identifying the cause of the disease does not present any difficulties. This pathology is detected during examination due to the characteristic clinical picture, the presence of rashes, and signs of inflammation in the mouth. In addition to an examination to clarify the nature of the disease, the doctor prescribes a general blood and urine test. In severe cases, tissues of the affected mucous membrane are examined to identify the type of pathogen. For this purpose, washouts and scrapings from erosions and ulcers are taken.
The following methods are used to identify the type of virus:
- immunofluorescence method;
- PCR;
- RSK;
- ELISA.
In order to prescribe effective therapy, especially in severe cases, identification of the type of pathogen is required.
Prevention measures
To reduce the likelihood of developing stomatitis in a child, specialists at a family dentistry clinic in Moscow recommend:
- regularly wash and treat toys, bottles and other items that the baby uses;
- strengthen immunity;
- maintain a balanced diet that contains vitamins and minerals;
- treat diseases of the gastrointestinal tract, as well as colds and flus in a timely manner;
- Visit your dentist regularly for preventive examinations.
Such simple tips will help you avoid more serious consequences of the disease or even minimize its occurrence.