We often hear from parents that it is not necessary to treat baby teeth. After all, they will fall out by themselves. But this popular belief is wrong. Baby teeth, of course, will fall out in due time, but their diseases can bring a lot of suffering to children, as well as damage the health of future permanent teeth - even to the point of malocclusion. Let's figure out whether baby teeth need to be treated, in what cases and how to do it.
Treat or remove baby teeth
Before talking about how baby teeth are treated, it is necessary to note their features that distinguish them from permanent teeth. First of all, baby teeth have thinner enamel, making them very vulnerable to tooth decay and other damage. In addition, contrary to popular belief, baby teeth also have roots, although they are smaller and thinner than the roots of permanent teeth.
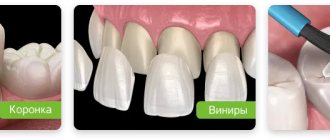
In this regard, the question arises: are milk teeth treated in children, or can they be removed if problems arise - after all, after some time, permanent teeth will appear in their place. It is important to understand here that most often a very short period of time passes between the spontaneous loss of a baby tooth and the appearance of a permanent one. In fact, the baby tooth falls out at the moment when the permanent tooth is ready to develop. But if a baby tooth is removed before its due date, an empty socket will appear on the child’s jaw, which may remain without a tooth for many weeks and even months. In this situation, neighboring teeth will begin to shift towards the socket, which will increase the gaps between them and create obstacles for the growth of a permanent tooth. It may begin to hurt, it will grow crooked, the formation of the bite will not occur correctly - and the child, in order to avoid serious problems and return a beautiful smile, will have to endure many dental procedures and even, probably, wear braces. Therefore, modern dentists are trying their best to preserve baby teeth until they naturally fall out - using different methods, including installing crowns.
In addition, when thinking about why we should treat baby teeth, we should not forget about the main function of teeth - chewing. If we simply remove a child’s diseased baby teeth, what will he chew on? In this case, the child will have to get a prosthesis, since it may take a long time for permanent teeth to emerge in place of the removed milk teeth.
Why is it important to preserve your child's primary teeth?
You need to fight decisively for every baby tooth, because it depends on:
- chewing function: nutrition directly affects the development of the body, the child should eat with pleasure and without any discomfort;
- speech formation: correct articulation depends on the teeth, therefore, they are necessary for the child to speak clearly and understandably;
- development of the dental system: premature loss of baby teeth leads to serious displacement of neighboring teeth, which causes the loss of space for a permanent tooth and changes the bite;
- psychological status: a child settling into society is vulnerable, anything can shake his self-esteem, and he needs a wide, white-toothed smile more than ever.
Is it necessary to treat caries of baby teeth?
Due to their thin enamel, baby teeth are very susceptible to tooth decay. At the earliest stage, caries does not even require drilling and filling - you can get by with polishing the tooth and applying a special mineralizing paste. But if the moment is missed and a hole has formed, then the treatment will be more serious. But in any case, parents who doubt whether it is worth treating caries of baby teeth should remember that on delicate baby teeth with thin enamel, caries develops much more rapidly than in adults. Therefore, severe toothache can suddenly overtake a child in the most inopportune situation - at the grandmother’s dacha, on a trip abroad. You will have to urgently look for a suitable clinic, possibly spend a lot of money and risk the child’s health, because if the tooth is removed poorly, parts of the roots may remain in the socket, which will interfere with the eruption of the permanent tooth.
Caries of baby teeth in children is also treated because it can become a source of infection, lead to periodontitis, and damage nearby permanent teeth. As in adults, caries in children must be treated promptly and as early as possible in order to preserve the tooth and not damage the normal development of the child’s jaw and bite.
Prevention is better than cure
As with adults, it is easier to keep children's teeth healthy than to get fillings. This task falls on the parents.
First of all, you need to brush your teeth from the moment they erupt. For babies there are soft silicone brushes that are used without paste. For children over 2 years old - children's brushes and toothpastes. There are also electric sonic brushes that introduce an element of game into the routine process: in a special application, daily “points” are given, a “reward” is given for good brushing of teeth for 30 days in a row and taken to the next level. You just need to choose a brush that is suitable for the child’s age - so that the bristles are not too hard.
Also, do not forget about scheduled appointments. If at the first appointments with the doctor the child’s teeth are not treated, but only examined, he will remember that there is nothing wrong with visiting the dentist. If you need treatment, it will be easier to go to a doctor you know.
Is there any other way to prevent the development of caries? There are several preventive procedures - remineralization, fluoridation of enamel, sealing of fissures (indentations of chewing teeth). In what case it is worth carrying out them, the doctor will advise.
When the time comes for the permanent teeth to erupt, the roots of the milk teeth gradually dissolve - therefore they are removed easily and painlessly. It is best to ensure that the first teeth last the entire required period, then the risk of problems with permanent teeth will be less.
Other articles:
- When should you not correct your bite? Temporary and permanent contraindications
- What to choose for a child – braces or aligners?
Is it necessary to treat pulpitis on baby teeth?
Pulpitis is inflammation of the pulp, i.e. nerve and surrounding soft tissues. Sometimes for some reason they believe that pulpitis does not occur in children. But baby teeth also contain nerves and they can become inflamed in the same way. The reasons are:
- advanced caries,
- tooth injury,
- an error in the treatment of caries (the dentin of a baby tooth is very thin and a dentist who does not have much experience in treating baby teeth in children may accidentally open the pulp chamber),
- infectious disease (for example, severe sore throat, as a result of which the infection penetrates the tooth from the inside, through the blood).
Pulpitis in children is uncommon, but does occur. Therefore, it is necessary to treat it. Otherwise, it can become chronic and not only lead to tooth loss too early, but can also transmit inflammation to the new emerging permanent tooth.
Pulpitis in baby teeth is now treated in three ways:
- Classical devital amputation: the diseased nerve is killed with a special paste, after a few days the pulp is removed and the tooth is filled. Now this method is considered outdated, but nevertheless is sometimes used.
- Vital amputation: if only part of the nerve is inflamed, then at the very beginning of the inflammation it is possible to remove the affected part of the nerve under anesthesia, and an antiseptic anti-inflammatory agent is applied to the rest and the tooth is filled. The operation is complex and leaves the possibility of re-inflammation of the pulp.
- Vital pulp extraction: under strong anesthesia, the inflamed pulp is completely removed and the pulp chamber is filled with a special zinc-eugenol paste, which in the future will be absorbed along with the roots of the baby tooth. The method is effective, but expensive and requires a highly qualified dentist.
Much more often, doctors suggest simply removing a baby tooth affected by pulpitis. This is both simpler and cheaper, but, unfortunately, there is a possibility of displacement of adjacent teeth (if the permanent tooth does not erupt soon), which can lead to the formation of a malocclusion. To avoid such a situation, it is best not to let the situation develop into pulpitis, but to treat caries as early as possible.
Treatment of ureaplasma infection of the urogenital tract
Ureaplasma infection can only conditionally be classified as a sexually transmitted infection. The fact is that the causative agent is Ureaplasma urealyticum from the mycoplasma family, which can actually live in the genital tract and be transmitted through sexual contact. However, the role of ureaplasmas, like other mycoplasmas, with the exception of M. genitalium, in the occurrence of an inflammatory reaction is quite ambiguous, as a result of which most authors, especially abroad, classify this pathogen as opportunistic. And in ICD-10, the internationally recognized list of diseases, such a disease as ureaplasmosis or ureaplasma infection is not listed. Meanwhile, a number of researchers provide quite convincing evidence in favor of the pathogenicity of this infection. Not so long ago, a doctoral dissertation was even defended in Moscow, the author of which defended precisely this point of view.
In 1954, Shepard first discovered U. urealyticum in secretions obtained from a patient with urethritis and named them T-mycoplasmas (from the English word tiny - tiny). In terms of their size, ureaplasmas are one of the smallest representatives of the bacterial flora detected in humans, and by the type of their life activity they are classified as intracellular parasites.
There are two known biovars of ureaplasma - Parvo and T960, which are divided into 14 serovars. Recent advances in molecular biology in the study of DNA and ribosomal RNA of ureaplasmas allowed some authors (F. Kong et al., 2000) to abandon the classical classification and divide all ureaplasmas into two species - Ureaplasma urealyticum (former biovar T960) and Ureaplasma parvum (former biovar Parvo ).
As mentioned above, the question of the role of ureaplasma in the etiology and pathogenesis of diseases of the urogenital tract has not yet been resolved. They are too widespread, and too often these microorganisms are detected in individuals who do not have clinical symptoms. Authors who classify ureaplasmas as obligate pathogens believe that they cause urethritis, cervicitis, prostatitis, postpartum endometritis, pyelonephritis, infertility, and various pathologies of pregnancy (chorioamnionitis) and the fetus (pulmonary pathology). Other researchers believe that ureaplasmas are part of the opportunistic flora of the urogenital tract and are capable of causing infectious and inflammatory diseases of the genitourinary organs only under certain conditions (in particular, with insufficiency of immunity) or with appropriate microbial associations.
Indicators of infection of the urogenital tract with ureaplasma among the sexually active population vary from 10 to 80%. Ureaplasma is usually found in people who are sexually active, and most often these microorganisms are detected in people who have three or more sexual partners. According to F. Kong et al., Ureaplasma parvum is detected in 81-87% of patients and Ureaplasma urealyticum in 13-19%. The clinical picture of the inflammatory process in which ureaplasma is detected does not have pathognomonic symptoms.
The authors of some works argue that it is ureaplasmas that are often the cause of adverse pregnancy outcomes and aggravate the risk of premature birth and death in the birth of children with very low body weight.
The question of the influence of ureaplasma on human reproductive function remains open. Meanwhile, female infertility may be associated with inflammatory processes in the genital area induced by ureaplasma, leading to disruption of the passage of the egg into the uterine cavity. Male infertility can be caused, firstly, by inflammatory processes, and secondly, by the influence of ureaplasma on spermatogenesis. Adsorption of ureaplasmas on the surface of sperm can change their motility, morphology and chromosomal apparatus.
As with most representatives of opportunistic flora, for ureaplasmas there are a number of factors that contribute to the development of infectious and inflammatory processes. The most important of them are immune disorders, changes in hormonal status, massive colonization, and associations with other bacteria. All these aspects should be taken into account when choosing management tactics for such patients.
Diagnostic methods
- Culture study on selective media. Such a study makes it possible to isolate a culture of the pathogen within 3 days and separate ureaplasmas from other mycoplasmas. The materials for the study are scrapings from the urogenital tract and the patient’s urine. The method makes it possible to determine the sensitivity of isolated pathogens to various antibiotics, which is very important given the frequent antibiotic resistance today. The specificity of the method is 100%. This method is used for the simultaneous detection of Mycoplasma hominis and Ureaplasma urealyticum.
- Detection of pathogen DNA by PCR. The study allows one to identify the pathogen in a scraping from the urogenital tract within 24 hours and determine its species.
- Serological tests. Allows you to determine the presence of antigens and specific antibodies to them in the blood. They can be useful in case of recurrent course of the disease, with the development of complications and infertility.
Like the problem of the pathogenicity of ureaplasmas, the question of the need to eliminate these pathogens from the urogenital tract also remains open. Most often, the authors suggest taking measures to eliminate these microorganisms if a person has an infectious-inflammatory process at the site of their detection (urethritis, prostatitis, cervicitis, vaginitis), as well as in case of infertility, miscarriage, inflammatory diseases of the pelvic organs, chorioamnionitis, postpartum febrile conditions in the presence of ureaplasma in the genitourinary tract.
Etiotropic treatment of ureaplasma infection is based on the use of antibacterial drugs of various groups. The activity of drugs against any infection is determined by the minimum inhibitory concentration (MIC) in in vitro studies. BMD indicators, as a rule, correlate with the results of clinical cure. It would seem that the optimal drugs should be antibiotics with the lowest MIC, but the importance of such parameters as bioavailability, the ability to create high interstitial and intracellular concentrations, tolerability and compliance of treatment cannot be discounted.
Ureaplasmas are resistant to β-lactam antibiotics (penicillins and cephalosporins), due to the fact that they lack a cell wall, and sulfonamides, since these microorganisms do not synthesize acid. In the treatment of ureaplasma infection, those antibacterial agents that affect protein and DNA synthesis, i.e., those that have a bacteriostatic effect, can be effective. These are tetracycline drugs, macrolides, fluoroquinolones, aminoglycosides, chloramphenicol and some others (see Table 1).
As can be seen from the table, doxycycline and clarithromycin have the best MIC indicators, in addition, they are highly active against ureaplasma. Other drugs have selective activity and their choice is determined depending on the results of microbiological studies.
Tetracyclines
Of the tetracycline antibiotics, doxycycline and minocycline are the most convenient to use, since they, unlike other drugs in this group, can be used 1-2 times a day. Currently, minocycline is not registered in the Russian Federation.
According to the 1998 methodological recommendations and the Federal Guidelines for the Use of Medicines, for ureaplasma infection it is recommended to prescribe doxycycline (Unidox Solutab, Vibramycin, Medomycin). The drug is prescribed 100 mg 2 times a day for 7-14 days. Usually, when you first take an antibiotic, the dose is doubled. According to the recommendations of the American Centers for Disease Control and Prevention (CDC), doxycycline, along with erythromycin and ofloxacin, is the drug of choice for the treatment of nongonococcal urethritis (NGU). Less convenient for the patient is a course of tetracycline, which is used at a dose of 500 mg 4 times a day for 7-10 days.
Doxycycline is used in the form of two salts, depending on whether the antibiotic is used in capsule or powder form. Capsules use doxycycline hydrochloride or hyclate. The powder for other oral forms is doxycycline monohydrate. The use of monohydrate salt instead of hydrochloride eliminates the occurrence of esophagitis. The most convenient to use is the dosage form Solutab.
Due to its special pharmacokinetic properties, doxycycline is much better tolerated than tetracycline.
Good results were obtained when administering doxycycline to women infected with various mycoplasmas (including ureaplasmas) and suffering from infertility or recurrent miscarriage. After sanitation from mycoplasmas, in a number of cases pregnancy occurred, which ended in normal birth on time and without complications.
It should be noted, however, that from 2 to 33% of ureaplasma strains can be resistant to tetracycline. Other significant disadvantages of tetracycline drugs include contraindications for their use in pregnant women and children under 8 years of age, a high incidence of adverse reactions from the gastrointestinal tract, as well as photosensitivity of the skin during their use.
Macrolides, lincosamines, streptogramins
Of the drugs from the group of macrolides, azalides, lincosamines and streptogramins, the most preferred are clarithromycin, josamycin, azithromycin, midecamycin and erythromycin.
As mentioned above, clarithromycin has the best MIC of all macrolide antibiotics, which has all the advantages of modern antibiotics belonging to this class: good tolerability, low frequency of adverse reactions and high compliance.
Clarithromycin (Clabax, Klacid) is prescribed 250 mg 2 times a day, and in the prolonged form of CP 500 mg 1 time a day, for 7-14 days.
Josamycin (vilprafen) 500 mg 3 times a day for 7-14 days.
Azithromycin (azitral, sumamed, hemomycin) is prescribed 250 mg once a day for 6 days or 1 g once.
Midecamycin (Macroene) - 400 mg 3 times a day for 7-14 days.
Erythromycin (erythromycin, erifluid) 500 mg 4 times a day for 7-14 days.
Roxithromycin (Roxide, Roxithromycin, Rulide) 150 mg 2 times a day for 7-14 days.
When taken orally, clarithromycin, unlike erythromycin, is stable in the acidic environment of the stomach, and therefore is prescribed regardless of food intake. This parameter also has a positive effect on the bioavailability of the drug. The elimination period of the main substance is about 3.5-4.5 hours, its metabolites - 7.5-8.5 hours. This determines the fast, powerful and prolonged action of clarithromycin in comparison with erythromycin. The most important aspect of the mechanism of action of clarithromycin, especially relevant when it comes to the treatment of ureaplasma infection, is its high ability to penetrate into cells. The drug actively accumulates in lymphocytes, leukocytes and macrophages, resulting in its high tissue concentration in the affected organs. Absolute bioavailability is more than 50%. The content in tissues is usually several times higher than in serum. Clarithromycin is an inhibitor of bacterial regrowth, which causes a pronounced post-antibiotic effect. To date, there are no reports of ureaplasma resistance to clarithromycin.
Due to the high MIC of ureaplasma, they are practically resistant to lincosamines - lincomycin and clindamycin, as well as to the “old” macrolides - oleandomycin and spiramycin.
During pregnancy, it is not advisable to prescribe azithromycin, roxithromycin, clarithromycin and midecamycin. For the treatment of pregnant women with ureaplasma infection, it is recommended to use erythromycin orally at a dose of 500 mg every 6 hours for 7-10 days. It has been shown that after such treatment the threat of miscarriage, the frequency of spontaneous abortions and the phenomenon of polyhydramnios are reduced.
Josamycin is also recommended for the treatment of pregnant women. It is highly effective, without causing adverse reactions from the liver, and does not affect the metabolism of other drugs. However, the effect of josamycin on the natural bacterial flora is small.
At the birth of children infected in utero with ureaplasma, therapy with erythromycin is also carried out. Preferably, intravenous drip administration of the drug at the rate of 20-40 mg per 1 kg of body weight.
Fluoroquinolones
All mycoplasma species are highly sensitive to new fluoroquinolones, especially ofloxacin. Its leading position in this group is due to its wide antibacterial spectrum of action, high bactericidal activity, good pharmacokinetic characteristics (rapid absorption, high concentrations of the drug in tissues, cells, biological fluids), low toxicity.
Ofloxacin (Zanocin, Oflo, Taricin) is prescribed 200 mg 2 times a day for 7-10 days, pefloxacin - 600 mg 1 time a day for 7-10 days, moxifloxacin (Avelox) 400 mg 1 time a day within 10 days.
It should be noted that antibiotic sensitivity studies of ureaplasmas show their frequent resistance in clinical practice to ofloxacin and other fluoroquinolones.
As in the case of tetracyclines, drugs of this group are undesirable for use in pregnant women; they also cause photosensitivity.
Ureaplasmas are moderately sensitive to aminoglycosides and chloramphenicol. Of the aminoglycosides, the most effective is gentamicin, which is administered parenterally at a dose of 40 mg every 8 hours for 5 days. Streptomycin and kanamycin are practically ineffective for ureaplasma infection.
In recent years, both in our country and abroad, cases of detection of mycoplasmas genetically resistant to tetracycline (up to 40%), erythromycin, spiramycin (up to 30%) and ciprofloxacin have become more frequent.
To select an adequate treatment regimen in specific cases, laboratory determination of the sensitivity of isolated ureaplasma cultures to various antibiotics is recommended. However, many authors note the ability of ureaplasmas to quickly acquire resistance to antibacterial drugs when they are passaged in vitro. Therefore, testing of strains freshly isolated from diseased individuals is necessary. Another complication is that antibiotic sensitivity in vitro does not necessarily correlate with benefit in vivo. This may be related to the pharmacokinetics of the drugs. An analysis of studies on the treatment of ureaplasma infection shows an extremely wide range in the effectiveness of various antibiotics - from 40 to 100%. In independent studies, the criterion for the effectiveness of a particular antibiotic for ureaplasma infection rarely exceeds 80%.
In some cases, etiotropic therapy may be part of combination therapy, in particular immunotropic therapy. In the work of Hadson MMT et al. (1998) reported on the importance of the patient’s immunological status during ureaplasma infection. Since antibiotics active against ureaplasma have a bacteriostatic rather than bactericidal effect, the patient’s immune response plays a decisive role. The use of immunotropic therapy may be especially relevant if at least one course of antimicrobial treatment is ineffective.
Our own studies have shown that when choosing immunotropic therapy, the drug Immunomax demonstrated particularly high effectiveness.
This drug belongs to the group of immunomodulators and is indicated for the correction of weakened immunity, treatment and prevention of viral and bacterial infections.
When there are indications for combination therapy for ureaplasma infection, patients are prescribed an antibiotic simultaneously with intramuscular injections of Immunomax. We used Immunomax 200 units simultaneously with a 10-day standard course of antibacterial therapy with doxycycline or clarithromycin on days 1-3, 8-10 of treatment. Injections were performed once a day, for a course of 6 injections. In 20 out of 23 (87%) patients, when diagnosed 2 weeks after the end of treatment and after 3 months of follow-up, no ureaplasmas were detected.
Summarizing the above, we can state that when treating patients with ureaplasma infection, among all antibiotics, preference should be given to doxycycline from the tetracycline group, clarithromycin from the macrolide group, and josamycin during pregnancy.
The most successful combination for cases of ureaplasma infection that are resistant to standard etiotropic therapy, as well as for recurrent course of this infection, is the use of antibiotics in combination with immunotropic treatment, which makes it possible to eliminate the pathogen and avoid relapses of the infection.
M. A. Gomberg, Doctor of Medical Sciences A. M. Solovyov, Candidate of Medical Sciences TsIKVI, MGMSU, Moscow
Sensitivity of ureaplasmas to various antibacterial agents (MIC in µg/ml)
| Antibiotic | IPC |
| Tetracyclines | |
| Tetracycline | 0,05 — 0,6 |
| Oxytetracycline | 0,5 — 62 |
| Chlortetracycline | — |
| Doxycycline | 0,01 — 1,0 |
| Minocycline | 0,5 — 62 |
| Macrolides, lincosamines, streptogramins | |
| Erythromycin | 0,12 — 3,0 |
| Oleandomycin | 5,9 |
| Spiramycin | 16,0 — 41,9 |
| Josamycin | 0,02 — 0,45 |
| Midecamycin | 0,06 — 0,6 |
| Clarithromycin | 0,015 — 1,0 |
| Roxithromycin | 0,06 — 1,0 |
| Azithromycin | 0,12 — 1,0 |
| Lincomycin | 73 |
| Pristinamycin | 0,1 — 1,0 |
| Clindamycin | 2,62 |
| Fluoroquinolones | |
| Ofloxacin | 1,0 — 4,0 |
| Ciprofloxacin | 0,25 — 0,1 |
| Norfloxacin | 2,0 — 4,0 |
| Lomefloxacin | 2,0 — 8,0 |
| Pefloxacin | 4,0 — 8,0 |
| Aminoglycosides | |
| Streptomycin | 0,4 — 12,5 |
| Kanamycin | 1,6 — 50 |
| Gentamicin | 0,4 — 6,2 |
| Other groups | |
| Levomycetin | 0,5 — 6,2 |
Is it worth treating baby teeth under anesthesia (sedation)
Despite the fact that many parents consider baby teeth to be fake (or, on the contrary, by nature more protected) and underestimate the problems that arise with them, it is still painful to treat baby teeth - just like molars. Therefore, it is important to contact pediatric dentistry, since the requirements for anesthetics for children are more stringent, and the necessary drugs may not be available in a regular “adult” clinic.
In many cases, treating baby teeth under anesthesia is not only possible, but also necessary. A distinction must be made between anesthesia and sedation. Sedation is the process of calming a small patient, relieving excessive agitation or fear before dental procedures. It is achieved with mild, safe means (for example, nitrous oxide) and is not accompanied by pain relief.
Anesthesia involves the patient falling asleep and dental treatment in his sleep. For children, the use of two drugs is allowed: sevoran, administered through a special mask, and propofol, administered intravenously. These are safe, well-tested products that are highly effective and do not affect the child’s nervous system.
Anesthesia is used in cases where it is difficult for the doctor to establish contact with the child, or there is a pathological fear of dental procedures. And also when a voluminous or complex intervention is expected: removal of several teeth, treatment of deep caries or pulpitis, etc. It is very difficult for a preschool child (or primary school student) to sit motionless in a chair for more than 20-30 minutes, and anesthesia will allow him to receive the necessary treatment in full, completely unnoticeably and painlessly.
Methods for treating caries in children - without pain and fear
There are many methods available for the treatment of caries in primary teeth. All of them are adapted for children and do not cause pain, discomfort or anxiety to the child. Depending on the complexity of the situation, dentists offer the following solutions:
- Remineralization of tooth enamel – restoration of a balanced structure of the tooth surface using special pastes. Formulas with a high content of calcium and sodium should be applied to baby teeth for some time, which will stop the spread of bacteria and the deepening of carious cavities.
- The ICON method is an ideal treatment option for superficial caries. The doctor applies a composition to the carious spot to remove the affected area of enamel, and then closes the cavity with a safe, quick-hardening polymer. The treatment takes place without a drill - quickly and painlessly.
- Ozone therapy is an effective method of combating caries. The damaged area is subjected to targeted exposure to ozone to disinfect the enamel and eliminate carious bacteria. Children tolerate the procedure very well, as it does not cause any discomfort.
- Filling. Cleaning carious cavities is done using a drill or manually without drilling. Next, the doctor treats the tooth with antiseptics and places a filling - white or colored. Treatment of caries of a baby tooth is carried out with anesthesia with local anesthetics or under sedation.
- Laser dental treatment. Advanced technology in which laser beams remove carious lesions quickly and accurately. A filling is placed on the cleaned and disinfected cavity.
A method for treating caries is suggested by the doctor after assessing the degree of damage to the baby tooth.
At what age should children have their baby teeth treated?
It is necessary to treat baby teeth at any age. In the first years, when baby teeth erupt, children are often limited in sweets and caries develops infrequently. At the age of 3-5 years, the situation becomes more complicated due to the fact that sweets become more accessible, and teeth brushing is often carried out irregularly and without due diligence.
At about 5-6 years old, baby teeth begin to be replaced by permanent ones. Usually this process is completed by the age of 14, although deviations in one direction or another are often encountered. It makes no sense for parents to wait for a certain time to start seriously taking care of their child’s teeth and taking him to the dentist. As we have already said, diseases of baby teeth can lead to their untimely loss and even cause damage to future permanent teeth. Decayed and prematurely lost baby teeth can cause problems with diction, prevent a child from chewing food normally, and cause digestive problems.
Therefore, from the very beginning, it is important to accustom children to regular oral hygiene, limit their insatiable love for sweets, and periodically take them for preventative visits to the dentist. In order for children not to be afraid of the dentist, it is important to choose a good clinic that employs pediatric dentists, with experience in treating primary teeth and attentive attitude towards young patients. If a child knows that a visit to the dentist does not necessarily mean that their teeth will be drilled, then they will be able to accept these regular visits with greater peace of mind, and their smile will always be flawless.
Prevention is the best solution
So that you do not have to worry about treating or removing baby teeth, organize proper nutrition for your child and oral care.
Try to prevent your baby from consuming a lot of sweets; if possible, reduce the amount of sweet juices and carbonated drinks in the diet. And, of course, take care of regular and proper brushing of your teeth.
The child should brush his teeth 2 times a day: morning and evening. At the same time, do not allow any snacks after brushing your teeth in the evening. If your child is under two years old, brush his teeth yourself. At this age, by the way, be sure to use special toothpastes recommended for children over 0 years old, for example, ASEPTA baby.
Older children should brush their teeth themselves, but always under adult supervision. From the age of two, also visit the dentist at least 2 times a year. This is the only way you can prevent the development of serious dental diseases and ensure timely resolution of all emerging problems.
Is it true that baby teeth don’t have nerves and don’t hurt?
Baby teeth are no different from permanent teeth. They have both nerves and roots (by the time they are replaced with permanent teeth, they resolve on their own). Of course, this is why it is very important to treat them with anesthesia. True, baby teeth, even with significant destruction, may actually not hurt for a long time, this is due to the peculiarities of their structure. But over time, they too can get sick. Therefore, in no case should you wait for this, since it is always more difficult to treat a child with acute pain - he is under stress, and there is absolutely no time to adapt. It is possible that the tooth will hardly be cured; it will have to be removed.
Features of treatment of children's teeth
Dental treatment in childhood requires compliance with a number of features. The methods are similar to those used for adults, but there are some differences. In general, pediatric dentistry is a separate “world” in which only experienced doctors who know how to approach children work. This requires a lot of experience and communication skills with young patients, since in some cases you have to try hard to calm the child down and carry out treatment in a favorable environment for him.
How to treat teeth at 1 year old
The first visit to the dentist is recommended at the age of one year. During the initial appointment, the specialist carefully examines not only the milk teeth, but also the frenulum of the lips and tongue. A visit to the doctor at this age is extremely necessary to promptly detect and then eliminate:
- bite defects;
- frenulum abnormalities;
- gum pathologies and other possible disorders.
If any diseases are discovered during the examination, the specialist prescribes treatment. If there is an assumption that manipulations may cause pain or discomfort to the child, anesthesia is used.
How to treat teeth at 2–3 years old
At the age of two to three years, for preventive purposes, the child should be taken to an appointment not only with a dentist, but also with a hygienist, since during this period most children usually erupt all their milk teeth, and they require special care. At the initial appointment, the doctor examines the oral cavity and assesses the correctness of the bite. In addition, all baby teeth are checked for cavities.
Most often, at 2–3 years of age, caries is diagnosed at the “spot” stage, when deep tissue structures have not yet been affected. In this case, two treatment methods are usually used:
- Remineralization.
The procedure is painless and performed without anesthesia. The method is based on the use of special compounds based on fluorine, calcium and phosphorus. The product is applied directly to the affected area and allows you to restore the mineral balance of the tooth.
- Silvering.
During the procedure, the teeth are coated with a special silver-based compound, which protects the enamel for a long time and prevents the re-development of caries.
Most often, using such methods, the stain is removed without instrumental intervention. If caries has affected deeper layers, it is impossible to do without removing the affected tissue, cleaning and filling.
How to treat teeth at 4–5 years old
If during diagnosis the doctor discovers caries, the most common disease at this age, treatment is prescribed according to the following algorithm:
- treatment of the oral cavity with antiseptic drugs;
- applying “freezing” agents to the gums in the area where the anesthetic was administered;
- injection administration of anesthesia;
- removal of affected tissue using special tools or a drill;
- filling.
The whole process takes about 30–40 minutes, sometimes more depending on the size and severity of the caries, and the child does not feel anything, since the procedure is carried out only after the anesthesia has taken effect.
If gum disease is diagnosed, topical agents are most often prescribed - ointments, creams, gels, as well as rinsing the mouth with pharmaceutical solutions or tinctures of medicinal herbs. In severe forms of pathologies, medications can be prescribed that eliminate inflammation and relieve painful symptoms.
How to treat teeth for children over 5 years old
At the age of 5 to 7 years, the replacement of baby teeth with permanent ones begins. During this period, particularly careful hygiene and regular visits to the dentist are required, as it is necessary to monitor the condition of the enamel, which is formed gradually over 2–4 years.
After 7 years, bite problems often arise. This is due to the fact that instead of a gradual increase in the jaw in proportion to the growth of permanent teeth, some kind of failure occurs, as a result of which anomalies appear - incomplete closure, displacement of the dentition, malocclusion, etc. In such cases, the therapeutic course includes not only wearing braces and other orthopedic structures, but also visiting a speech therapist.
The most common dental diseases in childhood
Among the main problems that force children to undergo dental treatment:
- Caries. Children encounter it most often. The disease is found in more than 60% of children under six years of age. It especially often affects molars. This is due to their relief volumetric surface and the baby’s nutritional conditions. On the crown of molars, plaque is deposited more actively. Pathogenic microorganisms multiply in it. The result of their life activity is progressive caries. The difficulty is that in the first stages, parents are not always able to detect a carious cavity on their own. It looks like a light speck and practically merges with the healthy surrounding enamel. Not knowing about the presence of the disease, mothers and fathers postpone a visit to the pediatric dentist. When the child arrives for an appointment, the carious “hollow” already turns out to be very large.
- Periostitis (flux). A complication of advanced caries, caused by the spread of bacteria, damage to tooth roots and tissues adjacent to them. The cheek is swollen. A voluminous abscess forms on the surface of the gum. When palpated, acute pain occurs. Flux may worsen the baby's general condition.
- Periodontitis. Inflammatory periodontal disease. The latter is formed by: periodontal ligament, gums, root cement and alveolar bone. It hurts your baby to bite into hard food. His temperature rises and headaches appear.
All of these dental diseases are highly treatable. The most important thing is not to put off visiting a dental clinic until later.
Maybe you shouldn’t treat the tooth, but just remove it?
It will be easier to persuade a child to treat a tooth than to remove it. Even under the influence of modern anesthesia, the patient does not lose tactile sensitivity (no pain occurs, but there is rocking and pressure). Children can perceive such sensations as pain. Medical manipulations during dental treatment are much more gentle. Also, with the early loss of one tooth (and especially several), it can cause problems with speech and malocclusion. Do not forget also about the psychological aspect: very often children who do not have front teeth begin to be teased by their peers.