Three-step algorithm for treating abdominal pain
Why painkillers don't help
Let's start with the simplest question: what should you do if discomfort appears in the abdominal area?
Of course, take a pill! For many of us, the answer is... "obvious." A person who cares “too much” about health, much less knows “more than necessary” about it, looks strange. From the point of view of many around him, he simply has nothing to do! The results are obvious: 45% of Russians, feeling pain in the stomach, grab analgesics... And only 28% take antispasmodics. Moreover, over the past six months, every sixth person felt pain in the abdominal area. Women are more often affected. Why is an analgesic dangerous for abdominal pain?
Because it will not eliminate the true cause of the unpleasant sensations, but will disguise it. Indeed, in 60% of cases the culprit of the pain syndrome is spasm.
What is a spasm?
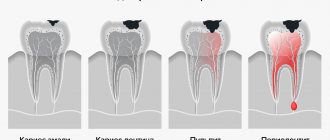
This is an excessive contraction of smooth muscle cells in various organs. In our case we will talk about the digestive system. Inflammatory process - for example, gastritis, enteritis, colitis or ulcers, poisoning and other exposure to pathogenic microbes, a foreign body in the cavity of the digestive organ (a part from a toy in the stomach or a stone in the gall bladder), an imbalance of the substances we need - vitamins and microelements... Because of this, our organs, which are one way or another responsible for digesting food, feel uncomfortable and painfully contract. Analgesics do not act on the cause of the pain, and they will only affect the transmission of nerve impulses, and will not remove the spasm. Plus, as was said earlier, they will mask the pain - and the doctor will not understand anything. Or he will understand, but it’s too late. After all, the remaining 40% of abdominal pain - 4 cases out of 10 - are conditions in which you need to call an ambulance!
Acute pancreatitis, appendicitis, perforation of an ulcer, rupture of an aneurysm of blood vessels in the abdominal cavity, severe inflammatory diseases in women. Peritonitis is an inflammation of the peritoneum, which occurs not only when the appendix ruptures, but also when “treating” gynecological diseases through patience. A stone that has passed out of the gallbladder and blocked the bile duct. If you take an analgesic, it will be difficult for the doctor to understand where the cause of the illness is. And precious time when emergency surgery should have begun will be lost. The antispasmodic will not affect the sensations caused by acute cholecystitis, perforation of an ulcer or rupture of the appendix. The pain will not decrease.
What happens if you “treat” ordinary chronic gastritis with an analgesic?
Painkillers of this type are harmful to the gastric mucosa (and other digestive organs). If you take non-steroidal anti-inflammatory drugs for just a week, then one in five will have a stomach ulcer. And one in seventy will experience gastrointestinal bleeding. What if such patients also take analgesics to relieve pain? “Harmless and safe” drugs for pain relief have their side effects. Therefore, non-steroidal anti-inflammatory drugs and other analgesics should be taken under the supervision of a doctor! Turning them into daily medicine is dangerous. By the way, how long can you “treat yourself” with painkillers?
What to do if your stomach hurts?
In 2002, Vladimir Trofimovich Ivashkin, academician of the Russian Academy of Medical Sciences, chief gastroenterologist of Russia, director of the Clinic of Propaedeutics of Internal Diseases, Gastroenterology, Hepatology of the First Moscow State Medical University named after. THEM. Sechenov, developed a stepwise algorithm of actions for abdominal pain:
• Stage one – mild pain What to do: if necessary, take an antispasmodic. But: – if the pain occurred once, after unusual or poor-quality food, eating disorders or overeating, this is one situation. And if pain occurs with sufficient frequency, i.e. the stomach hurts sometimes or periodically, or in the morning, or after nervous stress, or even from hunger - the situation is completely different. Go to the doctor for an appointment as soon as possible!
• Stage two – the pain is quite severe and/or long-lasting. What to do: be sure to take an antispasmodic. After this, even if your stomach hurts less or the abdominal pain stops altogether, consult a doctor immediately!
• Stage three – very severe pain! Or pain that gets worse. If your stomach hurts unbearably, the cause could be those same 40% - appendicitis, rupture of the gallbladder, perforation of an ulcer, thrombosis of intestinal vessels. What to do: call an ambulance!
Five principles that are important for everyone to know
Abdominal pain is a special pain. Its nature is simply not taken into account by universal drugs for pain relief. And our compatriots, having encountered at least once a modern “optimized” clinic (according to Ministry of Health standards, there is one gastroenterologist per 70 thousand people), try to solve the problem by taking a pill. They will not be told why this is dangerous. After all, there are not enough doctors even for treatment, let alone for prevention and health schools. Therefore, the French manufacturer SANOFI organized a training program - “Pain that is dangerous to anesthetize” with the involvement of gastroenterologists in the educational project. Clinical pharmacologist, candidate of medical sciences, Alexander Maslyakov has developed another instruction for the patient - five principles of action for abdominal pain.
• Principle 1. One of the causes of abdominal pain is spasm, a contraction of the smooth muscles of the digestive organs under the influence of unfavorable factors. For this reason, medications that relieve pain are only first aid. Be sure to find out why your stomach hurts, i.e. what is the condition of the gastrointestinal tract, liver, gallbladder, pancreas and spleen.
• Principle 2. The first choice drug for abdominal pain is an antispasmodic. If you have a spasm of the smooth muscles of the stomach or intestines, you will feel less pain after taking the medicine. And in acute conditions that require urgent surgery, antispasmodics will not mask the pain, and the doctor will have time to understand what happened and how to act.
• Principle 3. For abdominal pain, analgesics are dangerous! They must not be used under any circumstances! A drug of this type will not eliminate the cause of pain - it will simply block the transmission of signals about problems in the body. The brain does not know about problems. Doctors won’t even know about them - after all, the pain sensations are masked, and it’s difficult to make a correct diagnosis.
• Principle 4. If an antispasmodic does not relieve pain within 2–3 hours, consult a doctor!
• Principle 5. If the abdominal pain is severe, if it increases or even simply does not decrease, if you have a high temperature, if your blood pressure is low, if you have nausea and/or vomiting, if you have a headache, call an ambulance immediately!
Be careful! Take care of yourself!
Link to publication: life24.ru
Improved motor control
Physical therapists often seek to correct "dysfunctional" movement patterns. However, this is not entirely clear, for example, some studies show that exercises to improve motor control do reduce pain, but the interesting thing is that this can happen even in the absence of improvement in motor control. Additionally, most of our ideas about what movements are dysfunctional are guesswork and do not fully reflect the complexity and variability of human movement.
Types of lower back pain
Understanding the nature of the pain is very important, because this will help the doctor immediately make an assumption about the diagnosis and prescribe a more accurate diagnosis.
Pain happens:
- acute (occurs due to recent damage, lasts up to 1.5 months);
- aching;
- blunt;
- strong and long lasting;
- subacute (lasts 6-12 weeks);
- variable (transitory);
- chronic (lasts more than 12 weeks).
Low back pain is also divided into primary and secondary.
Primary
associated with chronic changes in the tissues of the spine and muscles. Sometimes the spinal roots are involved in the process.
Secondary
pain indicates another disease. This could be arthrosis, arthritis, or some pathology of the internal organs.
Manual therapy
There is evidence that manual therapy helps with musculoskeletal pain in the short term. Yes, this is true, but there are some nuances.
First, recognize that manual therapy works by modulating the nervous system's sensitivity to pain, not by "fixing" tissue problems such as malaligned vertebrae, fascial adhesions, etc. If you feel better after chiropractic therapy, know that the neurophysiological mechanisms that explain its effectiveness are not much different from what makes most people feel good after strength training or aerobic exercise, which shows good results in the long term.
On the other hand, there is no doubt that for some people, skillful and sensitive human touch represents something unique. If you respond well to what Diane Jacobs calls “human primate social grooming,” then of course you will prefer manual therapy. But don't think that this is necessary to "fix" some problem in your body, like a mechanic fixing a car.
Mind and body
Pain is more than just tissue damage. This is a reflection of how the nervous system and unconscious parts of the brain perceive processes occurring in the body (and beyond). This is especially true when the pain is chronic, correlated with other perceptual disturbances, and appears to be due to psychosocial rather than structural problems. There are many different mind/body practices that focus on improving body awareness through increased awareness and focused attention. Some of them, studies show, actually reduce pain.
If you are interested in this area, consider one of the following treatments for chronic pain:
- Meditation.
- Mindfulness-based stress reduction.
- Yoga.
- Dancing.
- Feldenkrais method.
- Martial arts (especially tai chi or qigong).
Note
- Don’t think that the pain is “in your head” and that the body doesn’t really matter, etc.
- The mind/body method is not a cure for pain, but rather it can be seen as a valuable tool for reducing it.
Acute pain after a fall or injury
A lower back bruise after a fall or blow is the most common back injury, from which even the most careful and cautious people are not immune. The high-risk group includes athletes, people engaged in heavy physical labor (loaders, storekeepers), and children. You can also get a lower back injury if you fall on slippery surfaces (wet floors, ice) or in public transport during emergency braking.
No one is safe from accidental falls
Before providing assistance to a bruised victim, you must ensure that there are no fractures or dislocations. The difference between a bruise and a fracture is damage only to soft tissues (skin, musculo-ligamentous apparatus), manifested mainly by swelling, hematomas and bruises (a symptom of damage to capillaries and small blood vessels).
Improved overall health
Anything you can do to improve your overall health can help with musculoskeletal pain, especially when the pain is chronic and comorbid with other chronic diseases such as obesity or autoimmune diseases.
In this case, working to improve your overall health may be the best way to manage your pain. This means eating a balanced diet, maintaining a work-rest schedule, walking outdoors, aerobic exercise, minimizing emotional stress, and getting good sleep.
Note
Make sure your interest in healthy living doesn't turn into unhealthy behavior.
Ways to get rid of bruises
Most often, the appearance of a bruise is preceded by a strong blow, which cannot be ignored. This injures small vessels, a small amount of blood flows out of them and permeates the subcutaneous tissue and lower layers of the skin. In response to injury, local swelling occurs - a protective reaction of the body. At this stage, the bruise is not yet visible, but you already need to take active action. The goal is to reduce tissue permeation with blood.
In order to quickly reduce swelling at the site of a bruise, it is necessary to use agents that cause vasospasm. Cooling with ice works well for this, but a frozen piece of meat wrapped in film and a thin towel will also work. It must be applied to the site of injury for 20 minutes. After cooling, the ice is removed, but the procedure can be repeated after 15-20 minutes. Constantly keeping the cold near the bruise is dangerous and can cause even more damage.
Home remedies can help relieve swelling. For this you can use:
- a compress made from a solution of vinegar or vodka;
- onion gruel with salt;
- applying a cut aloe leaf;
- half a raw potato.
Folk remedies against bruises can be used at an early stage, immediately after a bruise. A mixture of garlic and vinegar pulp and lavender essential oil, which should be applied to the injury site, are considered effective. But you need to be careful; minor bruises can be treated at home without the help of a doctor.