Publication date: March 13, 2022.
Date the information on this page was updated: February 01, 2022.
TMJ dysfunction is a fairly common pathology these days, as it is largely caused by stress factors. Here it can be difficult to understand what is primary and what is secondary, because people with joint dysfunction usually come with bite pathology, pathology of the musculoskeletal system (curvature of the spine, neck). Therefore, joint treatment is a complex story. It happens that the primary pathology is a pathology of the joint, and sometimes it is the musculoskeletal system.
Comprehensive treatment of TMJ
When the doctor has determined the cause of the joint pathology, or causes, he determines the patient's readiness for a comprehensive treatment plan. In addition to the orthodontist, an osteopath or chiropractor may be involved, or even an orthopedist if more complex correction of the musculoskeletal system is required.
The patient should be aware that it is possible to straighten the jaw using a splint or splint, but this will not solve the problem of malocclusion. Orthodontic treatment will be required to correct the bite. If you have already had orthodontic treatment before, then it is more difficult to decide on repeated treatment.
Therefore, first the problem with the joint is solved using a splint or joint splint, then bite correction is carried out, and, if necessary, prosthetics. In parallel, work is underway with an osteopath to restore the muscular corset of the back and neck.
It happens that a patient refuses treatment with braces after the problem with the joint has been resolved. In this case, we warn him about the need to wear a joint splint constantly in order to avoid the recurrence of old problems with the TMJ. After all, a relapse can happen quite quickly due to stress.
Prevention
It is possible to prevent malocclusion by correcting risk factors associated with behavior; Hereditary predisposition cannot be influenced. Prevention methods:
- During pregnancy, the expectant mother should eat enough foods containing calcium;
- visit a pediatric dentist from the moment the first teeth appear and then at least once a year;
- If possible, breastfeed your baby, avoiding the nipple;
- if the baby is breastfed, then use nipples with a small hole to stimulate sucking;
- Introduce solid foods into the diet in a timely manner.
Important! Parents with malocclusion in children need to start paying attention to preventing the formation of incorrect position of children's jaws as early as possible. Regular myogymnastics classes, as well as all of the above methods, are suitable for this.
Correcting teeth in children is an important task, the timely solution of which will prevent the development of many problems, both physiological and psychological. The doctor chooses the most appropriate method for correcting the bite; control of treatment lies with the parents.
Author: Zhukov M.A.
What may be the symptoms of TMJ dysfunction?
- Tenderness or pain in the area of one or both TMJs at rest or when opening the mouth.
- Crunching, clicking, crepitation and other noises in the area of one or both TMJs when opening the mouth.
- History of TMJ injuries (previous), incl. dislocation, subluxation, chronic subluxation.
- Restrictions in the mobility of the TMJ, restrictions in opening the mouth.
- Excessive tone of the masticatory muscles, bruxism (“grinding” of teeth in sleep, at rest).
- Asymmetry of the chin, lips, lip frenulum, asymmetry of mouth opening, S-shaped opening.
- Suspicion of a forced position of the lower jaw.
Structure of the TMJ
The presence of one or more of the above symptoms may indicate TMJ dysfunction.
Traditional orthodontic treatment does not address TMJ dysfunction. During orthodontic treatment, the severity of dysfunction may not change, decrease or increase. At the moment, in the world scientific orthodontic literature there is no convincing data on the connection between orthodontic treatment and the condition of TMJ. Deterioration of the joint after treatment may have nothing to do with this treatment.
Note! Even in the absence of visible clinical manifestations of joint dysfunction, hidden disorders may occur that require special diagnostics to identify them.
If there is a forced incorrect position of the lower jaw, its position may change during the treatment process with changes and complication of the treatment plan (the need to remove individual teeth, increasing the duration of treatment). A reliably forced position cannot be diagnosed by traditional orthodontic methods; to verify its presence, as a rule, a special analysis is required (manual functional analysis, determination of the central relationship of the jaws), the use of a special articular splint for a period of several months, which, however, does not give 100 % guarantees.
To conduct a detailed articular diagnosis, explain the specifics of your case, and further manufacture an articular splint, you can make an appointment with an orthodontist who deals with the issue of TMJ dysfunction.
TMJ dysfunction is a chronic condition that can be compensated, but not cured (i.e., it is possible to eliminate symptoms, however, pathological changes in the joints, if they have already occurred, will most likely persist).
What happens if TMJ dysfunction is not treated?
If the dysfunction is not treated, the compensatory capabilities of the body may sooner or later be exhausted, the symptoms will worsen, the pathology will begin to progress, causing greater discomfort (sometimes for several years), thereby affecting the deterioration of the function of the dental system.
In order to try to prevent this and carry out treatment taking into account the individual characteristics of the structure and functioning of the temporomandibular joints, patients are usually offered the following approach.
Treatment method for TMJ dysfunction
1. Diagnosis of TMJ dysfunction.
- When diagnosing a joint in the clinic, a series of measurements and tests are carried out, all sensations in the joint area are recorded (discomfort, clicks, pain, deviation of the jaw when opening and closing), the difference in sensations in the right and left joint.
- The orthodontist also takes impressions of the jaws and takes photographs of the face and intraoral photographs, and also performs three-dimensional computed tomography of the face (3D CT); if necessary, the doctor can give a referral for an additional study - magnetic resonance imaging of the TMJ (MRI).
- Often, the orthodontist, in addition to manual functional analysis, conducts a visual assessment of: posture, symmetry of the shoulder girdle, shoulder blades, hip bone structures, etc., performs the necessary tests and photographs. Based on the results, it is possible to schedule a consultation with an osteopath or chiropractor to jointly manage the patient. Related specialists (orthopedist, surgeon, periodontist) can also be involved in drawing up a treatment plan.
What exercises are prescribed to patients to normalize the work and relax the masticatory muscles?
Exercise No. 1
Draw a vertical line on the mirror with a marker, stand opposite so that the line divides your face into the right and left halves, place your fingers on the area of the articular heads, lift your tongue up and back, open and close your mouth along the line (it may not work right away), 2-3 times /day 30 repetitions. There is no need to open your mouth wide (a comfortable width), the main thing is symmetrically (so that the jaw does not “move” in any direction). If there is a click, open until it clicks.
Exercise No. 2 (cycle)
Do it whenever possible, for example, in front of the TV, at the computer, or in a traffic jam while driving. Open and close your mouth without closing your teeth for 30 seconds, then alternately reach your right and left cheeks with your tongue for 30 seconds. Open - close your mouth again, then for 30 seconds move your tongue in a circle inside the vestibule (behind the lips), first in one direction, then in the other direction (clockwise - counterclockwise), open again - close your mouth, etc.. For this a half-hour cycle, the teeth should not touch, the lips should be closed. If you want to close your mouth or swallow, place your tongue between your teeth. Repeat the cycle for 20-30 minutes 2-3 times/day
Custom sports mouth guards
An orthodontist not only treats various pathologies, but also helps prevent dental injuries. Contact sports (boxing, hockey, football) require protection of the front teeth from accidental injury.
To protect the dentition, individual mouthguards are made. They fit precisely to the teeth, are securely fixed in the oral cavity and protect athletes from dental injuries. Made from hypoallergenic materials, used for adults and children.
To make such a mouth guard, you will need two visits to the doctor:
- Taking impressions of the jaws. They are sent to the laboratory, where plaster models are cast, and the mouthguard itself is then cast.
- When the mouth guard is ready, the patient is invited to try it on and is given the design. The doctor gives recommendations on how to care for the mouthguard.
Occlusive therapy for TMJ dysfunction
After diagnosis, the patient is scheduled for an appointment with the orthodontist to determine the central relationship of the jaws (“true” position of the lower jaw, the position in which your joint and chewing muscles will be most comfortable).
In order to more accurately establish and fix this position, an occlusal splint (splint) will be individually made for the patient from a special plastic, which is erased as it is worn. The splint must be worn constantly (sleeping, talking, eating in it if possible) - this is the meaning of occlusion therapy, which will help the joint and masticatory muscles rebuild into the most comfortable functional state.
Cleaning and caring for the splint is very simple - after eating (as well as while brushing your teeth), brush with a soft brush with toothpaste or soap.
Basic information about gnathology
Gnathology is a branch of dentistry devoted to the work of the dentofacial apparatus and all its components - nerves, bones, chewing and facial muscles, periodontal tissues, joints, teeth. It is gnathology that is responsible for the correct structure of the jaw, normal chewing of food, and a beautiful smile.
Every dentist can have minimal knowledge and skills in this area, but when solving more complex and specific problems, you will definitely have to turn to a specialist - a professional gnathologist.
Installation of a brace system for a patient with TMJ dysfunction
Installation of a brace system on the upper jaw is carried out on average after 3 months of occlusion therapy. The splint is adjusted once every 1-2 weeks, or at the discretion of the doctor, until the main complaints from the TMJ are eliminated (in parallel with the alignment of the teeth in the upper jaw), then a brace system is installed on the lower jaw with partial reduction (grinding) of the interfering parts of the occlusal tires, or complete removal. Here the patient needs to be patient - the process may take several months.
At the same time, the new position of the lower jaw is monitored: repeated manual functional analysis, photometry, bite registration is possible, computed tomography of the face during treatment, continuation of orthodontic treatment with a brace system.
Upon completion of orthodontic treatment, final monitoring of the position of the lower jaw follows (manual functional analysis, photometry, bite registration, 3D CT scan of the face upon completion (after) treatment).
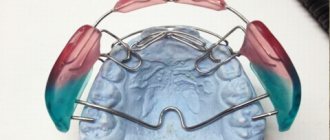
Joint splint
Joint splint with braces
Causes of incorrect formation of children's bite
The following factors lead to malocclusion in children:
- sucking pacifiers;
- long-term breastfeeding (more than 1.5 years);
- tooth decay;
- the predominance of liquid food in the diet;
- inflammation of the gums;
- habits of sucking fingers, biting pencils or nails;
- late eruption;
- broken bite in relatives.
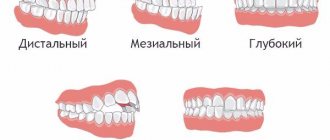
The type of malocclusion is determined by the position of the rows of teeth relative to each other with the jaws closed. The following pathologies in children are distinguished:
- Distal bite – the upper jaw is pushed forward.
- Mesial – the lower jaw protrudes forward
- Open – the front teeth do not meet when the mouth is closed.
- Deep - the upper teeth are significantly lowered down, overlapping the lower teeth by more than half.
- Crossed – teeth meet unevenly.
- Dystopia – teeth do not grow along the growth line.
- Diastema – thinning of teeth, increasing gaps.