Exacerbation of the inflammatory process in the tooth sometimes leads to swelling of the cheek. The symptom of swelling occurs due to inflammation of the periosteum, which in dental terms is called periostitis.
It must be said that swelling indicates that the stage of inflammation is seriously advanced. If the cheek is swollen from a tooth, then most likely the patient ignored the long period when the tooth was destroyed by caries. Then the infection penetrated into the pulp chamber, where the nerve of the tooth is located, and pulpitis began. But even at this stage the patient did not visit the dentist, but endured acute tooth pain with the help of painkillers. Then the pathogenic bacteria penetrated deeper into the periodontal tissues, which connect the root of the diseased tooth with the alveolar processes of the jaw, and from there they reached the periosteum, causing periostitis.
Dental treatment
If the dentist does not treat the tooth correctly or completely, it can cause swelling in the cheek.
Causes:
- Allergic reaction.
It appears in the patient as a result of intolerance to the components of the filling. To eliminate swelling, you should visit a doctor and replace the installed filling with a hypoallergenic one.
- Removal of a tooth.
If the cheek is swollen after surgery, then the patient probably ignored the doctor’s recommendations and ate solid or hot foods.
- Nerve removal.
Swelling occurs if part of the nerve is not removed. It is important to see a dentist immediately so as not to lose a healthy tooth.
- Gum section.
Usually required to remove accumulated pus. If the swelling does not subside while taking anti-inflammatory drugs, this may be a serious symptom that requires the attention of a specialist.
Is it possible without a tumor?
In the vast majority of surgical cases, the doctor causes injury to soft tissues. Including oral tissues. It is impossible to pull out a tooth without disturbing the gum, in which it is held by all its, albeit half-rotten, roots. Therefore, swelling after dental extraction is a common and normal reaction of the body to interference in its work.
Swelling after tooth extraction
Important! There is an important amendment - a tumor is not a pathology if it demonstrates a normal tissue response to injury. And it indicates pathology if it signals the onset of an inflammatory process or other postoperative complications.
What to do if your cheek is swollen
To reduce swelling, you can use one of the following tips:
- Rinse your mouth with a solution of salt and soda.
This remedy has an antiseptic effect and helps destroy pathogens. You can enhance the effect by adding a couple of drops of iodine to the solution.
- Use chamomile infusion to rinse
, sage or other medicinal herbs that have anti-inflammatory properties.
- Apply a cold compress to the swollen cheek
if the swelling is caused by a bite or mechanical injury. This method is contraindicated in patients who have an elevated body temperature or a tumor that develops due to inflammatory processes. Warming compresses are not recommended.
- Lotions with aloe or Kalanchoe juice.
A cotton wool soaked in the juice of the plant is applied to the inside of the affected cheek.
If the described methods do not eliminate the problem, you should seek help from a doctor. The day before, you should not take painkillers and anti-inflammatory drugs, so as not to complicate the diagnosis.
Swelling that is not dangerous
For each patient, tooth extraction is a serious surgical action aimed at healing through injury. When a tooth is extracted, blood vessels rupture and gum tissue is damaged. The longer and more difficult the surgery, the longer the damaged tissue will remain swollen and painful.
Important! Even uncomplicated extraction of a single-rooted tooth leads to swelling, which naturally subsides when impaired blood circulation returns to normal. Physiological tumor of the gingival tissue after extraction is not a complication and does not pose a threat to the patient’s health.
When edema develops, it is important to understand whether the situation is within normal limits or requires medical intervention
Gum swelling is not dangerous in the following cases:
- general condition, despite the presence of a tumor, is satisfactory;
- the temperature is normal or slightly increased only on the day of removal;
- the tumor is localized in one place and does not spread to facial tissues;
- the pain is present, but is fading and lasts no more than five days;
- immediately after the operation, the cheek swells, but no increase in pain is observed, and the swelling subsides within a few hours;
- facial skin or oral mucous membranes are of normal color, without redness;
- there is no tissue decay, there is no unpleasant odor from the gums, and there is no unpleasant taste in the mouth.
As for postoperative pain, it is always present in the background. Simple removal is accompanied by aching pain for three to four days. A difficult one can cause pain for a week.
Pain after tooth extraction is common
The main evidence that everything is normal is a gradual decrease in swelling and pain. If everything happens this way, you don’t need to do anything about the swelling, just watch it. You can take painkillers for pain.
Diagnostics
Dentists and maxillofacial surgeons are involved in determining the cause of swollen cheeks. According to indications, the patient is referred to other specialists: otolaryngologists, ophthalmologists, dermatologists. To clarify the diagnosis, the following procedures can be performed:
- Questioning, general examination
. The doctor finds out when and under what circumstances the cheek began to swell, and determines the presence and dynamics of the development of other symptoms. Detects pain on palpation, changes in skin color and temperature. Evaluates the prevalence of edema and tissue density. - Dental examination.
The specialist assesses the condition of the teeth, gums, oral mucosa, and bone structures. Detects signs of inflammation and suppuration, the causative tooth (if present). - Ophthalmological examination.
Indicated for damage to the lacrimal sac and suspected cavernous sinus thrombosis. It is possible to perform ophthalmoscopy, nasolacrimal test, probing of the lacrimal ducts, and other diagnostic procedures. - Otolaryngological examination
. Necessary for sinusitis, paranasal sinus cyst. Can be supplemented with echosinusoscopy and diagnostic puncture. - Radiography.
An x-ray examination of the tooth is prescribed to clarify the condition of the teeth, an x-ray examination of the jaw or zygomatic bone is prescribed to detect fractures due to injuries of the maxillofacial area, an x-ray examination of the accessory sinuses is prescribed to confirm sinusitis, maxillary sinus cysts. - Sonography
. Ultrasound of the salivary glands is recommended for tumors, adenomas, and other pathologies. Allows you to assess the size and structure of organs, identify stones, space-occupying formations, and signs of inflammation. For symptoms of ENT pathology, an ultrasound of the paranasal sinuses is performed to visualize fluid or tumor. - Lab tests
. Most often, a general blood test is used to confirm the inflammatory process, and a microbiological blood test to determine the pathogen. If a tumor process is suspected, a cytological or histological analysis of the biopsy specimen is performed.
Dental examination
Potential complications leading to swelling
When swelling does not go away for more than seven days, we can talk about the constant progression of inflammation. In this case, it is recognized that the patient has complications. It is very important to establish their causes and nature, and then quickly eliminate them.
There are several most common types of complications that patients usually complain about:
Alveolitis
There is always a small blood clot in the hole that remains in place of the extracted tooth. This is a natural reaction of the body aimed at preventing infection. The clot does not allow bacteria to penetrate inside - the wound gradually heals and heals.
But sometimes the clot is removed. As a result, the tissues remain defenseless, infection can occur and pus can begin to accumulate. In this case, inflammation will become more and more intense and will cover large areas.
Inflammation of bone tissue
Not the most common complication, but you won’t be able to insure against it either. It is usually characterized by the appearance of severe swelling that begins to spread throughout the jaw. In this case, the patient experiences severe pain and is practically unable to open his mouth or chew food normally.
The big danger is potential blood poisoning. Therefore, at the first signs of worsening inflammation, you should contact your doctor as soon as possible.
Gum abscess
Characterized by severe suppuration. If it is not addressed, you may lose other teeth in the row.
Flux
Also called “periostitis of the jaw” in the medical community. An intense inflammatory process, which, in addition to swelling, also manifests itself as severe pain in the jaw, radiating to the temples. The temperature rises and the patient feels very weak. Among the dangers are transition to a chronic form and the development of osteomyelitis.
Neuritis
In this case, severe damage to the facial nerve occurs. Not only the area next to the extracted tooth swells, but also the cheeks, tongue, and larynx.
When is swelling a sign of pathology?
- If swelling does not appear the next morning, but much later (on the third or fourth day);
- If swelling is accompanied by increasing pain;
- If, against the background of edema, the patient’s temperature rises;
- If the swelling is so severe that it makes speech and swallowing impossible;
- If there is a putrid odor from the mouth.
The listed symptoms may indicate that the patient has developed alveolitis. When wisdom teeth are removed, this phenomenon is not so rare, and according to statistics it happens in 20% of cases.
How to treat gumboil on the cheek
Once a tumor develops, antibiotics are often indispensable. The dentist selects them taking into account the stage of the pathology and the characteristics of the body. Antibiotic therapy should be completed to the end, otherwise further treatment will be greatly complicated.
If surgery is required, all activities are carried out in a dental clinic. For any complication, the patient is given local or general anesthesia. The gum is incised and the accumulated pus is completely pumped out. A drainage is placed to quickly remove fluid. The patient is prescribed antibiotics to allow the soft tissues to recover faster. In case of severe damage, the gum is sutured. In the absence of complications, this is not required.
How to remove swelling from the gums through surgery:
- In case of complicated flux, urgent hospitalization in a dental clinic and an operation performed by a dental surgeon are necessary.
- If an inflammatory process is diagnosed due to dental problems, endodontic therapy (cleaning and filling the canals) or root removal will be required.
- Broad-spectrum antibiotics are prescribed to treat infection in many situations. In case of serious complications, combination drugs are used to treat severe swelling, selected taking into account the sensitivity of the pathogens.
- Surgical treatment - incision of the abscess (on the face and oral cavity - the incision is made in both areas), removal of purulent discharge, treatment with disinfectants, installation of drainage. In severe cases, general anesthesia is used.
- Additional therapy - analgesics to eliminate discomfort, antipyretic drugs, large amounts of fluid (if necessary, fluid is introduced into the body by infusion during hospitalization).
Chronic pathology often occurs without pronounced symptoms, pus appears gradually. In this situation, the dentist uses a therapeutic approach, both surgical and conservative. Surgery can be replaced with herbs or antibiotics, or used as an additional treatment after consultation with a specialist.
Swelling of the cheek does not always indicate the presence of a serious pathology.
A tumor after depulpation is normal and does not require serious treatment. When the gumboil gradually grows, pain is observed against this background, and the help of a dentist is required. In case of serious complications, surgical intervention while taking antibiotics is indicated. The doctor's consultation
Why does cheek swelling occur?
A common cause of edema is odontogenic periostitis, or gumboil. The inflammatory process of the periosteum is accompanied by the formation of purulent contents at the base of the root. The causes of gumboil are the spread of infection from a diseased tooth - carious or pulpy. In this case, only surgical treatment of periostitis, an incision in the gum and cleaning out the pus will help relieve swelling.
Another cause of cheek swelling is gingival cysts. If the cystic formation is localized not strictly under the root, but on the side, the gums and along with it the patient’s cheek swell. Getting rid of cysts involves performing tooth-preserving operations or, in advanced cases, tooth extraction. Often the cyst itself does not cause swelling, but after surgery to resect it, the patient receives swelling, which goes away within 2-3 days.
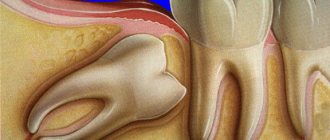
Patients with impacted and dystopic wisdom teeth often suffer from swelling during periods when the tooth is actively trying to erupt.
Symptoms of illness
Depending on the cause, symptoms may vary from case to case. More often with edema, the following symptoms appear:
- swelling on the cheek;
- pain in the causative area;
- difficulties in controlling facial expressions;
- inflammation of the mucous membrane.
It is important to monitor swelling. If it increases, medical attention is required. Reasons to urgently consult a doctor also include increased body temperature, general weakness, purulent discharge from the gums, loss of appetite, numbness and sagging cheeks.
How to relieve the condition at home?
To alleviate the condition before visiting a doctor, you can relieve pain and reduce swelling of the cheek with home remedies.
- A pronounced anti-inflammatory effect is exerted by rinsing infusions made from oak bark or calendula, chamomile, and sage inflorescences. To prepare the solution, two tablespoons of raw material are steamed with boiling water and infused for 15-30 minutes, after which rinsing is carried out three to four times a day.
- The soda-salt solution effectively relieves pain, reduces swelling and has a pronounced antiseptic effect. To do this, the components in the amount of 15 g (1 tsp) are stirred in a glass of warm water and used for their intended purpose.
- Dental ointments and gels, which are applied by application to the affected area 2-3 times a day, have proven themselves well.
- Pharmacy antiseptics are always effective, regardless of the causes of swelling of the cheek and gum tissue. Among the most popular: Chlorhexidine, Miramistin, Furacilin, hydrogen peroxide.
If your health worsens and you suspect an allergy, you need to take antihistamines, such as: Tavegil, Zodak, Suprastin, Kestin, etc. To relieve pain, take analgesics or NSAIDs - non-steroidal anti-inflammatory drugs.
Important! In case of severe swelling of the cheek, “tugging” pain, high body temperature and respiratory dysfunction, urgent hospitalization is necessary. Symptoms may indicate anaphylactic shock or sepsis.
Other causes of cheek swelling
If you have a tooth removed and your gums are swollen, the cause does not necessarily lie in soft tissue damage. Swelling is possible due to the following:
- performing an operation if the patient has a flux;
- complex course of the operation - due to tooth growth in the wrong direction, strong inclination, removal of large teeth with large, intertwined roots;
- inflammation and infection of soft tissues or tooth roots before surgery;
- allergies or other forms of individual intolerance to anesthesia and medications used during removal - therefore it is important to know exactly what components you are allergic to before removal;
- poor antiseptic treatment of the oral cavity and mistakes made by the doctor during tooth extraction;
- chronic diseases leading to complicated recovery - neuralgia, hypertension, as well as a general decline in the body’s immune functions;
- ignoring prescriptions received from the dentist - for example, independently adjusting the dosage or deciding not to take antibiotics.
Most often, patients' swelling does not subside after tooth extraction due to lack of normal care - skipping medications, complete absence or insufficiently frequent disinfection treatment.
Possible complications
Patients face complications due to incorrect care, complex or incorrect removal. Dentistry distinguishes 5 types of complications:
- Alveolitis - to put it simply, this is dryness of the socket. A blood clot always forms in the latter. It does not need to be removed, since the clot protects soft tissues from the penetration of bacteria and infection. If it is accidentally removed, the mucous membrane becomes susceptible to the pathogenic influence of bacteria, and suppuration may develop. Sometimes the inflammation shifts and spreads - a large area of the jaw, cheekbones and eyes become inflamed.
- Osteomyelitis is bone inflammation. With osteomyelitis, acute pain is felt in the upper and lower jaw, and swelling only increases.
- An abscess is suppuration inside the gum. Can move, leading to loosening of the tooth root.
- Flux is a severe inflammation of the jaw, in which the temperature rises and acute pain appears in the area of the jaw and temples.
- Neuritis is an inflammation in which the motor activity of the facial nerve is disrupted. Neuritis is indicated by swelling of the cheek, palate, tongue and larynx.
Flux symptoms
Clinical manifestations of acute periodontitis/periostitis are quite characteristic. Flux manifests itself as sharp pain in the tooth area, intensifying even with light pressure on it. Swelling and redness of the lips, cheeks, enlarged gums, and the tooth is often mobile.
There is an unpleasant odor from the mouth, and sometimes fistulas on the gums. A characteristic sign of gumboil is the appearance of independent pain, weak at first, then intensifying, becoming pulsating and tearing. Its difference from pain with pulpitis is that it is strictly localized and becomes sharp when pressing on the diseased tooth, especially in the form of tapping. The closing of teeth is so painful that many people refuse to eat even liquid food.
Clinical manifestations of acute periodontitis/periostitis are quite characteristic. Flux manifests itself as sharp pain in the tooth area, intensifying even with light pressure on it. Swelling and redness of the lips, cheeks, enlarged gums, and the tooth is often mobile.
There is an unpleasant odor from the mouth, and sometimes fistulas on the gums. A characteristic sign of gumboil is the appearance of independent pain, weak at first, then intensifying, becoming pulsating and tearing. Its difference from pain with pulpitis is that it is strictly localized and becomes sharp when pressing on the diseased tooth, especially in the form of tapping. The closing of teeth is so painful that many people refuse to eat even liquid food.
It is also possible to increase body temperature to 37.5-38.0°C. Severe pain and difficulty eating food force the patient to see a dentist within the next few hours from the moment of illness.
Chronic form of periodontitis
In chronic forms of periodontitis, a different picture is observed. The most formidable and insidious in its course and possible complications is chronic granulating periodontitis and exacerbation of its course. The pain reaction is mild, but often in the vestibule of the oral cavity, in the projection of the apex of the root of the affected tooth, a fistula periodically opens with small purulent discharge.
When the fistula is closed during periostitis, swelling and hyperemia of the mucous membrane in the area of the flux and pain when pressing on the diseased tooth are possible. Chronic granulating periodontitis is diagnosed based on a comparison of clinical manifestations with X-ray data, which shows destruction of the periodontal gap and changes in the jaw bone in the form of “tongues of flame” in the area of the apex of the tooth root. The purulent process in the medullary spaces of the jaw adjacent to the periodontium leads to the spread of infection over a considerable distance.
The vital activity of pathogenic microflora during the long-term existence of a chronic pathogenic focus ultimately leads to odontogenic chronic sepsis. This provokes the emergence, formation or exacerbation of chronic infectious diseases of the heart, liver, kidneys and other organs.
The presence of such infectious foci can dangerously affect the course of pregnancy at any stage; complications such as infection of the female genital area, miscarriage, and disruption of the formation of fetal tissue occur.