Toothache (dentalgia) is a pathological reaction of the body to various diseases, injuries, damage to teeth and gums, as well as anomalies and defects of the jaw. The most common cause of dentalgia in patients of any age is complicated forms of caries, in which inflammation of the internal tissues of the tooth occurs.
Most often, dentalgia in patients is observed with complicated forms of caries
Sometimes the pathogenesis of toothache is based on factors not related to the condition of the oral cavity. If your teeth hurt on one side, but the pain is localized both above and below, you may need not only dental treatment, but also a consultation with a neurologist, otolaryngologist, and even a cardiologist.
Teeth hurt on one side, top and bottom
Sudden toothache on the left side may be one of the reflected symptoms of myocardial infarction, and shooting, aching and throbbing pains may be manifestations of trigeminal neuralgia. Self-medication for such pain is unacceptable due to the high risk of complications, so you should consult a doctor when the first signs of unilateral (widespread) dentalgia appear.
Why is tooth extraction required?
In certain cases, tooth extraction is the only possible method of solving a particular dental problem. Indications for removal may include:
- Incorrect position of the tooth, when neither the patient nor the doctor can access it (high-quality hygiene and/or treatment is impossible);
- The absence of the main part of the dental material without a chance of its restoration;
- Malocclusions (for example, severe crowding);
- Inflammatory process in the roots of the tooth, which can lead to infection;
- Painful eruption of wisdom teeth.
This is also necessary when preparing to correct your bite using Invisalign aligners. In particular, it is usually necessary to remove the “eights” if they have not fully erupted and can interfere with quality orthodontic treatment. It is worth noting that such a decision should be prepared when there are certain indications and no other option is possible.
Otherwise, when installing aligners, the unerupted tooth hidden inside the gum will prevent the aligner from attaching and pull the remaining teeth in the right direction, leaving them no room to move.
Each organ has its own tooth
It has been known since ancient times that the condition of a particular tooth can determine the disease in the corresponding group of organs. Today this is a scientifically proven fact. For example, by using the incisors above and below (teeth 1 and 2), diseases of the ears, bladder and kidneys can be diagnosed, and by the canines (3) the condition of the liver and gallbladder can be determined. Small molars (premolars 4 and 5) transmit data about the lungs and large intestine, and large molars (molars 6 and 7) about the stomach, spleen and pancreas, and the so-called “wisdom teeth” can tell about the condition of the heart and small intestine .
At the same time, affected teeth identified by a dentist during an examination do not always mean the presence of diseases in the corresponding internal organs. It happens that a patient presents with pain in apparently healthy teeth or even with phantom pain (a painful signal comes from an internal organ to the site of the extracted corresponding tooth). Knowing about these relationships, it is easier to identify the affected organs.
Why does a pulled out tooth hurt?
The presence of pain after tooth extraction is due to the fact that soft tissues, blood vessels and nerves are damaged during tooth extraction. Typically, the first pain symptoms appear 3-4 hours after surgery. This is due to the fact that this is when the anesthesia stops working.
Also, during removal, the bone tissue of the jaw socket may be damaged. In this case, the pain during the healing period is more intense and prolonged. However, if the removal was carried out correctly, it will soon pass.
How long does it hurt?
In most cases, pain during removal worsens on the second day. On the third day they begin to decrease. By the fourth or fifth day, there is practically no pain. If by this period the pain after tooth extraction does not subside, the patient should consult a doctor, as this may indicate the emergence of complications.
However, it is important to remember that complete healing of the hole occurs only in the second or third week after the procedure. Until this time, the gums and bone tissue are vulnerable, so if they are irritated, pain may also occur. To prevent this from happening, you should follow your doctor's recommendations.
Headache
The recovery period after tooth extraction may be accompanied by headaches of varying intensity. They are associated with damage to the nerve fibers that go to the brain. Such symptoms should not frighten the patient, since as the wound heals, they will also pass.
Another cause of headaches during this period may be hypertension. The patient must notify the attending physician about the presence of such an illness. In this case, the surgeon will be able to select appropriate medications that will reduce pain.
Ear pain
For the same reasons, a patient may experience unpleasant or even painful sensations in the ear after tooth extraction. Most often they have a shooting character. This symptom is also normal and goes away in the coming days after the intervention.
Ear pain may worsen if, after the procedure, the patient does not properly care for the oral cavity and tries to chew solid food.
Pain in the gums
Pain in the gum is associated with its direct damage. In this case, not only the soft tissue suffers, but also the nerves, which are also located in the gums. Depending on the degree of damage, pain can last for different times and occur with greater or less intensity.
Increased pain in the gum may indicate the presence of fragments in its tissues, as well as the occurrence of one or another complication. If such symptoms occur, you should immediately consult a specialist.
Dental causes of unilateral dentalgia
Dental diseases and pathologies are the most common cause of dentalgia, regardless of its location and degree of prevalence. Pain in teeth simultaneously in the upper and lower jaw can be the result of deep caries on several teeth. If a person has several adjacent teeth affected, the pain syndrome, typical for complicated forms of this pathology, will be perceived as widespread pain on one side, while the person most likely will not be able to accurately indicate which tooth hurts.
- How long does it take for drugs to leave the body?
Video: Caries and its complicated forms
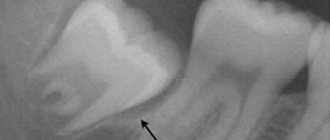
Complicated forms of caries
Complicated deep caries ranks first among all causes of toothache, since in this form a carious cavity is not only formed in the tooth, containing necrotic tissue, bacterial plaque and food debris, but also the peripulpal dentin (the bone tissue of the tooth surrounding its pulp) is damaged. .
Complicated caries
If the patient does not seek dental care for superficial or moderate caries, the pathological process can become complicated or spread to neighboring teeth.
Note! Caries is a slow-moving, but persistently progressive pathology, and inevitably leads to tooth destruction if left untreated. From the moment the chalk stain forms until deep damage to the hard tissues of the tooth occurs, it usually takes about 3 years.
Acute pulpitis (periapical dentalgia)
Acute forms of pulpitis are among the most painful dental pathologies. This disease is characterized by a widespread course of pain, so if all teeth on one side hurt, you should immediately consult a dentist and rule out damage to the pulp and periapical tissues of the tooth. Pulp is connective tissue that has a loose structure and is located in the dental canals. In addition to a large number of lymphatic and blood vessels that nourish the tooth from the inside, the pulp also contains many nerve endings, so the pain with pulpitis is always very strong (pulsating or aching).
Acute pulpitis
Pulp inflammation can also be suspected based on other symptoms (assessed collectively), which include:
- increased pain during night sleep;
- periodic nature of pain;
- severe dental hyperesthesia (increased sensitivity);
- persistence of painful sensations after removal of the irritant (this sign makes it possible to differentiate pulpitis from caries).
With pulpitis, pain can spread to the entire half of the jaw and intensify after contact with cold and hot food. In the case of purulent inflammation, increased pain is typical only when the affected area is heated, and the use of cold, on the contrary, relieves the pain and slightly reduces its intensity.
Untimely treatment of pulpitis is dangerous for the development of chronic diseases. If you ignore the problem, there will be complete destruction and loss of the tooth. Pulpitis is treated surgically, partially preserving the pulp or completely removing tissue, nerves and blood vessels of the tooth. You can learn more about the methods, as well as whether it is painful to treat pulpitis, in the article at the link.
Apical periodontitis
Periodontitis is characterized by inflammation of the periodontal tissues located between the tooth root and the alveolar plate and holding the tooth in the bony alveolus.
Acute apical periodontitis
Inflammatory periodontal lesions can be caused not only by infections (mostly deep caries), but also by various injuries, mechanical damage (for example, from fruit or fish bones), and improper use of medications. Often, pain, indicating the onset of periodontitis, occurs after dental treatment, when irritating materials or drugs (arsenic, formaldehyde) enter the periodontal fibers. If, after visiting the dentist, a person begins to experience girdling pain on the right or left side, he should return to the dentist’s office to rule out periodontal damage.
A distinctive symptom of apical periodontitis is the appearance of local pain that occurs strictly in the projection of the affected tooth. As the inflammatory process progresses, the pain becomes reflected and can radiate to neighboring teeth, as well as the jaw, ear or temple.
- Treatment of cystitis in women and men. How to properly treat cystitis?
Note! Periodontitis can clinically have the same symptoms as pulpitis, but an important difference between this pathology is the appearance of pain during vertical percussion (tapping) of the affected tooth.
Necrotizing ulcerative gingivitis
Gingivitis is a fairly common dental disease that is inflammation of the gums.
Ulcerative gingivitis
Gingivitis itself rarely causes shingles toothache, and all discomfort is localized exclusively in the gum area. This may include itching, burning, tingling, pinching, and increased dryness (xerostomia). But some forms of gingivitis are particularly painful and can cause severe or moderate pain that spreads to several teeth on one side of the jaw.
Hypertrophic gingivitis
Types of gingivitis, which are characterized by widespread dentalgia
| Variety | Peculiarities |
| Scaly (desquamative) | It is characterized by profuse exfoliation of gingival epithelial cells and intense redness in the area of maximum pain. |
| Ulcerative | The gums begin to bleed, turn red, and show signs of ulceration. In 80% of cases, patients complain not only of unilateral dentalgia, but also of itching and burning of the mucous membranes. |
| Hyperplastic | Gums with hypertrophic gingivitis change their color (cyanosis and an unnatural purple tint appear), bleed, and pus may be released from them. A distinctive feature of this type of gingivitis is the formation of false zebu-gingival pockets and an increase in the volume of periodontal papillae. In severe forms, the degree of tooth hyperplasia can reach ½ of the dental crown. |
| Necrotizing ulcerative | This type of gingivitis is called necrotic, since its main manifestation is necrosis (death) of the gingival papillae located between the teeth. |
Treatment of gingivitis
Will the site of the extracted tooth stop hurting on the second day?
Patients often believe that the pain at the site of pulled out teeth should go away after sleeping on the second day, and they get scared when it becomes even stronger. This situation is normal, since after a certain time the damaged gum tissue begins to swell, thereby pinching the nerves. All this leads to pain becoming more intense.
You need to be prepared for this. Today there are a large number of analgesics and other medications that can reduce inflammation and eliminate pain syndromes.
The site of tooth extraction hurts after a week, what should I do?
The holes in which the extracted teeth were located are usually completely healed by the end of the first week. Final healing still needs to wait, but the pain should have passed during this period. If, after a week, the area continues to hurt after tooth extraction or any other symptoms appear, such as bleeding, the patient urgently needs to see a doctor.
Under no circumstances should you try to relieve pain on your own. If it continues to bother the patient, this may indicate the development of inflammation or an abscess process in the gum. If they are not eliminated in time, the consequences can be very serious.
A dental problem is not just a dental problem
Pain in the quads above and below can be a sign of weak ligaments (shoulder, elbow, wrist, ankle and knee joints), chronic inflammation of the joints (for example, polyarthritis), diseases of the large intestine - diverticulosis, polyposis.
Sixes and sevens (molars) are beacons of gastrointestinal diseases (gastritis, gastric or duodenal ulcers), advanced anemia, chronic pancreatitis. Problems with the top six are a reason to get checked for tonsillitis and sinusitis, diseases of the pharynx and larynx, tumor formations in the thyroid gland, mastopathy, and inflammation of the appendages. If something is wrong with the lower sixes, there are problems with the arteries, atherosclerosis. But the lower sevens are problems with the lungs (chronic pneumonia, bronchitis, bronchial asthma), polyps in the large intestine, something is wrong with the veins (varicose veins, hemorrhoids).
Have your wisdom teeth been bothering you for a long time? Make an appointment not only with the dentist, but also with the cardiologist. Coronary heart disease, congenital heart disease and other cardiac diseases - in terms of wisdom teeth. Plaque and tartar can be a signal of endocrine system disorders, a sign of gastric ulcer.
Stages of socket healing
The holes in the place of pulled out teeth heal in several stages. The first one lasts about a week. At this time, the wound heals, its surface becomes smoother. The patient can return to his usual lifestyle - eat regular food, brush his teeth, etc. Usually, during this period, a blood clot remains on the surface of the hole, which in no case should be torn off, as this can lead to bleeding and will slow down the final healing process.
Complete healing of the wound ends by the end of the second week. At this time, the clot disappears, and residual pain goes away. The last stage, that is, complete healing, ends by the end of the third week. If the intervention was very serious, this period may last 4 weeks. By this time, the nerve fibers and blood vessels are completely restored, and the gums become completely smooth.
Complications after removal
In some cases, tooth extraction can cause complications. They can be associated both with poor quality of the procedure itself and with illiterate oral care during the healing period.
The main complications that may arise during tooth extraction include the following:
- an abscess that appears as a result of infection in open wounds in the sockets where teeth used to be;
- bleeding, which may be a consequence of injury to the gums during the healing period, and may also occur due to the presence of hypertension or poor blood clotting in the patient;
- paresthesia, characterized by numbness of the gums or part of the jaw in the place where the tooth was pulled out.
One of the most serious complications is osteomyelitis. It is characterized by the presence of an inflammatory process in the bone and bone marrow. This disease can occur when the patient has an infection of the bone tissue against the background of a general decrease in immunity. This disease requires immediate treatment.
Symptoms
The main symptom of a complication after tooth extraction is increased pain after the 5th day of healing. If by this period they do not subside, then you need to contact a specialist to find out the reasons. This could be either inflammatory processes or the presence of tooth particles that went unnoticed after the procedure.
Another symptom is a strong increase in temperature, sharp cramps in the head that last more than 5 days. This can also cause your gums to swell. If this happens, it means that the swelling cannot go away for some reason. This, in turn, is a sure sign of a complication.
Reasons for the development of complications
There can be a large number of reasons for the appearance of one or another complication. In addition to medical errors and improper oral care, these include the presence of certain physical diseases in the patient, which can lead to the development of inflammation or frequent bleeding.
To prevent such situations from arising, the patient must warn the doctor about all his ailments, even if he is sure that they will not affect the outcome of the procedure. After this, the specialist will be able to select certain medications that will reduce the risk of complications and make the wound healing process more comfortable.
Pain is a good signal
The connection between internal organs and teeth and the oral cavity is evidenced by medical statistics on patient treatment accumulated over many years. For example, bad teeth can be a source of headaches. Damage to molars - there is pain in the parieto-occipital region. A source of infection in the maxillary incisors can lead to pain in the frontotemporal region, and from diseased canines the pain can be concentrated in the temporal region. If you have problems with the teeth of the lower jaw, a migraine may develop, and it can only be alleviated by visiting a dentist.
Painful sensations in the upper and lower incisors are a reason to get checked for cystitis, otitis media, or treat chronic pyelonephritis. Pain in the first incisor is a possible syndrome of prostate adenoma, frontal sinusitis, tonsillitis, prostatitis, osteochondrosis. Aching pain in the fangs is possible with hepatitis or cholecystitis.
Chronic pneumonia can be diagnosed by pain in the 4th and 5th molars. The same focus of pain indicates colitis, advanced dysbacteriosis, an allergic reaction (rhinosinusitis, bronchial asthma, respiratory allergosis).
What to do after removal?
After tooth extraction, it is important to maintain proper oral hygiene and also slightly limit your diet. The main recommendations are:
- You can apply a cold compress to the damaged gum, which will reduce the pain;
- if the bleeding does not decrease, you can firmly press a cotton swab between the teeth in the area of tooth extraction;
- For disinfection, rinses based on natural herbs should be used;
- It is better to eat only warm and soft foods without solid particles.
Medications can also be used to reduce discomfort. However, you can only use those medications prescribed by your doctor. He should also tell you how long to rinse so as not to damage the wound.
If at any stage of healing the patient feels an increase in pain symptoms or discomfort that is not normal, he should immediately inform the doctor.