Mechanisms of action and types of anesthetics
Anesthetics are divided into:
- Local
- General: a) inhalation - volatile liquids and gases b) non-inhalation (intravenous)
Table 1
1. Local anesthetics
Local anesthetics reversibly reduce the excitability of sensory nerve endings and block the conduction of afferent impulses in the nerve trunks in the area of direct application, and are used to eliminate pain.
The first drug of this group, cocaine, was isolated in 1860 by Albert Newman from the leaves of the South American shrub Erythroxylon coca. Newman, like many chemists of the past, tasted the new substance and noted a numbness in his tongue. Professor of the Military Medical Academy of St. Petersburg Vasily Konstantinovich Anrep in 1879. confirmed the ability of cocaine to cause anesthesia. In experiments on frogs, he discovered that cocaine had a “paralyzing effect” on the endings of sensory nerves. V.K. Anrep studied the effect of cocaine on himself: an injection of cocaine in a dose of 1 - 5 mg under the skin was accompanied by complete anesthesia - a pin prick or cauterization with a smoldering match did not cause pain. A similar effect was observed when a cocaine solution was instilled into the eye and applied to the mucous membrane of the tongue.
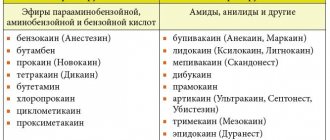
Local anesthetics are classified into esters (anesthesin, dicaine, novocaine) and substituted amides (lidocaine, trimecaine, bupivacaine). Local anesthetics - esters are hydrolyzed by blood pseudocholinesterase and act for 30 - 60 minutes. Their effect is prolonged by anticholinesterase drugs (prozerin). The hydrolysis product, n-amino-benzoic acid, weakens the bacteriostatic effect of sulfonamides. Substituted acid amides are inactivated by the liver monooxygenase system within 2-3 hours. Bupivaquine causes local anesthesia lasting 3-6 hours, after its cessation the analgesic effect persists for a long time.
From the point of view of practical use, anesthetics are divided into the following groups:
- Agents used for superficial (terminal) anesthesia: Cocaine, Dicaine, Anestezin, Pyromecaine
- Agents used primarily for infiltration and conduction anesthesia: Novocaine, Bupivacaine
- Agents used for all types of anesthesia: Lidocaine, Trimecaine
Mechanism of action
Local anesthetics are tertiary nitrogenous bases. They consist of hydrophilic and lipophilic parts connected by ester or amide bonds. The mechanism of action is determined by the lipophilic part, which has an aromatic structure. For application to mucous membranes and skin and parenteral administration, aqueous solutions of hydrochloride salts of local anesthetics are used. In the slightly alkaline environment of tissues (pH = 7.4), salts are hydrolyzed, releasing bases. The bases of local anesthetics dissolve in the lipids of the membranes of nerve endings and trunks, penetrate to the inner surface of the membrane, where they are converted into an ionized cationic form.
Figure 1 | Mechanism of action of local anesthetics
Receptors for local anesthetics are localized in the S6 segment of domain IV of the intracellular part of sodium channels. By binding to receptors, local anesthetic cations prolong the inactivated state of sodium channels, which delays the development of the next action potential. Local anesthetics do not interact with closed channels during the resting potential period. Thus, action potentials do not develop in the area where local anesthetics are applied, which is accompanied by a block in the conduction of nerve impulses. The selective effect of local anesthetics on sensory afferent nerves is due to the generation of long-lasting (more than 5 ms) high-frequency action potentials in them.
First of all, local anesthetics block unmyelinated C and myelinated Aδ and Aβ fibers (afferent pathways conducting pain and temperature stimuli; autonomic nerves). Local anesthetics act on fibers surrounded by a myelin sheath at the nodes of Ranvier. Thick myelinated fibers (afferent pathways that conduct tactile stimulation; motor nerves) respond less well to local anesthetics. In addition, the resistance of motor nerves to anesthesia is due to low-frequency short (less than 5 ms) action potentials. In the focus of inflammation, under conditions of acidosis, the dissociation of hydrochloride salts of local anesthetics and the formation of their free lipid-soluble bases are disrupted, so the analgesic effect is lost. For example, local anesthesia may not be effective for tooth extraction in cases of severe periodontitis.
2. General anesthetics
2.1. Inhalational anesthetics
2.1.1 Volatile liquids
Theories of the mechanism of action of general anesthetics
The effects of inhalational anesthetics cannot be explained by a single molecular mechanism. Most likely, the multicomponent action of each anesthetic is realized through many targets. However, these effects converge on a limited number of changes underlying the physiological effects. At the moment, there are lipid and protein theories of anesthesia, but none of them yet describes the sequence of events occurring from the interaction of the anesthetic molecule and its targets to physiological effects.
Figure 2 | Inhalational anesthetics
The activity of inhalational anesthetics is assessed by the minimum alveolar concentration (MAC). A dose producing 1 MAC prevents movement in response to surgery in half of patients. The potency of general anesthetics correlates with their lipid solubility, suggesting the importance of interaction with hydrophilic targets. In particular, the discovery of a relationship between the strength of an anesthetic and its lipophilicity (Meyer-Overton's rule) gave rise to the lipid theory of the mechanism of action of anesthetics. The lipid theory of anesthesia states that anesthetics dissolve in the lipid bilayer of biological membranes and cause anesthesia by reaching a critical concentration in the membrane. The most sophisticated versions of the lipid theory require that anesthetic molecules cause perturbation (changes in properties) of the membrane.
Figure 3 | Meyer-Overton rule
Figure 4 | In the 20th century, it was shown that the potency of general anesthetics correlates with their ability to inhibit the activity of the soluble enzyme luciferase, which is not a physiological target of anesthetics but serves as a lipid-free model protein molecule for anesthetic binding.
Modern facts suggest that proteins, to a greater extent than lipids, are molecular targets for the action of anesthetics. The interaction of anesthetics with hydrophobic regions of proteins also explains the Meyer-Overton rule. The direct interaction of anesthetic molecules with proteins allows us to explain exceptions to this rule, since any sites of binding with a protein are determined both by the size and shape of the molecule, and by solubility. Numerous physical methods (X-ray diffraction, NMR spectroscopy) confirm that general anesthetics act by directly binding to the amphiphilic cavities of protein molecules, and the size of the bound region explains the effect of “chopping off” the properties (longer alcohols lose their anesthetic properties).
Mechanism of action
Thus, general anesthetics change the physicochemical properties of neuronal membrane lipids and disrupt the interaction of lipids with ion channel proteins. At the same time, the transport of sodium ions into neurons is reduced, the output of less hydrated potassium ions is maintained, and the permeability of chloride channels controlled by GABA-A receptors increases by 1.5 times. The result of these effects is hyperpolarization with increased inhibition processes. General anesthetics suppress the entry of calcium ions into neurons by blocking H-cholinergic receptors and NMDA glutamic acid receptors; reduce the mobility of Ca2+ in the membrane, therefore preventing the calcium-dependent release of excitatory neurotransmitters. The most sensitive to the action of general anesthetics are the polysynaptic systems of the central nervous system—the cerebral cortex (1013–1014 synapses), the thalamus, the reticular formation, and the spinal cord. The respiratory and vasomotor centers of the medulla oblongata are resistant to anesthesia.
Volatile inhalational anesthetics:
- postsynaptically enhance inhibitory transmission by potentiating ligand-gated ion channels activated by GABA and glycine;
- extrasynaptically by enhancing GABA receptors and ionic leakage currents;
- presynaptically by increasing basal GABA release.
Inhalational anesthetics inhibit excitatory synaptic transmission by reducing glutamate release and postsynaptically by inhibiting ionotropic glutamate receptors. The paralyzing effect of local anesthetics involves the spinal cord, while sedation/anesthesia and amnesia involve the supraspinal mechanisms of memory, sleep and consciousness.
2.1.2. Gas anesthesia
In anesthesiology, the inhalation gas anesthetic nitrous oxide (N2O) is widely used. At the end of the 1980s. The inert gas xenon entered foreign anesthesiological practice.
Nitrous oxide is a colorless gas with a characteristic odor, stored in metal cylinders under a pressure of 50 atm in a liquid state, does not burn, but supports combustion. Its mixtures with anesthetics of the group of volatile liquids are explosive in certain concentrations. In subnarcotic concentrations (20 - 30%) of nitrous oxide causes euphoria (laughing gas) and strong analgesia. At a concentration of 20% it provides pain relief to the same extent as 15 mg of morphine. Nitrous oxide does not affect GABA-A receptors. Used only in combinations, as the MAC is 104%.
The inert gas xenon is considered the best alternative to nitrous oxide, as it has a more pronounced anesthetic effect, indifference and environmental safety. The ability of xenon to cause anesthesia was discovered in connection with the practice of deep-sea diving and the development of hyperbaric physiology. Xenon is colorless, does not burn and has no odor; upon contact with the mucous membrane of the mouth, it creates a sensation of a bitter metallic taste on the tongue. It is characterized by low viscosity and high solubility in lipids, and is excreted unchanged by the lungs. A xenon-saving anesthesia technology has been developed that includes a minimum flow and a recycling system for repeated reuse of gas. This technology successfully solves the practically important problem of the shortage and high cost of xenon. In the mechanism of the anesthetic effect of xenon, blockade of cytoreceptors of excitatory neurotransmitters - H-cholinergic receptors, NMDA receptors of glutamic acid, as well as activation of receptors of the inhibitory neurotransmitter glycine are important. When interacting with cytoreceptors, xenon acts as a proton-binding cluster and forms complexes with the cations HCO+, NH2+, HNCH+. Xenon exhibits antioxidant and immunostimulant properties, reduces the release of hydrocortisone and adrenaline from the adrenal glands.
2.2. Non-inhalation (intravenous) anesthetics are divided into three groups:
Short-acting drugs (3 - 5 min)
- propanidine (epontol, sombrevin)
- propofol (diprivan, recofol)
Medium-acting drugs (20 - 30 min)
- ketamine (calypsol, ketalar, ketanest)
- midazolam (dormicum, flormidal)
- hexenal (hexobarbital sodium)
- thiopental sodium (pentothal)
Long-acting drugs (0.5 - 2 hours)
- sodium hydroxybutyrate
Figure 5 | General anesthetics for intravenous administration
Mechanism of action
The most widely used intravenous anesthetic is propofol. Its mechanism of action is associated with an increase in chloride conductivity of GABA receptors.
Methohexital is close to propofol in terms of the speed of onset and recovery from anesthesia.
Barbiturates were used for anesthesia before the introduction of propofol. Thiopental causes rapid onset and rapid recovery from anesthesia with a single injection, but it accumulates rapidly with repeated or prolonged administration and thus slows recovery from anesthesia. Barbiturates are ligands of barbiturate receptors. In small doses, they allosterically enhance the effect of GABA on GABA A receptors. At the same time, the open state of chlorine channels lengthens, the entry of chlorine anions into neurons increases, and hyperpolarization and inhibition develop. In large doses, barbiturates directly increase the chloride permeability of neuronal membranes. In addition, they inhibit the release of excitatory mediators of the central nervous system - acetylcholine and glutamic acid, and block AMPA receptors ( quisqualate receptors) of glutamic acid. Barbiturates have cerebroprotective properties and can be used for this purpose.
Benzodiazepines are used mainly as anxiolytics and for sedation with preservation of consciousness. All benzodiazepine receptors allosterically enhance the cooperation of GABA with GABA A receptors, which is accompanied by an increase in the chloride conductivity of neurons, the development of hyperpolarization and inhibition. The reaction with benzodiazepine receptors occurs only in the presence of GABA. Remimazolam is the youngest benzodiazepine and has a very short duration of action due to rapid neutralization by plasma esterases.
Ketamine is chemically a derivative of phencyclidine. The synaptic mechanisms of action of ketamine are diverse. It is a non-competitive antagonist of the excitatory brain mediators glutamic and aspartic acids in relation to NMDA receptors. These receptors activate sodium, potassium and calcium channels in neuronal membranes. When receptors are blocked, depolarization is disrupted. In addition, ketamine stimulates the release of enkephalins and β-endorphin; inhibits the neuronal uptake of serotonin and norepinephrine. The latter effect is manifested by tachycardia, an increase in blood pressure and intracranial pressure. Ketamine dilates the bronchi. When recovering from ketamine anesthesia, delirium, hallucinations, and motor agitation are possible (these adverse events are prevented by the administration of droperidol or tranquilizers). An important therapeutic effect of ketamine is neuroprotective. As is known, in the first minutes of brain hypoxia, excitatory mediators - glutamic and aspartic acids - are released. Subsequent activation of NMDA receptors, increasing the concentration of sodium and calcium ions and osmotic pressure in the intracellular environment, causes swelling and death of neurons. Ketamine, as an antagonist of NMDA receptors, eliminates ion overload of neurons and the associated neurological deficit.
The newest intravenous anesthetic is dexmedetomidine. It is a highly selective α2-adrenergic receptor agonist with sedative, sympatholytic, hypnotic and analgesic effects. Its main action is as an agonist at the a2 receptors in the locus coeruleus.
Sources:
- Theories of the mechanism of action - https://en.wikipedia.org/wiki/Theories_of_general_anaesthetic_action and https://www.esus.ru/php/content.php?id=744
- Vengerovsky A.I., Lectures on pharmacology for doctors and pharmacists 2007
- Kharkevich, Pharmacology ed. 10
- Miller's anesthesia / Ronald D. Miller; associate editors, Neal H. Cohen, Lars I. Eriksson, Lee A. Fleisher, Jeanine P. Wiener-Kronish, William L. Young. - Eighth edition. 2015
Indications for use
Local anesthetic preparations are widely used in dentistry for infiltration anesthesia - during tooth extraction (removal) and minor operations on the periodontium (gums).
In order to achieve superficial anesthesia, local anesthetics are used in ophthalmology - in the form of eye drops during operations on the conjunctiva (for laser vision correction, removal of foreign bodies from the eye) and the cornea.
In addition, local anesthetics for superficial anesthesia are used for wounds, minor surgical operations on the skin and mucous membranes, and for ulcers, including gastric ulcers - some local anesthetic preparations (for example, benzocaine) are part of combination drugs that reduce the acidity of gastric juice (antacids).
Certain drugs (lidocaine) are used in endoscopic diagnostics to facilitate the procedure - anesthesia of the pharynx before inserting a tube through the mouth or nose; placement of a urinary catheter.
To achieve conduction anesthesia, local anesthetics are used for pain relief during childbirth (epidural anesthesia), operations on the pelvic organs and lower extremities.
The local anesthetic lidocaine, in addition to its local anesthetic effect, has an antiarrhythmic effect, so it is also used for heart rhythm disturbances - arrhythmias.