Alas, some people in our society are susceptible to a bad habit - smoking. We will not describe the dangers of this habit, and provide evidence of how teeth deteriorate from cigarettes. The article is devoted to a more practical issue - when will it be possible to smoke the first cigarette after tooth extraction surgery.
Tooth extraction at the DaVinci aesthetic dentistry clinic is performed using the most modern instruments and preparations. The patient must be given an anesthetic injection so that he does not feel pain during the operation. But still, tooth extraction is an operation. After it, an open wound will appear in the mouth, the size of which depends on the size of the tooth. Sometimes dentists place drainage and stitches in the gum. The wound will prevent you from eating your usual foods for some time, but if the patient follows all the doctor’s recommendations, then no complications will arise, and soon the hole will stop bothering you.
How does nicotine affect teeth?
Before entering the lungs, tobacco smoke passes through the mouth, therefore affecting the lips, teeth and gums.
The following factors influence the condition of the oral cavity:
- Heat. Cigarette smoke enters the mouth of a smoker in a very hot state and affects the integrity of tooth enamel. Exposure to high temperatures may cause it to darken or crack.
- Nicotine and tobacco tars thin out bone tissue, including the jaw. In extreme cases, bone atrophy begins, due to which it will be impossible to install implants without additional bone augmentation procedures.
- Poor effect on the immune system. Nicotine often causes inflammation. Experienced smokers often develop osteomyelitis of the jaw. Often, an addiction leads to mucosal cancer.
- Smoking is one of the reasons for the rejection of dental implants, which can occur at any stage of using a prosthesis.
- When you regularly smoke tobacco products, a thick plaque forms on your teeth, which becomes a habitat for bacteria. Their vital activity disrupts the microflora of the oral cavity, weakening the entire dental system.
- Increased salivation, which irritates the oral mucosa and enamel. Often causes dental diseases.
Medications
Using special medications can significantly increase your chances of quitting smoking. There are three types of medications to treat nicotine addiction:
Nicotine replacement therapy (NRT)
NRTs are the most commonly used medications. They have few side effects and are available both over the counter and by prescription in various forms (chewing gum, tablets, skin patch, inhaler, nasal spray).
NRT medications reduce symptoms of nicotine addiction. Your doctor will help you find the best dosage for you based on your current smoking habits.
Bupropion (Wellbutrin, Zyban). These antidepressants can be used to reduce withdrawal symptoms even if you are not depressed. Common side effects include dry mouth and insomnia (difficulty falling or staying asleep).
Varenicline (Chantix). This medication reduces withdrawal symptoms and, if you start smoking again, may reduce the pleasure you get from nicotine. Common side effects - may cause nausea, dreaming, constipation and drowsiness.
Implantation and smoking
Smoking complicates the operation and increases the likelihood of complications during healing. When a person smokes, thin air is created in the mouth, which prevents the formation of a blood clot. Tissue healing is complicated, and frequent bleeding accompanies the rehabilitation period.
Note: nicotine constricts blood vessels. Because of this, stagnation and suppuration of wounds are formed.
These reasons answer the question: “Why can’t you smoke after having implants installed?” Tissues heal much more slowly than in non-smoking people, osseointegration takes longer. Sometimes smoking after dental implantation causes the sutures placed on the gums to come apart. The risk of implant rejection increases and mobility increases.
Smoking after sinus lift and implantation
Often, before implantation, the dentist prescribes an operation for a smoking patient to increase the bone of the upper jaw, which is otherwise called a sinus lift.
Smoking after bone augmentation surgery or implant installation carries a 10% risk of complications during rehabilitation. The compacted layer of plaque due to tobacco smoke becomes a favorable environment for bacteria and microbes, whose vital activity causes inflammation.
Doctor's recommendations after removal
- 20 minutes after the operation, you need to remove the tampon soaked in antiseptic. During this time, the bleeding should have stopped and the wound should be disinfected. If you leave the tampon in longer, the accumulation of blood and saliva will make it an ideal environment for bacteria to grow.
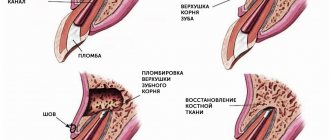
- A blood clot forms at the wound site, which cannot be picked out and spat out, as it will affect the formation of bone tissue, but for now it will become a natural obstacle to bacteria.
- If you have been prescribed rinses, you need to do them very carefully so as not to wash out the blood clot. It is best to simply draw up the solution, hold it in the desired area for 2-3 minutes and spit. Too vigorous rinsing will damage the clot and slow recovery.
- Sometimes the dentist will apply medication to the socket to speed up healing. They also cannot be removed ahead of time.
- Teeth brushing and rinsing can be done one day after surgery. Only movements with the brush must be careful so as not to remove the blood clot.
- After a complicated wisdom tooth extraction, your dentist may prescribe antibiotics to prevent the infection from spreading. The patient needs to follow the treatment regimen.
- To relieve pain, it is better to apply ice to the cheek; if the pain does not subside, you can take a painkiller.
When can you smoke after dental implantation?
Dentists recommend quitting smoking 2-3 weeks before surgery. It is worth quitting smoking to reduce the negative impact on the health and beauty of your teeth.
After installation of implants, you should refrain from smoking for a month, or minimize the number of cigarettes you smoke.
If you cannot quit smoking, you can use nicotine patches or e-cigarettes. E-cigarettes, smokeless and vaping devices are believed to be less harmful because they do not emit tar. However, the nicotine they produce still causes damage to the body and also complicates healing.
If you are not ready to quit smoking, your dentist will not be able to guarantee successful osseointegration. True, the risk of rejection of the structure is present regardless of smoking. Some implantologists estimate the service life of implants in smoking patients to be up to four years, while in non-smokers this period reaches ten years.
People who smoke and have implants need to pay careful attention to removing plaque from their teeth so that harmful microorganisms do not develop a habitat.
Why go to the plastic surgeons of the Pirogov Clinic in St. Petersburg for the best results from mammoplasty?
Plastic surgeons of the clinic named after. N.I. Pirogov has accumulated successful experience in aesthetic and reconstructive breast correction surgeries since 1999. We perform all types of mammoplasty: breast augmentation (endoprosthetics), lift (mastopexy), reduction mammoplasty, correction of gynecomastia, asymmetry and other defects. By contacting us, you can be confident in the high standards of preoperative examination, first-class aesthetic results and the professionalism of our doctors. On our website you can view the portfolio of each plastic surgeon and read reviews about him.
We offer our patients:
- Services of the best plastic surgeons in St. Petersburg, whose professional successes are annually noted by independent experts and industry leaders, as well as by the patients themselves.
- Promotions and special offers (all inclusive) at affordable prices;
- Free face-to-face consultations with plastic surgeons for primary patients.
- Availability of all highly specialized medical specialists whose assistance may be required in one place.
- Our own laboratory, which allows you to quickly obtain accurate diagnostic results - we can send the results of preoperative examinations by email, if that is more convenient for you.
- Operating rooms equipped with new generation medical equipment.
- High comfort and luxury rooms.
- The ability to consult with plastic surgeons remotely using the Online Clinic service.
- Interest-free installment plan for plastic surgery.
- Organizational assistance from a regional manager for patients from other cities.
How does an implant take root in a smoker?
The following factors influence the osseointegration of a smoking patient:
- Burns to the mucous membrane due to regular exposure to hot smoke. This provokes hyperkeratosis, which slows down reparative processes. The gums heal worse, and there is a risk of peri-implantitis.
- The functioning of the salivary glands is disrupted, which leads to chronic drying of the mucous membrane. This affects not only the gums, but also the balance of the oral microflora - the number of harmful microorganisms increases, which ultimately provoke peri-implantitis or inflammation of the gums around the implant. This may lead to failure of the structure.
- Nicotine constricts blood vessels, causing spasms. The speed of blood flow slows down, oxygen reaches the tissues less well, and the injured area receives fewer vitamins and building elements. The implant fuses with the bone less well.
- The immune system weakens - the dental system is exposed to the negative influence of bacteria. As a result, inflammation occurs at the implant site.
MYTHS ABOUT SMOKING CESSATION
Myth: Smoking is a completely personal choice.
Fact: In addition to nicotine, tobacco contains addictive chemicals, which is why many people who start smoking quickly become addicted to nicotine.
Myth: There is no point in quitting smoking if cancer is diagnosed.
Fact: It's never too late to quit smoking. People who quit smoking after being diagnosed with cancer live longer, have a better chance of successful treatment, experience fewer side effects from treatment, recover faster and have a better quality of life.
Myth: Quitting smoking is too stressful for patients undergoing cancer treatment.
Fact: Although nicotine addiction is difficult to overcome and quitting can be uncomfortable, the benefits of quitting outweigh any discomfort associated with it.
Myth: Smokers can stop using tobacco on their own without needing a doctor's help.
Fact: Doctors and other health care providers can provide support, information, and medication to help people quit smoking.
Myth: Most tobacco treatment treatments are ineffective.
Fact: There are medications that can help you cope with nicotine addiction and increase your chances of successfully overcoming it. Ask your doctor for help.
Is it possible to smoke after the implant has taken root?
The dentist cannot prohibit the patient from smoking; he can talk about the consequences, as well as give advice on how to quit the bad habit. Many people resume smoking when the implant takes root, that is, after 1-2 months. Tobacco smoke destroys bone, which provokes implant rejection. Bone separation also occurs in non-smokers, but smoking only increases the risk. Gradually, the gums may recede down to the body of the rod.
Nicotine poses a risk of peri-implantitis even after the implant has taken root. The gums change color and may turn red or, on the contrary, turn pale or blue. In critical cases, an abscess may form. To prevent possible complications, you need to take good care of your oral hygiene and visit your dentist regularly.
Talking to your doctor about your tobacco use
Many cancer patients are embarrassed to tell their doctor about their habit of smoking or chewing tobacco. They fear that the doctor may judge them or that they may receive less support and assistance from health care providers. Other people think that quitting smoking after being diagnosed with cancer doesn't make sense because they already have cancer and using tobacco can help relieve stress after a scary diagnosis. However, none of these statements are true. There are actually significant health benefits associated with quitting tobacco use, even after cancer has been diagnosed, and the health care providers involved in your care are committed to helping people who want to achieve this goal.
It is important to talk to your doctor or health care provider about your behavior. People who use tobacco products daily have a strong nicotine addiction. This addiction will be difficult to overcome, even if you are motivated to quit. It is necessary to determine the degree of nicotine addiction, which will help the doctor prescribe appropriate treatment. This will help you quit smoking and continue living without dependence on nicotine.
Your doctor needs to know the following facts about your tobacco use:
- Have you smoked at least 100 cigarettes in your life?
- Do you currently smoke
- Do you smoke within the first 30 minutes of waking up?
- How many years and how many cigarettes per day have you smoked regularly?
- At what age did you start smoking?
- How long have you not smoked (if you quit smoking)
- How many times have you tried to quit smoking and how long did each attempt last?
- What methods have you used or are currently using to try to quit smoking?
- Does anyone in your family smoke?
- Do you smoke at work?
- Do you use or have you used other types of tobacco besides cigarettes and how often have you used them?
- Has your tobacco use changed since cancer was diagnosed?
What to do -
Below we will discuss recommended implantation techniques and types of implants for smokers. Below we will talk about two types of implants, which are very different from each other. Firstly, classic traditional implants (in the professional literature they are called “crestal”), which are installed in the spongy bone of the alveolar process of the jaws.
Secondly, about the so-called basal or single-phase implants, which are installed in the deepest layers of the bone. Such implants are safer for smokers in general, and for heavy smokers, they are probably the only reasonable alternative.
When installing classic (crestal) implants –
As we have already said: traditional type implants are installed in the same parts of the bone (cancellous bone) in which the roots of your own teeth are located.
This means that the zone of osseointegration of these implants will begin immediately under the gum mucosa. Thus, the upper part of the osseointegration zone (located around the implant neck) will be almost directly affected by both nicotine and pathogenic bacteria. What to do with all this?
- Firstly – you should choose the right implant model... the success of implantation is largely based on the special properties of the implant surface and, it must be said, that the surfaces of implants from different manufacturers are absolutely not equivalent. As we said above, a history of smoking reduces both the rate of osseointegration and worsens the very quality (strength) of attachment of the implant to the bone.
But there are implant surfaces that have active properties and stimulate osteogenesis on the surface of the implant, which allows, in some way, to compensate for the effects of smoking. The following technologies impart active properties to implant surfaces: the presence of an ultra-hydrophilic surface, surface treatment with fluorine ions, and the presence of a thin layer of phosphorus molecules on the surface of the implant.For example, implants from the following manufacturers meet these parameters: → AstraTech (OsseoSpeed™ surface), → NobelBiocare (TiUnite® surface), → Straumann (SLActiv® surface), → Osstem (CA surface).
- Secondly – the correct choice of implantation technique... the most important thing you need to remember is that for smokers it is not recommended to use simultaneous implantation with immediate load on the implant (i.e. with immediate or early prosthetics). The choice of this technique will be an almost complete guarantee of its rejection.
It is also not recommended to use a one-stage implantation technique, in which a healing abutment is screwed into the implant at the end of the operation, designed to form a gum contour around the implant already at the stage of osseointegration (Fig. 6). With this technique, although prosthetics are carried out in the long term after surgery, due to the presence of such an abutment, the mucous membrane of the gums will not hermetically seal the implant. The latter means that the bacterial microflora of the oral cavity and nicotine will directly affect the area of osseointegration of the implant.The only reasonable alternative when installing crestal implants in smokers would be to choose the classic two-stage implantation technique, in which the implant is tightly sutured with the mucous membrane immediately after surgery (Fig. 7). Thus, the implant is isolated and pathogenic bacteria will not be able to get to it, and the effect of nicotine will be weakened.
Differences between one-stage and two-stage implantation techniques -
When installing basal (single-phase) implants –
Basal-type implants (Fig. 8) differ from traditional implants in that they are installed in a deeper basal layer of bone. Thus, the working part of the implant (with the help of which its osseointegration with the bone is carried out) is located much deeper from the surface of the mucous membrane than is the case with crestal implants.
As a result, pathogenic bacteria and nicotine have virtually no effect on the osseointegration of the implant. Thus, the incidence of peri-implantitis and implant rejection when using the basal implantation technique is minimized even in smokers (24stoma.ru). Other advantages of this technique are that prosthetics will be possible within 3 days after surgery, and there is no need for bone grafting if there is insufficient bone volume at the implantation site.
It must be said that if you are a heavy smoker, then this type of implant is generally the only option for you. To carry out this implantation technique, implants from two manufacturers can be used, you can familiarize yourself with the characteristics of which, see photos and videos of their use by clicking on the links below:
- ROOTT (Switzerland)
- Ihde Dental (Switzerland)
Why do implants fail?
If smoking occurs after implantation, the patient should be prepared for difficulties and adhere to oral hygiene, more about which you can read here. Structures may be rejected for the following reasons:
- Stone formation on metal pins;
- Acute inflammation of the mucous membrane and gums around the structure;
- Poor blood circulation at the implant site;
- Peri-implantitis;
- Implant mobility and loss.
My Tobacco Quit Plan
- Talk to your doctor, nurse, or other health care professional about different options for quitting tobacco use
- Determine the end date of complete smoking cessation
- Enroll in an in-person or online tobacco cessation program
- Find out about medications that can help you quit smoking
- Seek help to identify and eliminate the factors that push me to use tobacco
Online resources to help quit tobacco use:
- https://kurenie-yad.org/
- https://vrednokurit.ru/
- https://stopsmoking.ru/
- https://www.activestop.ru/
- https://www.legkie.org/
Information prepared based on materials from the American Society of Clinical Oncology* The American Society of Clinical Oncology is the world's leading professional association of oncologists of all subspecialties who treat cancer patients. The organization has more than 30,000 members from the United States and other countries. The society has developed standards of care for cancer patients and is searching for more effective methods of treating cancer, funding clinical and applied research, and, finally, methods of treating various types of cancer, which claims 12 million lives worldwide every year. The ideas and opinions expressed in this information leaflet do not necessarily reflect the views of the American Society of Clinical Oncology or the staff of the Division of Coloproctology and Pelvic Floor Surgery. The information contained in this guide is not a substitute for medical or legal advice. To resolve any issues that arise, the patient should consult a doctor. You should not neglect or delay in seeking professional medical advice based on the information in this information leaflet. Mention of any product, service, or treatment in this guide should not be construed as a recommendation by the American Society of Clinical Oncology or members of the Division of Coloproctology and Pelvic Floor Surgery. The American Society of Clinical Oncology and the Division of Coloproctology and Pelvic Floor Surgery are not responsible for any injury or damage to persons or property, or for any errors or omissions arising from or related to any use of these materials.
Why you can’t ignore discomfort after laser correction
The doctor informs each patient that in the first days, even with strict adherence to all recommendations, slight tearing of the eyes, sensitivity to light, and sensation of a foreign body are possible. There is no need to worry about dilated pupils and slightly swollen eyelids.
Temporary consequences will soon pass, but you should definitely pay attention to obvious discomfort and inform your doctor about the unpleasant sensations. In exceptional cases, an allergic reaction to prescribed medications may occur.
Might also be useful:
- Types of laser vision correction at the Smile Eyes clinic
- Laser correction using LASIK method
Rehabilitation period
Carrying out a sinus lift is a real surgical procedure, so patients should adhere to several recommendations to avoid complications, namely:
- take painkillers and antimicrobial medications prescribed by your doctor;
- keep your mouth clean using a soft toothbrush without using toothpaste;
- limit sports activities during the recovery period;
- avoid cold and allergens, as sneezing, coughing and blowing your nose are prohibited at first;
- refuse diving and air travel;
- do not inflate balloons, walk or lift heavy objects;
- eat only semi-liquid or highly crushed foods;
- do not drink drinks through a straw;
- quit smoking and alcohol.
All these rules and restrictions play a significant role in the process of wound healing after surgery. Unfortunately, some patients do not attach much importance to the consequences that such disorders can provoke. For example, air travel immediately after surgery can cause severe bleeding and rejection of implants, and drinking alcohol contributes to purulent processes on the gums, thins the blood and can provoke bleeding. Among all these points, it is not without reason that there is a ban on the use of tobacco products, since this, in the opinion of many, a relatively harmless habit entails the most unpredictable consequences.
Materials and methods
Observational materials from 350 patients who underwent ATP surgery for ESRD were analyzed. The follow-up period after kidney transplantation was 29 years (1985–2014). A total of 229 (65.4%) men and 121 (34.6%) women were observed. The age of the patients was on average 37.1±0.6 years; median age 38 years; minimum 12 years, maximum 61 years.
The main kidney diseases that led to the development of ESRD were chronic glomerulonephritis in 199 (56.9%), chronic tubulointerstitial diseases were observed in 17 (4.9%), congenital kidney diseases, anomalies of the urinary tract - in 23 (6.6% ), diabetic nephropathy - in 11 (3.1%), other nephropathies - in 10 (2.9%) and unspecified nephropathy - in 90 (25.7%) patients.
The average duration of dialysis before ATP was 26.6±1.3 months, the maximum period of dialysis before ATP was 162 months (13.5 years). 342 (97.7%) transplantations were performed using a cadaveric donor, and 8 (2.3%) from living related donors. Three protocols of immunosuppressive therapy were used: 1) cyclosporine + prednisolone + azathioprine; 2) cyclosporine + prednisolone + mycophenolate; 3) tacrolimus + prednisolone + mycophenolate.
The following main outcomes of kidney transplantation were studied: patient status after ATP (alive or not); PAT status (functioning or not); development of chronic transplantation nephropathy (CTN).
At the time of the study, 195 (55.7%) patients remained alive with a functioning graft, 68 (19.4%) lost RAT function and returned to hemodialysis; 87 (24.9%) died. Moreover, 81 (23.1%) patients had CTN at the time of the study. Any loss of PAT (loss of graft function due to rejection or death of a patient with a functioning graft) was considered a loss of PAT. CTN was defined as an increase in serum creatinine concentration of more than 0.13 mmol/L for 3 months or more.
Smoking patients were defined as those who smoked at the time of kidney transplantation. For statistical calculations, the following ATP outcome codes were adopted: for patient status: code 0 - alive, 1 - not alive; for transplant status: code 0 - functioning, 1 - not functioning (lost); for CTN: code 0 - no CTN, 1 - there is CTN.
The analysis used the SPSS application package, version 16. The main statistical methods were descriptive, correlation analysis methods, contingency tables, survival (life tables, Kaplan-Meier analysis), regression analysis (Cox logistic regression). p were considered statistically significant.
<0,05.
Table 1. Patient survival rates depending on smoking status before ATP