According to antiplagiat.ru, the uniqueness of the text as of October 16, 2018 is 99%.
Key words, tags: caries, pulpitis, bone tissue destruction, cyst, odontogenic cyst, flux, OPTG image, tooth-preserving operations, resection of the apex of the tooth root, cystectomy, root amputation, dental microscope, preservation, tooth extraction .
There are many different dental diseases, but perhaps the most serious among them in terms of the degree of damage caused is periodontal inflammation - periodontitis. Occurring in the vast majority of cases as a complication of caries and/or pulpitis, it poses a serious threat, because under its influence not only the tooth is destroyed, but also the soft and hard tissues surrounding it, in addition, it has a negative effect on the immune system. This disease requires immediate medical intervention, which, today, has an impressive arsenal of very effective techniques.
Historical reference
Periodontitis, as a concept, did not previously exist, but, of course, this disease has worried humanity, and its history dates back more than one millennium. Thus, in the scientific literature there has been a discussion for a very long time about the methods of dental treatment in Ancient Egypt. The basis for the debate is a number of artifacts, which indicate the predominance of conservative treatment methods in dentistry of that time, and no traces of surgical intervention were identified during the study of the mummies of the pharaohs1. At the same time, a study of mummies showed that the ancient Egyptians suffered from severe damage to the teeth and periosteum, from which we can conclude that periodontitis “flourished” among the first persons of Ancient Egypt, along with other dental diseases. Egyptologist M.A. Raffer wrote that in Egyptian cemeteries it was not uncommon to find diseased teeth that had almost fallen out of inflamed sockets, or carious teeth that were the cause of extensive diseases of the jaws, which could have been avoided and/or cured by performing simple operations 1.
In general, the existence of these dental artifacts inexorably indicates that such a pathology of the dental system as periodontitis has existed for more than one century. But in those days, the symptoms by which today medical science classifies and treats this disease were symptoms of simply a “sick tooth.”
More than a century and a half later, in 1889, a Swiss mechanic and formerly an experienced watchmaker, August Maillefer, who was seriously interested in dentistry, together with his three sons founded a company that was engaged in the creation of high-precision mechanical instruments and gave it his family name - Maillefer. Maillefer used his extensive experience working with watch movements, characterized by unsurpassed “Swiss” precision, to expand the capabilities of dentistry.
Perhaps the first serious treatise, which described about 130 dental diseases caused by various reasons, was the work “The Dentist-Surgeon, or Treatise on Teeth” by P. Fauchard, published in 1728. He also became the author of a number of new filling materials and dental instruments 2. As if anticipating the role endodontic instruments would play in the future, the Maillefer company was the first in the world to invent trimers, pulp extractors, files - tools for working in dental canals. Since 1995, this company became part of the DENTSPLY concern, later called DENTSPLY IMPLANTS, and today it is DENTSPLY SIRONA. And it was the developments of August Maillefer’s company that became the “first signs” of modern endodontic instruments, without which effective, efficient and reliable treatment of periodontitis is impossible today.
Periodontal anatomy
The periodontium (from Latin perio - around, around; odontos - tooth) is a complex of tissues surrounding the tooth and holding it in the socket. It includes the gum, dental cement, alveolar bone, periodontal ligament, which is located between the dental root and the alveolar plate and communicates between the alveolar bone and the cement of the tooth root. The periodontium consists of many blood and lymphatic vessels, nerve endings, and periodontal fibers. The thickness of periodontal fibers depends on age and averages 0.2 mm, becoming thinner over the years. The periodontal ligamentous apparatus is represented by groups (bundles) of fibers that have different directions, connecting all areas of the periodontium into a single system, stretching between the teeth, from the cement of one tooth to the cement of another. The ground substance of the periodontium occupies about 60% and is an amorphous gel-like substance, 70% consisting of water. A large amount of base material and water in it are factors that play a huge role in providing shock absorption. A characteristic feature of the cellular structure of periodontal tissue is the ability for rapid renewal, but with age this process becomes slower. The structural integrity of the periodontium is ensured by the enamel attachment, the cells of which are completely renewed within 4–8 days. This ability to renew provides mechanical protection of the entrance to the marginal part of the periodontium and reduces the risk of negative factors affecting it. The periodontium performs the most important functions. Plastic – ensures the growth and development of teeth due to the activity of osteoblasts and cementoblasts; trophic – provides nutrition to the cement base of the tooth and the alveolar plate; supporting-retaining – ensures fixation of the tooth in the alveolus; shock-absorbing - distributes chewing pressure due to the ligamentous apparatus; protective – prevents the entry of pathogenic microorganisms and the spread of inflammatory processes 3.
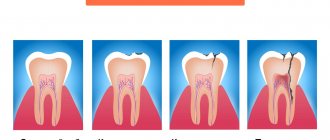
Periodontitis: definition, etiology, symptoms
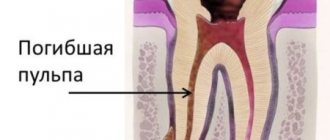
Periodontitis is a disease characterized by inflammation of the complex of tissues surrounding the tooth and holding it in the socket. Based on etiology, there are several types of periodontitis. Infectious periodontitis is the most common (90% of all cases) and occurs due to the irritating effect on the periodontium of the infectious-toxic contents of the root canals. As a rule, the cause of this is caries or pulpitis, in some cases – poor-quality root canal treatment. The process of disease development begins with the entry of microbes into the tooth canal, where they undergo natural selection in the harshest conditions of a closed anaerobic space. The strongest bacteria, surviving, form a special class, which is collectively called “odontogenic microflora”. It differs from the dental microflora of the oral cavity in its unique vitality and extremely aggressive effect of its metabolic products on surrounding tissues. Gradually, in the apical and apicolateral zones or, less commonly, in the bifurcation zone, the process of destruction of bone tissue begins. If there are epithelial elements in the above areas, they become involved in the odontogenic inflammatory focus and begin to grow, forming a granuloma. Next, the granuloma develops and enters the so-called transitional stage - cyst-granuloma and then “grows” into a cyst. Depending on a number of factors, such as the activity of pathogenic microflora, the strength of the immune system, characteristics of the chewing load, the frequency of stressful conditions, living conditions and others, an odontogenic cyst can be a source of constant discomfort or not bother the patient at all. An “asymptomatic” cyst can grow to enormous sizes, causing many dental pathologies and even jaw deformation due to the involvement of a large number of teeth in the growth process. It is extremely rare that the infection enters the periodontium through the blood or lymph flow. In such cases, the disease is called retrograde periodontitis. Traumatic periodontitis is the result of an injury - domestic or sports, when the patient receives a severe bruise, or iatrogenic, that is, caused by the actions of a doctor (for example, an accidental endodontic injury, a piece of an endodontic instrument left in the canal, a filling with the filling material extending beyond the apex of the root, an over-inflated filling or crown, causing permanent microtrauma). With acute trauma, acute periodontitis develops, characterized by visible injury to soft tissues, hemorrhage, and the appearance of tooth mobility. With chronic trauma, changes in the periodontium occur gradually. Drug-induced or toxic periodontitis is most often a complication of the treatment of pulpitis, when drugs containing arsenic, sodium hydrochloride, resorcinol-formalin mixtures, aseptic solutions, and some filling materials cause irritation, necrotization and inflammation of the periodontium. In some cases, toxic periodontitis may be caused not by drugs, but by decay products of the pulp, which has undergone necrotic damage due to poor-quality filling during caries. Symptoms of periodontitis may vary depending on the stage of the disease and the location of the inflammation. Thus, a pulsating, constantly increasing localized pain occurs when biting, closing teeth, and even when touching them. Eating food and fluids often becomes difficult and may sometimes be accompanied by a fever. Patients often note that the tooth feels like it has “grown” and there is a feeling of fullness. Symptoms also include swelling of the gums, gumboil, and fistula. At the same time, periodontitis at its various stages may be asymptomatic or accompanied by some discomfort in the area of the diseased tooth. Types of periodontitis according to the clinical picture of the disease Periodontitis is a complex, serious disease that medical science has carefully studied for several decades. In the process of searching for effective methods of its treatment, various species classifications were developed, which made it possible to recognize and treat periodontitis in its most diverse manifestations. Today, the most authoritative is the International Classification of Diseases ICD-10, adopted by WHO, where periodontitis is located in section K04 - diseases of the pulp and periapical tissues. But, according to dentists, a more detailed description of all stages of periodontitis is presented in the International Classification of Dental Diseases ICD-C-3 based on ICD-10, but which has some differences with the accepted Classification. Thus, according to these classifications, several types of periodontitis are distinguished: K04.4 Acute apical periodontitis of pulpal origin Acute apical periodontitis NOS*. This is a “classic” type of disease with a clearly defined etiology and clinical symptoms: swelling, tissue infiltration, inflammation, which can be serous - this stage lasts 1-2 days, is characterized by constant pain, especially with pressure on the tooth; serous-purulent - duration about 2 weeks, swelling of soft tissues, hyperemic mucosa, tooth mobility is observed; purulent-necrotic with the formation of an abscess. K04.5 Chronic apical periodontitis (Apical or periapical granuloma. Apical periodontitis NOS* .
This stage of the disease is the outcome of the acute stage and means that the source of infection has been present for a long time - from several weeks to several months. At this stage, the patient feels almost no pain. In the tooth cavity in the area of the root apex, granulation tissue growth is observed. Under favorable conditions, this tissue encapsulates, forming a granuloma, which can be sterile or infected. It is not connected to the alveolus, but with its fibers passes directly into the periodontium, causing excessive formation of cement at the root apex or, on the contrary, promoting bone resorption. Hardening of the formation and disappearance of the source of inflammation is considered a favorable outcome, which becomes possible as a result of high-quality treatment and filling of the canals. An unfavorable outcome in the absence of treatment is a complication in the form of subcutaneous odontogenic granuloma.
K04.6 Periapical abscess with cavity Tooth (dental) abscess with cavity. Dentoalveolar abscess with cavity. Previously, this code corresponded to Periapical abscess with fistula , which was divided into:
K04.60 Fistula communicating with the maxillary sinus.
K04.61 Fistula communicating with the nasal cavity.
K04.62 Fistula communicating with the oral cavity.
K04.63 Fistula communicating with the skin.
K04.69 Periapical abscess with fistula, unspecified. This stage of periodontitis is characterized by the absence of pain, as there is an outflow of infectious-toxic contents (exudate) from the periodontal area into the root canal of the tooth, and then into the oral cavity. Another option may be the penetration of purulent contents through the fistula into the oral cavity, maxillary sinus, nasal cavity, and skin. Granulation tissue grows, fills the fistula tract 4. K04.7 Periapical abscess without cavity Dental abscess NOS. Dentoalveolar abscess NOS. Periapical abscess NOS. This code in ICD-C-3 corresponds to Periapical abscess without fistula , which was characterized by the fact that the absence of a fistula increased the amount of exudative content in the periodontal area, which caused severe pain, increased swelling and ultimately the formation of an abscess 5. K04.9 Other and unspecified diseases of the pulp and periapical tissues 6.
Acute process
Acute apical periodontitis (ICD-K code 04.4) is of pulpal origin - irreversible pulpitis or a consequence of poor-quality root canal passage. With a pulpal origin, the inflammatory process from the inner chamber of the tooth with the neurovascular bundle passes to the apex of the root. The patient begins to complain of constant aching pain in the area of the causative unit. The soft tissues of the face do not change, and the lymph nodes are palpated slightly painfully. In the oral cavity, we see the unchanged mucous membrane of the disturbing unit, which can be intact or sealed. Percussion is sensitive, but probing is not.
Treatment methods for periodontitis
Modern methods of treating periodontitis can be divided into two large groups - conservative and operative (surgical). All methods follow the same goals: eliminating the source of infection, that is, eliminating inflammation in the periapical area, eliminating the pathogenic effect of an odontogenic inflammatory focus on the body, regenerating the structure of periodontal tissues, preserving and/or restoring tooth functions. In each case, the method is selected individually and only on the basis of a thorough diagnosis, including an examination of the oral cavity, an OPTG image, CT and targeted X-ray images. Conservative methods are divided into therapeutic and physiotherapeutic. In general, they are effective in most cases. Difficulties that may arise in the process of conservative treatment are associated with the duration of the regeneration processes of the focus of destruction in the periapical region, as well as with the anatomical features of the already complex structure of the canal system of the tooth. Therapeutic treatment of periodontitis is a complex of endodontic measures, including: preparation of a diseased tooth, expansion of canals to a conical shape for ease of work in them, cleaning of canals from decayed root pulp and canal walls from layer(s) of infected dentin, therapy using antiseptic and antibiotic drugs to destroy pathogenic microflora, filling. If the treatment requires changing the medication in the canals, a temporary filling is first installed and only after the end of treatment the canals and the tooth as a whole are filled. The filling should ensure complete sealing of the canal and its branches. After filling, the doctor may prescribe drug therapy aimed at stimulating the regeneration process. In many cases, this therapy is combined with physiotherapeutic procedures. Physiotherapeutic treatment in most cases is combined with endodontic treatment or complements it. It includes UHF procedures, intracanal electropheresis, laser or magnetic therapy and ozone therapy. These additional treatment methods are determined and prescribed by the attending physician, according to the clinical picture and general physical condition of the patient. Surgical methods of treating periodontitis are used only if conservative treatment is ineffective, insufficiently effective or impossible for clinical reasons. In most cases, tooth-preserving operations are used, that is, surgical interventions that eliminate the cause of the disease, but preserve the tooth as a unit of the dentition. Such operations include resection of the apex of the tooth root, indicated in the presence of a granuloma or cyst, during which infected and modified tissues are removed along with partial cutting off of the tooth root. For the same purpose, cystectomy or the PARCH-2 method can be used - a surgical intervention that involves complete removal of the cyst with excision (in most cases) of the root apex containing the infected apical deltas. In order to hermetically “seal” the canals, after resection of the apex, the retrograde filling method is used. The root amputation operation allows, by removing one of the tooth roots affected by the disease, to keep the tooth in place while preserving its coronal part, and hemisection involves removing one of the roots along with the adjacent coronal part, if the second root has not entirely undergone pathological changes.
In order for the treatment of periodontitis to be as effective as possible, all its stages, regardless of the treatment method used, are carried out using the most modern dental instruments, drugs and always using a dental microscope. But, rarely, in severely advanced cases of periodontitis, when all other methods are powerless, an operation to remove a tooth is performed as gently as possible with minimal traumatic effects on soft tissue. After tooth extraction, the resulting cavity must be filled with osteoplastic materials—preservation.
Apical periodontitis: pathogenesis
Why does inflammation appear in the peri-root zone? Pathogenic bacteria in tissues are the most likely cause of apical periodontitis. It is called an infectious form of periodontitis, it is a logical continuation of untreated caries, which subsequently develops into pulpitis. If the patient continues to ignore the symptoms and does not seek treatment, the pulp dies, allowing pathogenic bacteria to enter the periodontium through the apical foramen.
Another cause of the disease can be mechanical damage - a blow, bruise, displacement or fracture of a tooth. Then the patient is diagnosed with traumatic periodontitis.
The third reason is the penetration of caustic, potent substances into the peri-root tissue, for example, medications. Almost always this is a consequence of a medical error, most often - inaccurate treatment of pulpitis. Such cases are called drug-induced apical periodontitis.
Treatment of periodontitis and retreatment of tooth canals
Particular attention should be paid to the treatment of periodontitis with already obturated tooth canals, that is, teeth whose canals have previously been subjected to endodontic treatment. “Re-treatment” of such canals is an extremely labor-intensive and time-consuming process. The main difficulty is that clearing the canal of filling material is many times more difficult than carrying out the initial cleaning of odontogenic microflora and removal of the pulp (dental nerve) with subsequent sanitation.
When filling canals, the dentist is forced to focus not on the anatomy of the canal, but on the material with which it was filled during filling. This “blind work” requires the highest qualifications and extensive practical experience of the treating doctor. To remove obstructive materials from the root canal, for example, gutta-percha, in cases of retreatment, mechanical, chemical methods and their combination are used. The mechanical method involves working in the dental canals with instruments - files and profile files, and the chemical method - dissolving hard tissues with reagents. To date, a clear algorithm for repeated endodontic treatment when working with files and solvents has not been developed, depending on the manipulations in the apical, middle and mouth parts of the root canal 7. The next difficult stage after cleaning from filling materials in the treatment of periodontitis with previously obturated tooth canals is canal sanitation .
This stage plays a dominant role, since in order to significantly reduce the likelihood of a relapse of the inflammatory process, it is necessary to carefully carry out the treatment. In this regard, the dentist often places antiseptic medications into the canal for a while at this appointment. The crown part of the tooth is closed for this period with a temporary filling. After the time interval set by the doctor, further treatment is carried out - hermetically sealing the tooth canals and installing a permanent filling.
In cases where, while the integrity of the root is preserved, the coronal part of the tooth is severely damaged and subsequent prosthetics are required, after sanitation and before filling, an anchor or fiberglass pin is inserted into the canal. Then, after filling, an artificial stump is built up from composite materials, and only after this the process of creating and installing a dental restoration begins. In view of these difficulties, even the pinpoint accuracy and high qualification level of the doctor cannot guarantee 100% success in unfilling, subsequent sanitation and complete tightness during new obturation of such tooth canals. This is explained by the fact that small branches of the canal, especially the lateral deltas, may be inaccessible or difficult to navigate even with the most modern and ultra-thin endodontic instruments.
To achieve the best results in the treatment of previously obturated tooth canals, control targeted photographs are taken at each stage. This allows the dentist to avoid intensive instrumental and mechanical treatment and completely clean the canal from microbial contaminants, etc. Maintaining this balance is one of the main tasks of the doctor, since, without achieving balance at this stage, all this can lead to complications such as perforation of the tooth root wall, decreased mechanical resistance of the tooth, relapse of periapical inflammatory processes and, sooner or later, will lead to tooth loss. Therefore, the goal and main task of the dentist is to ensure the clinical and radiological success of endodontic treatment.
Effective treatment of dental periodontitis is an important and pressing problem of modern practical dentistry. The need to solve complex problems leads to the development and implementation in practice of clinicians of new approaches to mechanical treatment of root canals, new irrigation protocols, new technologies for filling canals, new principles of post-endodontic dental restoration, and requires the creation of new instruments and devices, medications and filling materials. Today, the key to the success of endodontic treatment is three-dimensional cleaning and obturation of the entire root canal system with sealing of all branches of the apical delta canals, including the lumen of the dentinal tubules.
Comments
I heard from a friend that her periodontitis was treated extremely unsuccessfully. At first, they fumbled at the dentist, shelled out a considerable amount of money, and in the end the tooth was told to be removed. What is the likelihood that a tooth with periodontitis will be saved for a long time? Or is it easier to remove?
Alla Ufa (08.11.2021 at 21:34) Reply to comment
- Everything depends on the experience and qualifications of the general practitioner, endodontist, as well as the materials, methods, and diagnostic and control measures he uses for treatment. So, if the doctor adheres to strict regulations in his work, correctly determines the length of the canals and carries out hermetic filling, and performs diagnostics at each stage, then it is possible to save the tooth for many years. It is even better if during treatment the specialist uses high-precision equipment, for example, a dental microscope. This device allows you to visually enlarge the treatment area many times over, so that the doctor will not miss a single pathological area, but will preserve healthy tissue in full.
Editorial staff of the portal UltraSmile.ru (09.11.2021 at 10:35) Reply to comment
Ten years ago I had a root cyst removed, but the tooth became darkened and chipped. Now I understand, after reading your articles, that I should have sealed it faster. Or is this still a medical error?
Victoria (07.12.2021 at 13:38) Reply to comment
It often hurts to bite on one of the teeth. The gum above it is slightly swollen. But there are no other signs of the disease, as well as a fistula. Is it possible that the cause of the problem is periodontitis? How can I check this?
Kira (07.12.2021 at 17:22) Reply to comment
How long does it take to treat periodontitis and what is the likelihood of re-exacerbation after treatment? Are there special procedures that can be performed at home for the purpose of prevention?
Irina (12/08/2021 at 09:15) Reply to comment
Write your comment Cancel reply
Complications
Periodontitis is dangerous due to rapidly developing serious complications, so it is extremely important to immediately consult a dentist at the first symptoms. The initial form of acute periodontitis very quickly, within a few days, turns into a purulent form, and then into an abscess. At the stage of chronic periodontitis, fistula tracts are formed, which cause suffering to the patient and significantly increase the treatment period.
In addition, we must not forget that periodontitis destroys the bone tissue surrounding the tooth, and is also a chronic odontogenic inflammatory focus, therefore it significantly reduces the patient’s immune status and contributes to the complication of various somatic diseases. In addition, Swedish scientists from Orebro University recently discovered and proved the effect of periodontitis on the cardiovascular system. The reason for this influence is the activity of the bacterium Porphyromonas gingivalis, which is a common pathogen of periodontitis. This bacterium disrupts the functioning of the gene responsible for controlling inflammation in the coronary arteries, contributing to the occurrence of atherosclerosis and heart attacks 8.
Diagnostics
Diagnosis of apical periodontitis in acute and chronic forms is objectively very similar, therefore, it is necessary to use basic and additional diagnostic techniques.
Basic:
- collection of patient complaints and medical history;
- probing;
- percussion, palpation and determination of tooth mobility;
- X-ray image.
Additional:
- Pulp EDI (reduced to 200 µA);
- determination of jaw ratio;
- the presence of a fistulous tract;
- thermometry (cold tests).
To accurately diagnose and distinguish between exacerbation of chronic or acute forms of apical periodontitis, therapists at the West Dental clinic can use sterile instruments, Pax-i3D (CBCT and OPTG on one equipment), a powerful Leica M320 microscope (for examining hard and soft structures of the oral cavity) .
Treatment quality criterion
High-quality, effective treatment of periodontitis requires pinpoint precision when working in tooth canals that have a complex shape and individual anatomical features. Obturation (sealing) of canals is based on the principle of “three pillars”: the canal must be sealed to its entire length, along all micro-branches, without pores and air cavities. This requires high qualifications and extensive experience of the attending physician, as well as the use of modern equipment - endomotors, apex locators, files, dental microscope. Modern endodontic treatment is a high-tech medical procedure and is based on new medical, technological and ergonomic principles, which obliges clinics to be equipped with modern equipment, and doctors to regularly improve their level of professional competence.
Recommendations after treatment
After the first stage of treatment, it is necessary to use a cotton swab before each meal to prevent its penetration inside. Next, the tampon is thrown away, and the oral cavity is cleaned by rinsing with water and an antiseptic. You should refrain from eating for 2-3 hours after the second stage of treatment, as local anesthesia is used. To prevent the re-development of apical periodontitis, it is recommended to maintain proper oral hygiene and brush your teeth thoroughly.
Indications
Indications for the use of conservative treatment methods are considered to be all types of periodontitis, provided that the canals have good patency, but often such methods are supplemented with surgical techniques for the greatest effectiveness of treatment. Most often they are resorted to in cases where cystic or granulomatous formations are detected, canals are obstructed, the canals have an extremely complex structure, on “retreated” teeth - when the canals are sealed with old cement fillings and they cannot be removed. In addition, surgical methods are used if fragments of endodontic instruments are found in the canals, as well as in cases where restoration of the crown part of the tooth to its full functionality involves the creation of a multi-stage, multi-link structure, which raises high doubts about the effectiveness and functionality. Tooth extraction for periodontitis is indicated in cases where the tooth is severely damaged and its restoration is impossible, when methods and drugs for relieving pain symptoms are ineffective, in the presence of a purulent inflammatory focus, the elimination of which by drainage seems impossible. The final decision on the choice of technique and method of treating periodontitis in each specific case is made by the attending physician, taking into account all the features of the clinical picture of the disease and based on his experience, qualifications, preferences, as well as the capabilities of the clinic. After all, ultimately, it is the doctor who is responsible for the provision of medical services.
Age restrictions
Periodontitis can occur in a person of any age, and there are no age restrictions for its treatment. Pregnant women are treated with special care, since, on the one hand, periodontitis is a dangerous source of infection that reduces immunity and can threaten the adequate course of pregnancy, and on the other hand, highly effective drugs with a strong effect can also threaten the development of the fetus. Therefore, treatment of periodontitis during pregnancy and lactation is carried out using the most gentle methods and drugs. But in order to prevent such situations, it is necessary to carry out routine monitoring, sanitation and medical examination at any age, and even more so during periods of pregnancy planning, as well as the prenatal period.
Prognosis and prevention
The prognosis is positive if it was possible to start treatment on time after diagnosis and prevent chronic periodontitis. Lack of treatment and a competent approach will lead to the growth of cysts and granulomas, so it will not be possible to save the tooth (extraction will be required). For preventive purposes, it is recommended to visit the dentist twice a year for professional cleaning and examination. Be sure to regularly brush your teeth, use mouthwash and floss. If you notice symptoms of the disease, immediately make an appointment with a specialist.
Price
The cost of periodontitis treatment is always strictly individual and consists of a combination of factors. These include diagnostics at the initial and intermediate stages of treatment, the diagnosis made and the algorithm of treatment measures adopted on its basis, the number of visits, drugs, equipment and technologies used in treatment, the work of specialized specialists if necessary, the level of qualifications of the doctor.
Periodontitis is a very serious disease of the teeth and the dental system as a whole. Failure to consult a doctor in a timely manner and attempts at self-medication can lead to serious complications, including those that can threaten your life. At the first appearance of symptoms, you must urgently visit the dental clinic! Be prepared for long-term treatment, which involves multiple visits to the doctor, since the treatment of periodontitis consists of several stages, each of which cannot be started without diagnostically proven effectiveness of the previous one. Only this approach to treatment, combined with the professionalism of the doctor and the patient’s strict, vigilant attitude to all prescriptions and recommendations, is a guarantee of high-quality treatment and reliable protection against relapse for several years.
According to antiplagiat.ru, the uniqueness of the text as of October 16, 2018 is 99%.
Key words, tags: caries, pulpitis, bone tissue destruction, cyst, odontogenic cyst, flux, OPTG image, tooth-preserving operations, resection of the apex of the tooth root, cystectomy, root amputation, dental microscope, preservation, tooth extraction .
1 I. Zimin “From the history of dentistry.” 2 “Teeth and dentistry. Essays on history” / K.A. Pashkov. – M.: Veche, 2014. – 240 p.: ill. 3 Britova, A. A. Endodontics. Diseases of the dental pulp and periapical tissues: textbook. manual, 3rd ed., rev. and additional / A. A. Britova; NovSU named after. Yaroslav the Wise. – Veliky Novgorod, 2016. – 171 p. 4 https://elestom.ru/recommends INTERNATIONAL CLASSIFICATION OF DENTAL DISEASES ICD-C-3 BASED ON ICD-10. 5 https://elestom.ru/recommends INTERNATIONAL CLASSIFICATION OF DENTAL DISEASES ICD-C-3 BASED ON ICD-10. 6 https://mkb-10.com 7 Kleshchenko A. V. Improving the technique of unfilling root canals of teeth obturated with gutta-percha: Dissertation of a candidate of medical sciences: 01/14/14 / Kleshchenko Alexander Viktorovich; (Place of defense: Moscow State Medical and Dental University). - Moscow, 2011 - 93 p. 8 Report of the American Society of Microbiology based on the work. Author: Tobjörn Bengtson, presented by the Faculty of Clinical Medicine, School of Health Sciences, Örebro University, Sweden. * NOS is an abbreviation for “not otherwise specified,” meaning “unspecified” or “unspecified.”