Pain after tooth extraction: how long does it last, and is it normal? These and other questions concern patients after dental procedures. Pain syndrome is normal in several cases: early postoperative period, complex removal, simultaneous implantation.
Normally, pain can persist from several days to a week, and its intensity should decrease. The appearance of symptoms such as increased pain, swelling, inflammation, bleeding or the appearance of purulent exudate is a reason to immediately consult a doctor.
How does a postoperative wound heal?
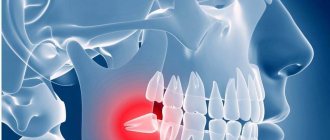
How long the area hurts after tooth extraction depends on many factors. The healing process after tooth extraction is a complex and lengthy process. Removal occurs with a rupture of the dentofacial connection, namely the connection with the alveolar process and the jaw bone.
The recovery process lasts about two to three weeks. Much depends on the surgical protocol, the clinical situation and the characteristics of the body.
Main stages:
- Formation of a blood clot. Forms 1.5-3 hours after extraction. The function of the clot is to protect the wound area from pathogens and secondary infection.
- Active tissue regeneration. The affected mucous membranes are restored, after 3-4 days swelling and inflammation decrease.
- Formation of granulation tissue. After 4-6 days, granulation tissue forms on top of the clot - the basis of a new epithelial layer.
- Granulation proliferation. After a week, the granulation tissue grows, completely covering the socket.
Already on the eighth to tenth day, the wound is completely healed and by the end of the second week a new epithelial layer is formed.
After two weeks, bone tissue begins to renew. After six months, the bone tissue in the area of removal becomes completely healthy.
Causes of pain
The occurrence of pain after tooth extraction is associated with damage to nerve endings, vascular structures and soft tissues. The peak intensity of pain occurs in the first hours after the cessation of anesthesia. The symptom persists for about 12 hours.
In case of incisions in the gums or damage to the bone tissue, as well as after implantation after removal, toothache may persist for 2-3 days. Pain syndrome also occurs in the case of displacement of the dentition towards the formed void. Therefore, doctors recommend prosthetics as soon as possible after extraction.
How to remove formation
Before removing the cyst, the dentist will prescribe additional procedures that will help safely get rid of the purulent accumulation. To do this, it is necessary to fill the diseased teeth and clean the root canals. Surgical intervention includes the following stages:
- The patient is given an anesthetic.
- The soft tissue is cut to open access to the root of the chewing element and remove the cyst. If necessary, the gums on adjacent teeth are cut.
- The cortical plate is removed using a drill. As a result, the doctor has the opportunity to get to the root of the tooth on which the tumor has formed.
- Resection of the root apex is performed, while the tooth structure is preserved and the cyst is removed.
- If the removal is successful, the doctor cleans the root canal. Cleaning helps neutralize residual pus and infection that cause inflammation.
- A bone-like substance is installed to completely restore the structure of the damaged unit of the dentition.
After this, the doctor schedules an appointment to conduct an examination and determine the presence or absence of complications after cystectomy. During the examination, the specialist determines whether the tumor has begun to develop again.
Pain during difficult removal
The duration of pain after complex extraction (wisdom teeth, impacted or dystopic incisors) is associated with damage to a larger tissue area. Often such an operation involves making an incision in the gum, sawing out the roots, extracting tooth fragments, and draining an abscess, which increases the scope of the surgical intervention. If your ear hurts after wisdom tooth removal, this may indicate nerve damage.
In some cases, patients complain of persistent discomfort and pain for up to a week. Clinical manifestations such as swelling, swelling of the gums, enlarged submandibular lymph nodes, fever, and malaise are also common.
Dangerous complications of long-term pain
Ignoring pain and tissue swelling can lead to serious complications that may require surgery.
When the inflammatory process is advanced, purulent foci form in the tissues, increasing the risk of pus spreading through the bloodstream throughout the body. The development of phlegmon and destruction of the jawbone is likely. With a hematoma, a thickening of the clot may occur, which will inevitably lead to the need for surgical intervention, the appearance of scars and an increase in recovery time.
Types of pain
The nature and type of pain depends on the type and surgical intervention, the duration of the operation, and the complexity of the clinical process. Clinicians distinguish the following types:
- Aching. It is felt immediately after the anesthesia wears off. Keeps for about 2-4 days. The jaw may ache when opening the mouth or chewing.
- Intense, enduring. Occurs during extraction of a complex tooth with drainage or opening of a purulent cavity.
- Phantom. Occurs after traumatic surgery and may be felt from time to time. Phantom pain occurs with weak immunity and a low pain threshold.
It is difficult to say how intense the pain will be in each specific case, which is why it is so important to follow medical recommendations to prevent complications.
What else can pain indicate?
Severe pain after removal may indicate the development of complications. Pulsating pain that radiates to the ears and submandibular lymph nodes is not normal. The most common causes of complicated postoperative pain are the following factors:
- Violation of treatment protocol. Unfortunately, mistakes do occur, especially in the removal of complex teeth. The techniques and approaches used in different clinics may differ from the standards. Errors include leaving fragments of materials or a splintered tooth root behind.
- Alveolitis. Occurs in the absence of a blood clot. The disease complicates natural healing and interferes with normal tissue regeneration. That is why doctors do not recommend touching the wound with your tongue or rinsing your mouth intensively.
- Dry hole. One of the common complications and the cause of long-term pain after tooth extraction. Despite the moisture of the mucous membranes, bone tissue is visible at the bottom of the wound opening. This problem is typical for smokers during periods of hormonal surges. The doctor seals the wound with a swab containing medication.
- Trigeminal neuritis. Long-term pain persists when a tooth in the mandibular row is removed if the trigeminal nerve is damaged during the manipulation. Damage may be accidental due to structural anomalies or multiple branching of nerve structures.
The likelihood of complications developing is low if the removal protocol, medical recommendations after extraction, and timely response to alarming manifestations are followed.
When deletion is indicated
Modern dentistry strives to preserve teeth and their roots whenever possible, but this is not always possible. Dental surgeons remove teeth with cysts for the following indications:
- the infectious process was caused by an advanced form of periodontal disease;
- there is a vertically located crack on the root of the tooth or on itself;
- the dental root canals are impassable, as a result of which therapeutic treatment becomes impossible;
- severe tooth decay, and restoring it does not make sense (too expensive and time-consuming);
- the tooth is located entirely in the cavity of the neoplasm;
- the cyst has grown into the nasal cavity, or the size of the tumor is more than 10 mm;
- the root of the tooth has fused with the neoplasm;
- the tooth is very loose.
The dentist decides to remove a tooth with a cyst after a thorough examination of the patient, which includes examination, history taking, radiography or visiography.
How can you reduce pain?
In the early postoperative period, it is important to follow basic recommendations that reduce the risk of negative manifestations:
- maintain the integrity of the blood clot - do not touch the wound with your tongue, rinse vigorously with solutions or water, just take an antiseptic or herbal decoction into your mouth, hold for a few minutes and spit;
- after a complex removal, take broad-spectrum antibiotics - this is important to prevent the infectious process;
- taking symptomatic medications for up to 2-3 days - in the first days, medications help reduce pain and inflammation;
- use a gel with a cooling effect for intense pain;
- do not eat for two hours after surgery, and eat solid food in the area of manipulation for 5-7 days.
You can reduce the pain if you chew a piece of ginger or propolis on the healthy side of the jaw, apply ice through a handkerchief to your cheek or chin, and rinse with the following ingredients:
- tea tree (10 drops per 500 ml of boiled water);
- steep chamomile decoction;
- decoction of eucalyptus and string;
- soda-salt solution (1 tsp soda, 1 tsp salt, 500 ml water).
The temperature of rinsing solutions should be comfortable - neither cold nor hot. Herbal solutions are best used as an alternative 3-5 days after surgery. In the early period, it is better to rinse the wound and oral cavity generously with water-based antiseptics.
The appearance of pain after tooth extraction is associated with trauma to the deep layers of the jaw structures. The tooth can hurt from several hours to 3-7 days, depending on the severity of the clinical situation and the scope of medical intervention. If questionable symptoms or other signs indicating complications appear, it is recommended to consult a doctor.
Tooth cyst (radicular cyst) - symptoms and treatment
Types of treatment for radicular cysts can be divided into conservative, surgical and conservative-surgical.
Conservative treatment
The conservative method is aimed at removing the necrotic neurovascular bundle of the tooth (pulp) and eliminating pathological changes in the bone behind the root apex.
The decayed pulp is removed with special endodontic instruments. Then the root canal is expanded and antiseptic treatment is carried out. Medicinal pastes are introduced into the root canal, which eliminate the microbial flora and restore the affected bone tissue. These pastes are administered for a period from several days to 1–1.5 months. Usually this process is well tolerated, but sometimes the pastes cause an exacerbation of the process with severe pain. To prevent the paste from getting into the mouth, the tooth cavity is hermetically sealed with a temporary filling.
If the inflammation of the bone tissue is eliminated, the root canals are filled with permanent material, and the defect in the hard tissues of the tooth is closed with a filling.
The fact is that there are no microorganisms in the cyst cavity itself. This is a response to a high concentration of microorganisms in infected root canals. After proper treatment of the canals, the number of microbes decreases and the body, with the help of cellular immunity, copes with a small number of microorganisms in the area of the root apex. The “barrier” in the form of a thin connective tissue membrane of the cyst becomes unnecessary, and macrophages completely destroy the membrane. With a small size of the cyst, rational treatment and the body’s ability to resist the disease, conservative treatment gives a good result - the shell of the radicular cyst is completely resorbed, the alveolar fascicle bone is restored.
After final treatment of the canals, it is recommended to do a CT scan after 6 and 12 months. If the cyst is completely resolved, there is no need to fear relapses, since the cause (bacterial infection of the canals) has been completely eliminated.
After root canal treatment, the tooth does not receive adequate nutrition, so it may deteriorate over time. To prevent this, it is recommended to cover pulpless teeth with artificial crowns.
If the conservative method is ineffective and the focus of destruction remains, surgical removal of the cyst is performed. This combination of methods is called conservative-surgical treatment.
Surgery
The surgical method involves removing a cyst from a previously pulpless tooth, and often the apex of the tooth root is cut off. The operation is carried out strictly according to indications: in case of a broken instrument, poor-quality treatment of the measles canal, or if the root protrudes into the cavity of the cyst. The extent of surgical intervention is determined during diagnosis.
To improve the prognosis after surgical treatment, bone defects are more often replaced with osteoplastic materials [15][16]. Such materials restore lost bone tissue and stimulate the formation of new one.
One of the main directions in modern reconstructive surgery is the use of biotechnologies, which allow accelerating the processes of regeneration of damaged tissues [17]. We are talking about platelet-derived growth factors obtained from the patient’s own blood. First, venous blood is taken from the patient. Then, using a centrifuge, the blood is separated into fractions. The platelet-rich fraction is used to restore bone tissue defects. This method is available almost everywhere.
There are two main surgical methods for treating radicular cysts: cystectomy and cystotomy.
1. Cystectomy is an operation in which the fibrous membrane of the cyst is completely removed. Usually performed in an outpatient setting under local anesthesia. If the cyst is large and affects the nasal cavity, maxillary sinus or mandibular canal, the operation is performed in a maxillofacial surgery hospital.
Surgical technique:
- Under local or general anesthesia, a section of the jaw bone in the projection of the cyst is skeletonized (exposed).
- Access to the cyst cavity is created, all affected bone tissue and the cyst shell are removed.
- According to indications, the root apex or part of it is cut off and retrograde filling of the root canal is performed (filling through the root apex) and filling of the apical openings of the canals with special cement intended for these purposes.
- The surgical wound is treated with antiseptic solutions, filled with osteoplastic material and sutured.
- Postoperative material is sent for pathohistological examination.
A dental microscope is used for treatment. It allows you to minimize the volume of removal of the root apex and effectively close the root canals.
You must visit the doctor the next day after the operation, then if the course is calm after 10–14 days, to remove the stitches. The patient should be under the supervision of the attending physician until the postoperative wound is completely healed, then return every six months to monitor the restoration of bone tissue and exclude relapse. As practice shows, relapses are rare; they are usually detected in the first year after surgery.
Types of material for filling a bone tissue defect after surgery:
- Autogenous material is obtained from another area of the patient’s bone tissue (branch of the jaw, chin, etc.). Due to its complete biological compatibility, such material is rarely rejected and quickly restores the defect. However, when the patient’s tissue is taken, the operation time increases, the intervention becomes more traumatic, which negatively affects the patient’s recovery.
- Xenogeneic material is obtained after special processing of mammalian bone tissue. The most commonly used bones are ox and pork. Processing removes substances that can cause immune and allergic reactions.
- The synthetic material contains calcium salts. For better compatibility it is often used in combination with autogenous material.
2. Cystotomy is an operation during which the cyst shell is not removed, but only its anterior wall is excised, which allows the contents of the cyst to be evacuated. With cystotomy, the scope of surgical intervention is smaller, but recovery after such an operation lasts longer (about a month). The resulting bone defect is filled with turunda with iodoform, then dressings are made with a certain frequency, replacing the turunda. This method is used less and less due to protracted recovery, the introduction of new techniques and the improvement of the material and technical base.
Oronasal (between the mouth and nose) cystectomy and oronasal cystotomy are performed if the cyst penetrates into the maxillary sinus or pushes it aside.
Surgical methods using laser technology are increasingly used in modern dentistry. Laser techniques are less traumatic. In addition, the laser has a bactericidal property, which reduces the likelihood of developing purulent-inflammatory complications [18][19][20].
Removal of a tooth. A tooth is removed only if saving it is not practical. Indications for removal:
- complete destruction of the crown part of the tooth;
- destruction of the hard tissues of the tooth below the level of the gingival margin by more than 2 mm, when it is not possible to advance the root orthodontically or when the root of the tooth is too short, which will complicate further prosthetics;
- lack of lumen in the root canal (due to structural features or previous treatment).
In all other cases, tooth-preserving operations described above are performed.
Complications after treatment
Complications after cyst removal occur infrequently. These include perforation of the maxillary sinus, damage to the inferior alveolar nerve, as well as the formation of a residual cyst, which is formed during incomplete excision of the radicular cyst.