Description and location
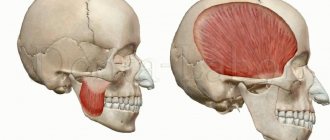
Trigeminal nerve - V pair of cranial nerves
The trigeminal nerve is the fifth of twelve pairs of cranial nerves that arise from the brain. This is the longest, mixed, complexly organized nerve, containing many sensory and motor roots. It received its unusual name due to its division into three main parts:
- The superior sensory nerve is the optic nerve.
- The middle sensory nerve is the maxillary nerve.
- The inferior mixed nerve is the mandibular nerve, consisting of motor and sensory fibers.
Together, they provide sensitivity to the facial and cranial soft tissues, mucous membranes of the nose, mouth, conjunctiva of the eye, teeth, as well as some areas of the dura mater. The motor nuclei innervate the masticatory and some other muscle fibers.
Coming from the pons, the trigeminal nerve is located in Meckel's cavity - the space between the cleft of the cranial shell in the area of the pyramidal depression of the temporal bone, formed by the sphenoid bone. Meckel's cavity is located in the postorbital region, containing numerous venous and arterial vessels, including the cavernous sinus adjacent to the nerve. It is filled with cerebral fluid.
Not far from the nerve lies the carotid (carotid) artery, and its lower node (ganglion) borders on the pyramid of the temporal bone, inside the tubule through which the internal carotid artery passes.
Causes of inflammation
The installation of a dental implant should be carried out taking into account the parameters of the jaw, size, characteristics of the alveolar process and bone tissue of the implanted area. The relief of the canal through which the mandibular nerve bundle passes must be thoroughly studied.
Lack of preparation for implantation and lack of professionalism are the main causes of damage to the mandibular branch.
You can touch or damage the neurovascular bundle:
- needle during anesthesia;
- direct pressure with a long implant;
- tool when forming a dental bed.
Damaging factors include a long period of flap retraction and bone graft harvesting. Restoring sensitivity is a long and problematic process; the task of implantologists is to reduce potential risks to a minimum .
Anatomical structure
The character of TN is mixed. At the base of the brain structures, emerging from the thickness of the bridge with sensitive and motor roots, it is directed forward and slightly to the side, penetrating into the cleft of the dura mater. The sensitive root forms the trigeminal cavity, in which a fairly long ganglion (Gasserian ganglion) lies. The concave part is placed back, and the convex part is placed forward.
From the convex edge, which is located in front, there are three main branches: the ophthalmic, maxillary and non-maxillary nerves. On the inside, the node goes around the motor root, heading towards the cranial foramen ovale. There it reunites with the third branch of TN.
Factors influencing neurological response to nerve injury
— Preoperative screening for neuropathic pain is necessary. Preexisting neuropathic dental pain (PDAP type 1), which exists before surgery, can be caused by many different systemic conditions, medications, and other lesions. It is critical that surgeons recognize presurgical neuropathic conditions because neuropathic pain does not respond to surgery and can often lead to worsening pain. In addition, poorly controlled preoperative pain and nerve damage can cause chronic postoperative pain.
— The main indicators for predicting chronic post-surgical pain are psychological factors, including the level of anxiety, neuroticism (a fundamental personality trait in psychology, characterized by anxiety, fear, rapid mood swings, frustration and a feeling of loneliness. It is believed that neurotic people cope worse with stress and are prone to exaggerate the negative side of a particular situation.), catastrophization and introversion. Thus, the doctor has the opportunity not to perform the surgery of choice (implantation) in such patients, but to decide in favor of an alternative treatment plan.
- The concentration of the anesthetic used is up to 2% lidocaine - the accepted standard, because higher concentrations have a greater neurotoxic effect, which may cause permanent neuropathy. Avoid using multiple (repeated) anesthetic blocks in the same area for the same reason.
— Preoperative medical examination should exclude the following diseases : Raynaud's disease, Erythromelalgia (Mitchell's disease), Irritable bowel syndrome (IBS), Migraines, Fibromyalgia.
—Location of surgery is another factor associated with neurological response. Trauma in the distal jaw is more significant (eg, angle and ramus) than in the mental foramen, because the closer the proximal nerve injury is, the greater the risk of damaging trigeminal ganglion cells and initiating retrograde effects of differentiation into the central nervous system. .
Thus, a thorough interview and examination of the patient, detailed pre-implantation planning based on CBCT data, appropriate visualization of the implantation plan and the use of surgical guides, selection of optimal implant sizes with extended safety zones, use of drill limiters and, of course, an experienced team of doctors who will carry out the implantation followed by early postoperative care, all of which will contribute to safer practice and optimized patient outcomes.
Main functions
The trigeminal nerve is the most sensitive nerve in the face and mouth. It also contains motor tissues responsible for the innervation of the masticatory muscles. Has two sensors:
- The superficial nucleus of the trigeminal nerve, responsible for pain and tactile sensitivity.
- Deep nucleus (proprioceptive), responsible for the perception of free receptors.
Its motor part originates from the motor nucleus. Sensitive tissues are branched processes of neurons of the Gasserian ganglion. Nerve impulses depart from them to nerve cells embedded in the substance of the secreted part of the third brain, which continues the spinal cord.
The superficial nucleus is a continuation of sections of the spinal cord that look like horns. It runs through the medullary pons and bulb of the brain, and also covers the two upper cervical spinal segments.
The deep nucleus is located in the dorsal part of the pontine tegmentum. Receiving sensitive impulses from touch and pressure, it conducts them along the spinal cord through the posterior cords.
The motor nucleus is located in the middle of the deep nucleus. Its impulses exit near the sensory root, connecting with the mandibular nerve, innervating the facial and digastric muscles.
The layout and structure of the trigeminal nerve allows it to perform several important functions for the body:
- provide deep and superficial sensitivity of the eyes, mouth, nose, brain;
- responsible for the motor ability of the head muscles (temporal, chewing).
The trigeminal nerve perceives any touch, including pain, and transmits a sensory signal from the elements eaten or exhaled.
Symptoms of the lesion
You can assume that the mandibular nerve is affected by the following signs:
- numbness of the face from the implantation side: lower lip, chin, tongue, lower teeth, cheeks;
- pain in the implant area;
- the appearance of profuse salivation;
- choking when eating or drinking;
- the occurrence of facial expression and articulation disorders.
A person feels discomfort when caring for facial skin (unpleasant sensations during shaving, applying makeup). Clinical manifestations depend on the type of injury and the depth of the lesion.
Branches of the trigeminal nerve
The ophthalmic branch is divided into three nerves: lacrimal, frontal, nasociliary
. The processes extending from the ganglion, leaving behind the cranial cavity along the superior orbital cleft and foramen ovale, form three large branches.
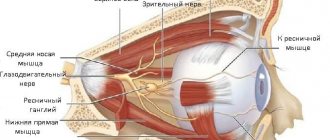
Ophthalmic branch
It comes from the convex area of the trigeminal ganglion and is located in the thickness of the lateral part of the cavernous sinus. It enters the orbital cavity along the superior orbital cleft. Before entering the orbit, it gives off a tentorial branch, which extends backward, dividing in the cerebellar tent. In the orbital cavity, the first branch of the trigeminal nerve divides into three large nerves:
- The lacrimal passes along the lateral orbital wall towards the lacrimal gland. Before merging with it, it receives a connecting branch from the second branch of the TN - the zygomatic nerve. It includes parasympathetic tissues through which the lacrimal gland is innervated. The terminal branches of the lacrimal nerve supply the skin and conjunctiva of the upper corner of the eye with nerve fibers.
- The frontal one is the largest. It extends forward under the superior orbital wall, and then bifurcates into the supraorbital (coming from the orbit, it gives off middle and lateral branches, ending in the skin of the forehead) and the supratrochlear nerve (running above the superior oblique muscle, ending in the skin of the nose, forehead, upper eyelid, corner of the eye).
- The nasociliary goes anteriorly between the eye muscles, giving off the anterior and posterior ethmoidal nerves, long ciliary branches, the infratrochlear nerve and the connecting branch.
Since the elements that make up the visual organ need to move, and the ocular branch is not able to provide this, a ciliary vegetative node is located near it. Through connective nerve tissues and the accessory nucleus, it leads to contraction and unclenching of the pupillary muscles.
Maxillary branch
Heading from the TN, it goes forward, exiting through the round opening into the pterygopalatine fossa. Even in the cranial cavity of the skull, a middle branch branches off from it, accompanying one of the branches of the meningeal artery. In the pterygopalatine fossa, from the trunk of the maxillary branch (MSV), the infraorbital, zygomatic and nodular branches run to the node of the same name.
The infraorbital is considered a continuation of the HFV. Through the region of the infraorbital fissure, it enters the orbit and enters the infraorbital maxillary canal. Further along the infraorbital foramen it goes to the outer surface of the upper jaw, and is divided into small branches:
- lower branches of the eyelids, going to the skin of the lower eyelid;
- external nasal, extending into the outer integument of the nose;
- upper labials;
- alveolar (upper, anterior, middle, posterior), forming the maxillary plexus in the tissues of the upper jaw;
- internal nasal, extending to the mucous membranes of the nasal cavity.
The zygomatic nerve comes from the HFV in the pterygopalatine fossa near the node of the same name and enters the orbital cavity along the infraorbital fissure. There it gives off a connecting branch with parasympathetic fibers that innervates the lacrimal gland. It then goes into the zygomaticoorbital foramen and bifurcates into the zygomaticotemporal and zygomaticofacial branches.
Mandibular branch
It exits the cranial cavity through the foramen ovale. Contains motor and sensory tissues that innervate the chewing muscles of the same name. Motor branches include the masseteric, deep temporal, and pterygoid (lateral and middle) nerves. This group also includes the nerve of the muscle that contracts the soft palate and the nerve of the muscle that regulates the tympanic membrane. Sensory branches include the meningeal branch, buccal nerve, and auriculotemporal nerve.
Many people confuse the trigeminal nerve with the facial nerve, but the second is responsible for motor function, facial expressions and the functioning of certain glands. It cannot be considered identical to trigeminal, especially when carrying out diagnostic and therapeutic measures.
Neuropathy of the buccal nerve.
The causes of the disease can be periostitis, inflammatory diseases of the teeth and gums, traumatic removal of teeth in the lower jaw.
Clinic.
The pain occurs subacutely, is constant, and its intensity gradually increases. First it occurs on the front surface of the gum, transitional fold, and then spreads to the entire front surface of the teeth of the lower jaw and covers the entire area of innervation of the buccal nerve. Numbness is uncharacteristic; an objective examination reveals a decrease in all types of sensitivity in the area of innervation of the mucous membrane of the cheek and vestibular surface of the gums, as well as the skin of the corner of the mouth.
Possible pathologies of the trigeminal nerve
If you have a disease of the trigeminal nerve, you need to consult a dentist.
If the trigeminal nerve is affected, its functions are impaired. Clinical symptoms depend on the tissues of which branch have pathological changes associated with inflammation or pinching of sensory-motor tissues.
Various specialists, including neurologists, dentists, and surgeons, are struggling with the causes and consequences of diseases of the trigeminal nerve. There are at least ten known provoking factors that negatively affect the condition and functionality. Some of them:
- congenital anomalies in the structure and placement of blood vessels;
- injury to the face, head;
- infectious diseases (syphilis, tuberculosis, influenza);
- tumor formations;
- failure of the endocrine system;
- serious dental problems (for example, complicated caries).
General or local hypothermia, severe stress, psychoneurological illnesses - all this provokes unpleasant symptoms in the form of severe pain (shooting and acute), as well as:
- formation of triggers (painful reaction to chewing, brushing teeth);
- facial muscle spasms, numbness in some areas, decreased sensitivity;
- disturbances in the activity of the salivary glands;
- migraine attacks, cephalalgia;
- increase in body temperature.
All diseases affecting the trigeminal nerve are divided into inflammatory and non-inflammatory.
Neuralgia
Involves any pain associated with damage to the trigeminal nerve. It can be idiopathic and secondary. The cause of the appearance of the first form of the disease is difficult to establish, and the provocateurs of secondary neuralgia are most often other diseases.
A distinctive feature of neuralgia is sudden sharp pain, similar to an electric shock.
Gradenigo syndrome, characterized by paralysis of the nerve branches of the trigeminal nerve, as well as trismus of the masticatory muscles, is closely associated with neuralgia.
Neuritis
An inflammatory disease that leads to the destruction of the nerve trunk. Accompanied by burning excruciating pain, itching, and impaired muscle sensitivity. May be accompanied by insomnia, facial distortion, irritability, and fatigue. The patient has difficulty speaking and chewing food.
Caused by infectious processes occurring in the body: meningitis, sinusitis, syphilis, as well as autoimmune diseases that require aggressive treatment.
First signs of damage
The first symptoms of nerve damage are discomfort in the gums, cheeks, and lower lip. Manifestations of the problem are:
- paresthesia, that is, a change in the level of sensitivity without pain;
- dysesthesia with pain in the affected area, a feeling of “pins and needles”, changes in the general sensitivity of the area;
- anesthesia - complete loss of sensation in a certain area.
In some cases, the lingual nerve, which runs from the side of the tongue into the gum tissue, may be affected. This is usually observed as a result of the removal of "eights" (in approximately 2.1% of all cases). When implanted, this nerve is affected less frequently. If this situation occurs, the following symptoms appear:
- salivation becomes profuse;
- involuntary biting of the tip of the tongue appears;
- diction disorders;
- burning sensation, numbness in the tongue;
- loss, change in taste;
- swallowing is impaired.
In 90% of cases, the problems go away on their own within seven to ten weeks; no special treatment is required.
Complications and treatment
Facial asymmetry is one of the possible complications.
Chronic diseases develop with untimely or illiterate treatment of neuralgia and neuritis. As a result, dangerous complications are diagnosed, leading to the following pathologies:
- muscle atrophy;
- decreased sensitivity of the skin, mouth, and nasal cavity;
- facial asymmetry;
- violation of diction;
- deterioration of hearing and vision acuity.
Inflammatory and non-inflammatory processes affecting TN require complex therapy with the use of medications, physiotherapy sessions, and massage. Pharmacological agents include nonsteroidal anti-inflammatory drugs, muscle relaxants, anticonvulsants together with Novocaine blockades, antispasmodics, and sedative tablets.
If traditional therapy does not help, they resort to radiofrequency and microvascular destruction, which causes virtually no complications. In severe cases, surgical intervention is used through microvascular decompression with the placement of a special “protector” between the nerve and the vessel, which helps protect the nerve fibers from clamping and further damage.
What methods are used in treatment
The treatment method depends on the extent of the lesion and is carried out after assessing the sensitivity deficit. With neuropraxia, recovery occurs on its own within 4-6 weeks . No medical attention is required since the nerve structure is not damaged.
With partial degeneration, symptoms subside two months after the injury. For a complete recovery, medical measures will be needed. Numbness for 9-12 months is dangerous due to irreversible degeneration of nerve cells . Microsurgical treatment can be urgent (for an open injury) or planned (for a closed injury).
Treatment tactics for closed injury
- For numbness that does not go away for three months - suturing, transplantation;
- For dysesthesia (perversion of sensitivity) for more than 3 months - revision, decompression, neurolysis, suturing and nerve transplantation;
- If hypoesthesia (decreased sensitivity) lasts for more than 3 months, partial unscrewing or removal of the structure, revision, transplantation, suturing is indicated.
Drug treatment
Indicated for chronic nerve inflammation syndrome. An important point is pain relief. Can be used:
- Antineuralgic drugs:
- Carbamazepine;
- Phenytoin;
- Baclofen.
- Antidepressants:
- Amitriptyline;
- Imipramine.
- Local products:
- ointments with capsaicin;
- acupuncture;
- electrical stimulation;
- physiotherapy.
Diagnosis and prevention of pathologies
When alarming symptoms appear, the doctor collects anamnesis, listens to the patient’s complaints, and conducts a visual examination. Next, he probes the exit points of the trigeminal nerve branches, assessing the degree of their sensitivity and pain. If triggers are identified, a preliminary diagnosis is made, which is confirmed using computed tomography and magnetic resonance imaging. These examinations make it possible to exclude the presence of other pathologies, as well as to detect vascular compression of the trigeminal nerve roots.
There are no specific preventive measures for trigeminal nerve diseases. Experts advise strengthening the immune system, treating infectious diseases in a timely manner, and not overcooling, especially in the summer, sitting under fans and air conditioners.
What is mandibular nerve injury?
By this concept, dentists mean injury to one of the nerves:
- chin;
- lingual;
- alveolar.
Types of injuries include sprain, compression, crushing and rupture - partial or complete. The cause of the stretching is the long-term retraction of the mucoperiosteal flap, which is created by an implant of greater length than necessary. Crush injuries and compression are caused by needle injuries during the administration of anesthesia. Rupture occurs in two cases: when cutting the mucosa or during preparation of the hole for the implant.