The nerves of the eye are usually divided into three groups: motor, secretory and sensory.
Sensory nerves are responsible for regulating metabolic processes and also provide protection, warning of any external influences. For example, a foreign body entering the eye or an inflammatory process occurring inside the eye.
The task of the motor nerves is to ensure movement of the eyeball through coordinated tension of the motor muscles of the eye. They are responsible for the functioning of the dilator and sphincter of the pupil, and regulate the width of the palpebral fissure. The motor muscles of the eye, in their work to ensure the depth and volume of vision, are under the control of the oculomotor, abducens and trochlear nerves. The width of the palpebral fissure is controlled by the facial nerve.
The muscles of the pupil itself are controlled by nerve fibers in the autonomic nervous system.
Secretory fibers located in the facial nerve regulate the functions of the lacrimal gland of the organ of vision.
Innervation of the eyeball
All nerves involved in the functioning of the eye originate in groups of nerve cells localized in the brain and nerve ganglia. The task of the nervous system of the eye is to regulate muscle function, ensure sensitivity of the eyeball, and the auxiliary apparatus of the eye. In addition, it regulates metabolic reactions and blood vessel tone.
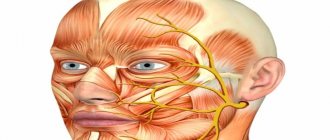
The innervation of the eye involves 5 pairs of 12 available cranial nerves: oculomotor, facial, trigeminal, as well as abducens and trochlear.
The oculomotor nerve originates from nerve cells in the brain and has a close connection with the nerve cells of the abducens and trochlear nerves, as well as the auditory and facial nerves. In addition, there is its connection with the spinal cord, providing a coordinated reaction of the eyes, torso and head in response to auditory and visual stimuli or changes in the position of the torso.
The oculomotor nerve enters the orbit through the opening of the superior orbital fissure. Its role is to raise the upper eyelid, ensuring the work of the internal, superior, inferior rectus muscles, as well as the inferior oblique muscle. Also, the oculomotor nerve includes branches that regulate the activity of the ciliary muscle and the work of the pupillary sphincter.
Together with the oculomotor nerve, 2 more nerves enter the orbit through the opening of the superior orbital fissure: the trochlear nerve and the abducens nerve. Their task is to innervate, respectively, the superior oblique and external rectus muscles.
The facial nerve contains motor nerve fibers, as well as branches that regulate the activity of the lacrimal gland. It regulates the facial movements of the facial muscles and the work of the orbicularis oculi muscle.
The function of the trigeminal nerve is mixed; it regulates muscle function, is responsible for sensitivity and includes autonomic nerve fibers. In accordance with its name, the trigeminal nerve splits into three large branches.
The first main branch of the trigeminal nerve is the ophthalmic nerve. Passing into the orbit through the opening of the superior orbital fissure, the optic nerve gives rise to three main nerves: nasociliary, frontal and lacrimal.
The nasolacrimal nerve passes through the muscular funnel, in turn dividing into ethmoidal (anterior and posterior), long ciliary, and nasal branches. It also gives off a connecting branch to the ciliary ganglion.
The ethmoidal nerves are involved in providing sensitivity to cells in the ethmoidal labyrinth, the nasal cavity, and the skin of the tip of the nose and its wings.
The long ciliary nerves lie in the sclera in the area of the optic nerve. Then their path continues in the supravascular space in the direction of the anterior segment of the eye, where they and the short ciliary nerves extending from the ciliary ganglion create a nerve plexus around the circumference of the cornea and the ciliary body. This nerve plexus regulates metabolic processes and provides sensitivity to the anterior segment of the eye. Also, the long ciliary nerves include sympathetic nerve fibers that branch from the nerve plexus belonging to the internal carotid artery. They regulate the activity of the pupillary dilator.
The short ciliary nerves begin in the region of the ciliary ganglion; they run through the sclera, surrounding the optic nerve. Their role is to ensure nervous regulation of the choroid. The ciliary ganglion, also called the ciliary ganglion, is a union of nerve cells that take part in the sensory (via the nasociliary root), motor (via the oculomotor root), and also the autonomic (via sympathetic nerve fibers) direct innervation of the eye. The ciliary ganglion is localized at a distance of 7 mm posterior to the eyeball below the external rectus muscle, in contact with the optic nerve. At the same time, the ciliary nerves jointly regulate the activity of the pupillary sphincter and dilator, providing special sensitivity to the cornea, iris, and ciliary body. They maintain the tone of blood vessels and regulate metabolic processes. The subtrochlear nerve is considered the last branch of the nasociliary nerve; it is involved in the sensitive innervation of the skin of the root of the nose, as well as the inner corner of the eyelids, part of the conjunctiva of the eye.
Entering the orbit, the frontal nerve splits into two branches: the supraorbital nerve and the supratrochlear nerve. These nerves provide sensitivity to the skin of the forehead and the middle zone of the upper eyelid.
The lacrimal nerve, at the entrance to the orbit, splits into two branches - upper and lower. At the same time, the upper branch is responsible for the nervous regulation of the lacrimal gland, as well as the sensitivity of the conjunctiva. At the same time, it provides innervation to the skin of the outer corner of the eye, covering the area of the upper eyelid. The inferior branch unites with the zygomaticotemporal nerve, a branch of the zygomatic nerve, and provides sensation to the skin of the cheekbone.
The second branch becomes the maxillary nerve and is divided into two main lines - the infraorbital and zygomatic. They innervate the auxiliary organs of the eye: the middle of the lower eyelid, the lower half of the lacrimal sac, the upper half of the lacrimal duct, the skin of the forehead and zygomatic region.
The last, third branch, having separated from the trigeminal nerve, does not take part in the innervation of the eye.
Optic nerves
Visual disorders such as decreased acuity, color perception, visual field impairment, and blindness cause damage to any part of the second pair of the cranial nerve - visual. The types of violations depend on the dislocation of the source.
Tubular vision manifests itself in neuritis of the second pair of cranial nerves, hysteria, glaucoma, arachnoiditis. Complete blindness - as a result of injury, pathology of the chiasm. The condition is assessed based on the results of an examination of the visual components (acuity, visual field, etc.) and the fundus.
Polychromatic tables allow you to assess the level of color perception. Visual defects (so-called scotomas) detected by an ophthalmologist signal a pathology affecting the optic nerve. Patients themselves rarely consult a doctor when the severity decreases. Amblyopia can result in amaurosis. Sometimes complete loss of vision is the result of advanced pathology, when the pathological process is irreversible.
Taste nerves
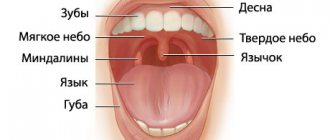
Ellipsoidal-shaped cells located in the mouth are designed to detect taste (taste bud). Taste buds consist of basal cells and chemoreceptors (the taste receptors themselves). Taste buds of different types are located on the tongue, cheeks, soft palate, epiglottis in the initial part of the esophagus.
Sensations of sweet, salty, bitter are transmitted to a certain part of the GM cortex through the nerves: glossopharyngeal (IX), facial (YII), vagus (YIII). Taste bioimpulses travel through nerve fibers to the thalamus, then to the guardian region of the GM cortex.
Damage to these nerves and the central parts of the brain (tumors, injuries, operations) provokes neural taste disorders:
- total ageusia, loss of the ability to distinguish taste (salty, sweet, etc.);
- ageusia partial;
- specific ageusia;
- dysgeusia (perverted taste).
Diagnosis of neuralgia
A neurologist is involved in differential diagnosis. Diagnosis of neuralgia begins with a neurological examination of a patient with typical complaints for this disease. The listed causes of neuralgia require a more complete examination to identify or exclude the underlying disease.
In some cases, additional instrumental examination (electroneurography) may be required if the cause of neuralgia was injury in the projection of the nerve. An MRI of the spine or any of the nerve plexuses may be required in the event of any volumetric impact on the nerve structures, as occurs with a herniated or protruded intervertebral disc or soft tissue tumors.
Diagnostics
Diagnosis is based on symptoms, medical history, and research:
- The doctor talks with the patient, finds out the symptoms. Finds out what the pain is and where it is located. Are there any infectious diseases in the head area? For example, otitis media, sinusitis, tooth extraction, adenoiditis.
- Then he examines and palpates the damaged area. The presence of swelling and redness is detected.
- When the doctor roughly presents the diagnosis, he examines for the presence of diseases with similar symptoms. That is, differential diagnosis is carried out. Refers for examination to a dentist and otolaryngologist.
- To determine the diagnosis, there is a method of applying a solution of cocaine hydroxide to the mucous membrane of the front of the nose. If the patient stops feeling pain, then this is inflammation of the nasociliary nerve.
- Next, instrumental studies should be carried out. Ophthalmoscopy, MRI of the head, biomicroscopy, anterior rhinoscopy.
- Once the diagnosis is made, treatment is prescribed.
With the help of additional examination, neuralgia of the nasociliary nerve is differentiated from other diseases. And they establish an accurate diagnosis.
Biomicroscopy of the eye
This is done using a slit lamp, the main part of which looks like a large slit. The device examines the structure of the eye, the back and front walls. This method allows you to see any damage, foreign body, and detect the disease at an early stage. Biomicroscopy allows you to see the condition of the retina and optic nerve.
Ophthalmoscopy
The fundus of the eye is examined using an ophthalmoscope. With the help of an eye mirror you can see blood vessels and nerves. Identify changes, redness, swelling.
Anterior rhinoscopy
This is done using a nasal speculum.
The anterior part of the nasal cavity is examined by inserting the device into the nostrils. The most suitable for this procedure is the Hartmann mirror. The doctor holds the device in his left hand, slightly dilating the nostril. In this case, the nasal septum and passages are visible. This is how redness, curvature, atrophy and hypertrophy are noticed. Sometimes it is possible to examine the nasal cavity using reflector lighting. It is used to examine children, as they may be frightened by an unknown object.
MRI of the head
To accurately confirm the diagnosis, an MRI of the head is performed. X-ray radiation is not used here. The examination is carried out using magnetic fields, which create an energy change in the examination area. This is how photographs are taken without the use of contrast. A cross-sectional image is displayed on the computer monitor.
Treatment of the disease
Treatment of nasociliary nerve neurosis consists of eliminating the disease that affects it.
In case of inflammatory processes in the ENT organs, patients are prescribed a course of treatment with antibiotics and a set of drugs that affect the elimination of inflammation and restoration of the mucous membrane, or surgical intervention (for pathologies of the nasal septum).
For vascular diseases, patients are prescribed drugs with antihypertensive and nootropic effects. Treatment is also carried out using vasoactive drugs.
To relieve pain and other symptomatic and clinical manifestations of neuralgia, local anesthetic drugs are used in medical practice in combination with non-narcotic painkillers and vasodilators. Their use is determined by which part of the nasociliary nerve has undergone pathological effects:
- For neuralgia of the long ciliary nerve, dicaine (0.25% eye solution) mixed with adrenaline (4 drops per 10 ml of solution) is used.
- For neuralgia of the subtrochlear region of the nasociliary nerve, cocaine hydrochloride (2% solution) mixed with 0.1% adrenaline (4 drops per 5 ml of the drug) is used. A solution of lidocaine is also used in the form of a spray, which is injected into the nasal passages on the corresponding side or both at once (for bilateral neuralgia) up to 4 times a day.
- If any part of the nerve is damaged, use a powder mixture of papaverine, glucose, antispasmodic, diphenhydramine and aminazine 2 times a day.
As an additional therapy for patients diagnosed with Charlin's syndrome, a course of intramuscular vitamin B12 is indicated, as well as intravenous administration of sulfonamide drugs.
Unpleasant chest pain is often a sign of heart disease. But a similar symptom is also characteristic of neuralgia. A competent specialist should be able to distinguish the signs of neuralgia in the heart area from heart pain. Read the article about how to treat this disease.
We will consider the causes and symptoms of trigeminal neuralgia in this topic.