Bad breath is one of the most common complaints with which patients turn not only to the dentist, but also to other specialists (therapist, gastroenterologist, otolaryngologist), since such a problem can be a consequence of a number of diseases.
In scientific and medical circles, special terms are used to refer to bad breath, such as “halitosis” or “ozonostomia”. In ICD-10, bad breath is classified as a clinical symptom related to gastrointestinal diseases and abdominal pathologies, and is designated by code R19.6.
Putrid odor from teeth and gums can also be the result of active growth of anaerobic bacterial flora in the mouth due to infectious and inflammatory dental diseases. If a sharp, unpleasant odor appears from the gums (in the absence of other symptoms), a dental examination and oral sanitation are recommended.
If the problem does not disappear after this, a comprehensive examination of the ENT organs and digestive tract is necessary.
Why does my breath smell bad?
The mechanism of formation of bad breath is represented mainly by the growth of pathogenic flora on the mucous membranes of the gums and the inner surface of the cheeks.
The reasons for this may be different, but the basis of the pathogenetic changes is a violation of the qualitative and quantitative relationship between pathogenic bacteria (some strains of streptococci, Escherichia coli and Pseudomonas aeruginosa, the bacteria Bulleidia moorei) and aerobes that can suppress their activity.
Aerobic microorganisms are microorganisms whose ability to function is active only when exposed to atmospheric oxygen. Both microorganisms are opportunistic for humans and can cause a number of serious diseases (tuberculosis, Lyme disease, streptococcal pharyngitis, etc.), but it is their balance that allows maintaining a normal level of acidity and local immunity of the mucous membranes in the oral cavity.
A pungent odor from teeth and gums in a person who does not suffer from pancreatitis, gastritis, cholecystitis and other pathologies of the digestive system and abdominal organs occurs as a result of excessive synthesis of volatile compounds that can penetrate into the environment in significant concentrations. Such compounds are secreted by representatives of the anaerobic flora, feeding on food debris contained in dense dental plaque and deposits, therefore, one of the leading factors in the development of ozonostomy is rightly considered to be the low quality of oral hygiene.
Swelling
Swelling may appear after gum injury. In this case, it is localized, extends only to the site of the bruise, may hurt a little, but in general it goes away quickly. If after an injury the swelling persists for a long time, intensifies, the pain becomes acute or throbbing, you need to consult a doctor.
In other cases, swelling of the gums is a symptom of inflammation. It is accompanied by pain, bleeding may appear, the color of the mucous membrane changes (it becomes darker or acquires a bright red tint). Such swelling may accompany gingivitis or periodontitis.
What could the smell be?
The cause of halitosis can be guessed by the specific odor a person emits into the environment.
Types of volatile compounds and their relationship with bad breath
| Substances produced by bacteria in the mouth | What smell do they have? |
| Methanethiol (poisonous, colorless gas) | Rotten cabbage (even in minimal concentrations). |
| Allyl mercaptan | Garlic, rotten onions. |
| Propyl mercaptan | Pungent smell of rot. |
| Dihydrosulfide | Rotten eggs. |
| Dimethyl sulfide (organic volatile liquid) | Pungent smell of sulfur and petroleum products (gasoline). |
| ?-pentamethylenediamine | The smell of a decomposing corpse, the pungent smell of urine. |
| Indole and its derivatives | Naphthalene. |
| Ammonia derivatives | Feces (feces). |
| 1,4-diaminobutane | Spoiled meat. |
| Dimethylamine | Rotten fish. |
| Methylbutanoic (isovaleric) acid | Sour milk. |
Note! All the compounds listed in the table are produced primarily by pathogenic microorganisms, so dentists cite poor-quality hygienic care and dental diseases (especially chronic ones) as the main causes of unpleasant gum odor.
Dental reasons
If a putrid odor from the gums appears suddenly, the first thing to do is consult a dentist and rule out the presence of caries, inflammatory processes in the gingival and periodontal tissues, hilar cysts and granulomas, and abscesses. It is almost impossible to independently identify the source of bad breath (gums or teeth), so dental diagnostics are carried out comprehensively and often include not only a visual examination using a medical mirror, percussion of the teeth (if periodontitis is suspected), but also an X-ray or computed tomographic examination.
The causes that can provoke halitosis include a number of pathologies and diseases.
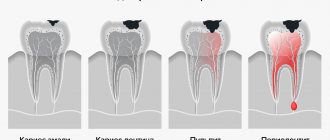
- Caries. This is the most common disease among all age populations, in which the hard tissues of the tooth are affected and necrotically modified. The causes of caries are dysbacteriosis, poor hygiene, lack of sufficient preventive measures, chronic infections (especially diseases of the ENT organs). A pungent odor from the gums and teeth with stage 3-4 caries appears in almost 100% of patients and is perceived by others as the smell of rotting food, feces or urine.
- Inflammatory and infectious gum diseases. This group includes infectious and non-infectious pathologies of the oral cavity, in which soft tissues (gums and tongue) are involved in the inflammatory process. These are stomatitis, gingivitis, desquamative glossitis, pharyngomycosis of the oral cavity and other diseases whose pathogenesis is based on catarrhal, herpetic, exfoliative, traumatic or eczematous inflammation.
- Periodontal diseases. Periodontium is a special type of fibrous collagen fibers with a low degree of elasticity that fill the space between the alveolar bone and the hilar cementum. One of the complications of periodontitis and periodontitis is the formation of periodontal (periodontal) pockets, into which food can become clogged, undergoing processes of fermentation, fermentation and decay. It is the decay products that cause the putrid odor from the gums in this case.
- Abscesses, cysts of the gums, tooth roots or dental alveoli. Bad breath with cysts may indicate that the cavity is inflamed and filled with purulent exudate, which can be a source of hematogenous spread of infection throughout the body. Treatment for a purulent cyst or abscess is surgical (followed by antibiotic therapy).
One of the causes of bad breath can also be xerostomia, a pathology of the salivary glands, in which an insufficient amount of saliva is produced in a person’s mouth. Saliva is necessary not only to maintain normal levels of moisture and acidity, but also for the primary processing of incoming food due to the action of digestive enzymes. If there is not enough saliva, food enters the stomach poorly processed, which can cause indigestion and the release of bad-smelling gases and acids that rise up the esophagus back into the oral cavity.
Important! If the patient has undergone orthodontic treatment (dental implantation, installation of braces, etc.), in addition to a dental examination, an orthodontist consultation is also indicated to exclude galvanic syndrome - poor survival or intolerance of installed dentures.
Factors of destruction of a molar, incisor or canine
Installing a crown does not provide a 100% guarantee of the safety of a molar, canine or incisor.
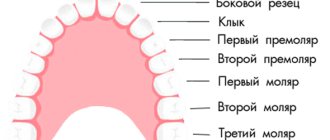
Photo 1. Names of teeth
Under the influence of unfavorable factors, they begin to collapse even under a prosthesis. Possible reasons:
- Thermal – temperature changes adversely affect not only the enamel, but also the material of the prosthesis.
- Mechanical - the formation of cracks when chewing solid food.
- Chemical - crowns are made of inert material, but with prolonged exposure to aggressive substances they begin to deteriorate.
- Poor hygiene.
- The general condition - lack of nutrients, calcium, fluoride - leads to the fact that the tooth begins to decay under the crown.
- Infection - the causes are either poor quality work of the dentist, or a severe form of any bacterial, viral or fungal disease.
What other reasons can cause ozonostomy?
If an examination by a dentist does not reveal any diseases or pathologies, the doctor will refer the patient to specialized specialists to determine the possible causes. These may include:
- pathologies of the digestive system and abdominal organs (pancreatitis, cholecystitis, gastritis, duodenitis, chronic colitis, irritable bowel syndrome, gastroduodenitis);
- untreated or recurrent infectious diseases of the nasopharynx and oropharynx (tonsillitis, sinusitis, laryngitis, pharyngitis);
- kidney pathologies accompanied by partial dysfunction of the renal system;
- diabetes mellitus (the smell of urine and acetone from the mouth is one of the signs of a lack of insulin);
- long-term use of certain medications that can cause xerostomia (proton pump blockers, heartburn medications, alpha-agonists, etc.);
- abuse of foods with a high content of purines and phytoncides (onions, garlic, green onions, all varieties of cabbage, sorrel);
- smoking (especially if a person smokes more than 10 cigarettes per day).
Often the unpleasant smell of sour milk or rotten eggs appears in women on diets. A prolonged absence of food in the stomach provokes increased activity of parietal cells, which are responsible for the production of hydrochloric acid. As a result, a colorless gas accumulates in the stomach, which is a compound of hydrogen and sulfur and has the characteristic smell of rotten eggs. If food does not enter the stomach, this gas rises to the top and is released into the environment through the mouth when a person talks, yawns or sneezes.
People who are susceptible to emotional instability and are often in a state of prolonged stress experience unpleasant gum odor 2.1 times more often than their peers who are in an emotionally stable state.
Important! A constant smell of rot, feces or urine from the mouth, especially if it intensifies or is combined with other symptoms (sore throat, sensation of a foreign body in the pharynx and esophagus, nausea, discomfort in the stomach, etc.), may be a manifestation of malignant tumors digestive system or larynx. Consultation with an oncologist is indicated in cases where it is not possible to get rid of the unpleasant odor within 3 months, despite a complete examination, sanitization of foci of chronic infection and adherence to personal hygiene measures.
Diagnosis at home
The patient himself very often does not notice that his breath smells bad, and the people around him are embarrassed to say so, for fear of offending a loved one. To independently assess the freshness of your breath and the intensity of odors, you can perform one of the tests below. All of them are simple to perform and do not require the help of outsiders or any special equipment or tools.
Method 1
This method requires floss (dental floss) without adding flavoring or coloring additives.
- Clean the interdental spaces using the classic method. To assess the freshness of breath, it is necessary to treat molars (molars).
- After the procedure, carefully examine the color of the floss. The presence of a yellowish, light brown or creamy tint indicates a large amount of bacterial plaque on the inner surface of the tooth enamel. If a pinkish tint appears on the thread, you should check the condition of your gums.
- The smell can be assessed 20-30 seconds after the procedure.
The test cannot be considered reliable if colored or scented thread was used.
Method 2
To carry out this test, you need to use a soft silicone spoon or wooden spatula (can be purchased at a pharmacy).
Using a spatula, remove the plaque from the middle part of the tongue, then wait 10-15 seconds and evaluate the quality and intensity of the smell.
Method 3
This method is the simplest and allows you to carry out express diagnostics in 1 minute, from anywhere. To do this, wash your hands thoroughly with soap and lick the outer surface of your hand (near the thumb) or wrist. You can evaluate the result in 40-50 seconds.
How does a dentist diagnose?
To identify signs of ozonostomy, dentists use the organoleptic diagnostic method. Indicators are measured using special instruments and analyzed in accordance with established standards.
To ensure that the test result is as reliable as possible, 12-20 hours before the doctor’s visit, the patient is recommended to:
- stop smoking and chewing gum;
- do not use hot spices, seasonings, seasonings and products containing large amounts of flavorings, flavor enhancers and dyes;
- discontinue antimicrobial treatment (48 hours before the test), if possible;
- Do not use tooth balms or rinses.
Note! You cannot brush your teeth before the procedure. The last brushing of teeth is allowed 8-10 hours before the test.
Main symptoms
The main sign of pathology is the appearance of blood while eating or brushing teeth. When gums become inflamed, they become more vulnerable to injury, their capillaries become highly permeable, and the tissue becomes thinner, so bleeding occurs much more easily. Additional symptoms depend on the specific disease. Most often, bleeding is accompanied by the following symptoms:
- unpleasant odor;
- swelling of the mucous membrane;
- the appearance of a metallic taste;
- redness of the gums, formation of white plaque;
- exposure of the neck of the tooth;
- discomfort when brushing teeth or pressing on the gums;
- uneven height of the gingival margin.
If these signs appear, it is advisable to immediately consult a doctor. It is much easier to treat bleeding gums at an early stage than in an advanced form.
How to deal with the smell?
Treatment of halitosis and its manifestations consists of complete sanitation of infectious foci. The patient is treated for carious cavities with the installation of fillings and cleaning of the canals. If the tooth cannot be saved, extraction is prescribed (installation of dentures is permissible only after high-quality sanitation and oral hygiene). For infectious or inflammatory pathologies, a course of local treatment (application, rinsing with antiseptics, instillation), antibiotic therapy and antimicrobial therapy is carried out.
For recurrent gingivitis, the doctor may prescribe Metronidazole at a dosage of 100-200 mg 2-3 times a day. The standard course of treatment is 7-10 days. In more severe cases, antibiotics are indicated - amoxicillin, tetracycline, cephalosporin. Local applications are made with medicinal ointments and gels, some of which can be placed directly into periodontal pockets (Cholisal, Metrogil Denta, Asepta, Kamistad).
For fungal infections (candidal stomatitis, pharyngomycosis), systemic and local antimycotics are used - Fluconazole, Candide, Miconazole. In all cases, rinsing with antiseptics (Miramistin, chlorhexidine, furatsilin solution) is indicated.
Important! To treat unpleasant odor caused by diseases of the digestive system, upper and lower respiratory tract, abdominal organs, complex medical, physiotherapeutic and surgical (if necessary) treatment is prescribed: rehabilitation of foci of chronic infection in case of sinusitis, pharyngitis, treatment of gastritis, correction of IBS.
What is gum disease
This is a lesion of periodontal tissues, that is, the tissues surrounding the tooth. This general definition combines deep and superficial inflammatory processes.
Damage to soft tissue occurs gradually. At the initial stage, only the marginal part of the gum is inflamed. If the inflammation is not cured at this stage, the infection penetrates deeper, the deeper layers of the periodontium are affected, and the disease becomes severe.
Prevention
The main measure to prevent bad breath in patients of any age is high-quality oral hygiene and timely treatment of dental diseases. The tips and recommendations below can be used both to prevent halitosis and to improve the effectiveness of its treatment.
- It is necessary to carry out hygienic treatment of the oral cavity at least 2 times a day. You should brush your teeth immediately after waking up in the morning, and after your last meal in the evening.
- If you are prone to bleeding and the deposition of bacterial plaque, you should additionally use balms and rinses with medicinal herbs and natural antiseptics (Forest Balsam, Listerine, Asepta). Such products should be used in courses - 2-3 weeks every 3-4 months.
- Incorrect or irregular nutrition can provoke the appearance of an unpleasant odor, so it is important to adjust your diet and habits.
- After eating, you should rinse your mouth with boiled water so that there are no pieces of food left in it, which are a breeding ground for bacteria.
Persons who practice oral sex should brush their teeth (at a minimum, thoroughly rinse your mouth with water or mouthwash) after each contact.
Video - 10 ways to combat halitosis
Foul odor from gums is a common dental problem that can only be solved with an integrated approach. Treatment should begin with a visit to the dentist and a complete sanitation: removal of necrotic tissue, relief of inflammatory processes, extraction of teeth that cannot be treated or restored. If the cause of halitosis is diseases of the gastrointestinal tract or larynx, treatment also involves the sanitation of existing infectious foci. Any local remedies (oral sprays, rinses, chewing gums) only mask the problem for a short time, but do not solve it completely, creating conditions for the development of possible complications.
Medicines
The choice of medications is determined based on the type and stage of the disease. Miramistin, chlorhexidine, furatsilin can be used for rinsing the mouth. In the presence of inflammation, you can use ointments that have anti-inflammatory and disinfectant effects. Infections are treated with the following:
- antibiotics;
- antiseptic drugs;
- antifungal agents;
- immunostimulants;
- vitamins.
Home treatments can be used as aids. Good results are shown by rinsing with herbal infusions of calendula, chamomile, and yarrow. To eliminate pain and strengthen soft tissues, use propolis tincture or a solution of soda and sea salt.