Otolaryngologist for adults and children
Manevich
Igor Semenovich
Experience 27 years
Otorhinolaryngologist of the highest category, member of the European Rhinologic Society
Make an appointment
With inflammation of the laryngeal mucosa, laryngitis and concomitant diseases with sputum production often develop, so many patients wonder what it is, what are the causes, signs and symptoms of the disease, how to diagnose and how to treat to avoid complications. The occurrence of laryngitis can be triggered by viral, bacterial or fungal pathogens. The disease is of infectious origin through airborne droplets, contact, or to the fetus in the womb during pregnancy. Forms of laryngitis in adults caused by allergens or occupational activities are not contagious.
Introductory information
Laryngitis is an inflammatory process of the larynx with sputum production, which is promoted by various pathogens. Both adults and children of different age groups are susceptible to the occurrence of a pathological condition, especially children with weakened immunity and concomitant diseases. In most cases, the disease proceeds without significant complications; the process of complete recovery occurs in 7-10 days.
The acute form can develop due to respiratory infections, acute respiratory viral infections, influenza, and adenovirus infection. It can also occur as a concomitant factor in measles, diphtheria, tuberculosis and whooping cough.
Classification of pathologies of the upper respiratory tract:
- acute laryngitis manifests itself as a separate or concomitant pathology, the main signs are the primary manifestation and the effectiveness of therapy, after which after two weeks there are no consequences or complications for the body;
- the chronic form can occur due to untreated pathology and inflammation in the larynx and upper respiratory tract. It is characterized by the production of sputum. The key factors of the pathological condition are smoking, which increases the volume of sputum, and the ligaments being under constant strain.
In the absence of timely treatment of laryngitis in adults, the pathological condition turns into a chronic form and contributes to certain complications. Mostly they are associated with respiratory problems, since the larynx is an organ of the respiratory system. The main complications include:
- bronchitis;
- loss of sonority and beauty of the voice;
- false croup - mainly occurs in children. Inflammation contributes to whistling and asthma attacks;
- airway obstruction;
- mediastinitis - inflammation quickly occurs in the space between parts of the adult’s larynx, which often ends in death;
- laryngeal paresis – dangerous due to respiratory dysfunction;
- phlegmon of the neck is an acute purulent inflammation that affects the upper respiratory tract. It develops in the absence of therapeutic measures and is an indication for surgical intervention.
How does laryngitis occur in children?
In young children with laryngitis, pronounced swelling of the vocal folds and loose tissue of the subvocal space very quickly develops. This leads to a progressive narrowing of the lumen of the larynx. This condition is called acute laryngeal stenosis or false croup. Therefore, in children, the first symptom of laryngitis may be shortness of breath, accompanied by a feeling of fear and motor restlessness. Breathing may be wheezing.
The child is also bothered by a frequent dry, hysterical cough, which does not bring relief and even often worsens respiratory failure. Pallor of the skin, blueness (cyanosis) of the lips and nasolabial triangle appear. Severe respiratory failure can provoke the development of convulsive syndrome if the child previously had perinatal or later brain damage.
Symptoms and causes
In order to clearly understand the causes of laryngitis in adults and children, it is necessary to determine the pathologies that occur in the larynx and upper respiratory tract during the disease process. The muscles and cartilages of the larynx are covered by the vocal cords, which, when closed correctly, move smoothly and allow air to pass through, which contributes to the production of sound.
Laryngitis is an inflammation of the mucous membrane of the throat - the vocal cords. As a result of edema, the mechanism of ligament closure is disrupted, the lumen narrows, and the amount of sputum increases, which can lead to suffocation and other complications.
Let's look at the typical causes of laryngitis:
- allergic reactions that appear as a result of various irritants and are characterized by regularity in the presence of irritating factors;
- infectious agents;
- prolonged inhalation of frosty or hot air;
- the causes may be injuries to the throat and related organs in adults;
- a common cause is regular overstrain of the vocal cords;
- with laryngitis, further development of the pathology is facilitated by inhalation of polluted air, as a result of which sputum production increases.
The problem appears in the respiratory tract due to various external and internal factors. To determine treatment tactics and select appropriate medications to eliminate the causes of laryngitis, the doctor must identify clear causes and symptoms, and the patient’s complaints. Only competent elimination of characteristic causes and individual manifestations will allow choosing effective treatment methods for quick relief from the symptoms of pathology without complications and complete recovery.
The classic symptoms of inflammation are characterized by signs that can be easily identified not only by the doctor, but also by the patient himself, since such processes in the larynx have some distinctive characteristics. Main symptoms of laryngitis:
- disturbances in vocal activity are the primary signs of laryngitis. The vocal cords are characterized by being in an inflamed state, swollen, and the voice becomes hoarse. Painful sensations worsen when trying to speak loudly or scream;
- With laryngitis, narrowing of the larynx contributes to breathing problems. Therefore, this symptom of laryngitis with difficulty breathing often develops into false croup with severe complications;
- accompanying symptoms of laryngitis in adults are general poor health, loss of appetite, low-grade fever and chills;
- headache.
The main symptoms by which the diagnosis is made are signs from the first two categories, the rest are accompanying only to confirm the disease.
The key manifestations of the causes of laryngitis are a feeling of dryness in the throat, soreness and burning, tingling and other unpleasant sensations in the throat. Such conditions are also typical when the patient suffers from ARVI or influenza, but in this case they are more pronounced. The patient may also have a feeling of the presence of a foreign object in the larynx and pain. A common symptom of laryngitis is a dry cough, which turns into a wet cough with the release of a large amount of sputum. Basically, infectious causes of laryngitis lead to this course of the disease.
Laryngitis is characterized by low-grade fever and fatigue. The voice of patients with laryngitis may become hoarse, hoarse, or disappear completely. Depending on the causes of the pathology, at high temperatures and other signs of complications, it is necessary to take timely therapeutic measures aimed at comprehensively combating the pathological disease of the respiratory tract.
Why are vocal cords easily injured during inflammation?
There are two true vocal cords. At rest, they are at a fairly large distance from each other, forming a triangle with a wide base and coming together only in the area of the anterior ends (at the point of their connection), while the edge of each vocal cord is free.
When producing sound (and when coughing), the vocal cords come closer and touch each other. During inflammation, the edges of the vocal cords are swollen, inflamed and very easily injured during voice formation, as well as when coughing, which can not only increase their inflammation, increase the duration of the recovery process of the vocal cords, but also contribute to the chronicity of inflammation and provoke the appearance of benign neoplasms along the edge of the vocal cords , coarsening of the edges of the vocal cords and, as a result, a change, deepening of the voice. Therefore, it is so important to remain silent during their inflammation, maintaining a safe distance between the vocal cords, avoiding their traumatization.
Diagnosis of the disease: how it goes, what procedures are performed
To diagnose pathology of the upper respiratory tract, it is necessary to examine the throat by a qualified otolaryngologist, who takes an anamnesis, prescribes tests, laryngoscopy or a biopsy of the affected area of the larynx.
The pathology is diagnosed during the initial examination, then to confirm the diagnosis it is necessary to take laboratory and biochemical blood tests, and you can also do an ultrasound scan to see the presence of sputum in the larynx and upper respiratory tract. When taking blood, a bright red hue of the blood indicates insufficient coagulation and the occurrence of inflammatory processes in the body. Often, in the presence of inflammation, the pathological condition is diagnosed using a biopsy in order to select appropriate antibiotics.
If there is difficulty breathing or pain in the upper respiratory tract, the patient should be immediately checked by a qualified doctor. In the presence of minor symptoms and manifestations on the laryngeal mucosa, patients often confuse the pathology with ordinary shortness of breath or a cold. In such conditions, carrying out routine diagnostics and examination is very difficult; it is necessary to check the current state of the larynx using a modern method - laryngoscopy.
This diagnostic method is carried out using a laryngoscope and allows the doctor to deeply examine the larynx by viewing through a backlit mirror. This diagnostic method is used to identify swelling of the throat mucosa and the location of blood vessels. Basically, in adults with laryngitis, the following signs are revealed: overflow of blood vessels, and overflow of the throat mucosa with sputum, bilateral pathology in advanced cases. Laryngoscopy allows the doctor to make an unambiguous diagnosis; this condition can be cured with properly selected medications.
To determine the severity of the disease with laryngitis, examinations are prescribed using radiography or computed tomography of the larynx, endofibrolaryngotracheoscopic method. These methods are not basic and are prescribed only if there are prerequisites and indications. In some situations, differential diagnosis is necessary to exclude oncology of the upper respiratory tract and laryngeal tuberculosis.
What types of laryngitis are there?
Currently, doctors use several classifications of laryngitis simultaneously, which makes the diagnosis as detailed and informative as possible.
- By type of course: acute (lasting up to 3 weeks) and chronic laryngitis.
- According to the prevalence of the inflammatory process: limited (with damage to certain areas of the larynx) and widespread (diffuse);
- According to the nature of changes in the mucous membrane: catarrhal, atrophic, hypertrophic (or hyperplastic), the last 2 forms are characteristic only of the chronic process;
- By etiology: infectious (viral, bacterial, fungal) and non-infectious.
Doctors treating the disease
Many patients wonder which doctor treats the larynx, respiratory diseases in children and adults, and identifies the causative agent of the pathological condition. If you have a painful sensation in the throat or diseases of the upper respiratory tract, you should contact an otolaryngologist rather than a general practitioner.
A doctor who is directly involved in the diagnosis and treatment of laryngitis in adults is an otolaryngologist. To diagnose the main signs and make a diagnosis, you must contact a qualified ENT specialist in a clinic or private clinic. Experienced doctors with high qualifications and significant work experience at JSC “Medicine” (clinic of Academician Roitberg) are engaged in diagnostic procedures and treatment for adults and children of different ages. An experienced doctor treats the disease on an outpatient basis using effective medications, and in case of significant complications, prescribes hospitalization.
Treatment methods
Modern methods of treating laryngitis depend on the symptoms, causes and indications; they are selected only after a thorough diagnosis and determination of the causative agent of the laryngeal disease. Since the course of the pathology occurs in different ways, the forms differ in course and symptoms, laryngitis in adults in each form has different treatment. Therefore, we will consider the key principles of treatment, as well as what method is recommended to treat the disease in one form or another. Therapy is mainly carried out on an outpatient basis; in case of a complex and advanced form of the disease, the patient undergoes procedures in the hospital.
Acute therapy
Treatment of laryngitis for adults is prescribed medicinal and non-medicinal, depending on the characteristics of the disease, causes, symptoms and special indications.
Non-drug therapies:
- if possible, completely limit vocal activity to allow the cords to return to normal. You can’t not only shout or speak loudly, but also talk in a whisper. In most cases, such a ban lasts up to two weeks. If the voice is a direct part of professional activity, after getting rid of the disease, it is necessary to visit a phoniatrist for periodic examinations within 2-3 months;
- phonopedia – measures aimed at activating and normalizing the vocal cords;
- physiotherapy - microwaves, phonophoresis and electrophoresis.
Drug treatment of acute laryngitis in adults involves the use of a complex of medications prescribed after the causative agent has been identified and an accurate diagnosis has been made. Features of treating laryngitis with medications:
- Antibiotic therapy is necessary in the presence of inflammatory processes in the throat, purulent exudation, and high fever. Also, antibiotics are used if there is no response from anti-inflammatory drugs within 4-5 days, and if the disease has spread to the lower respiratory tract, there is green sputum. An antibiotic is prescribed depending on the causative agent of the pathology in an adult after conducting appropriate blood tests and sputum from the throat;
- antihistamines to eliminate the causes of sore throat. This group of drugs is aimed at relieving swelling of the larynx;
- antifungal agents are used for fungal pathogens in adults; they help cure the disease with complex therapy;
- If there is green sputum or a strong cough, expectorants and antitussives are prescribed to remove phlegm from the throat. They also relieve irritation of the mucous membrane. You can use mucolytics in the form of inhalations for adults, so they penetrate deep into the throat into the foci of inflammatory processes and act most effectively. Such inhalations in combination with other medications allow you to quickly and effectively remove green phlegm.
croup
“Croup”, “acute or recurrent laryngitis/laryngotracheitis”, “acute airway obstruction”, “larynx stenosis” - are the names listed above synonymous or are they independent nosological forms? Every practicing physician should have a clear understanding of what the listed terms mean.
Probably the most widely used term, especially in pediatric practice, is “croup,” and the most general term can be considered “acute airway obstruction,” but in ICD-10 the codes are given according to the “organ principle.”
So, croup (from the Scottish croup - to croak) is an infectious disease syndrome that always implies the presence of acute stenosing laryngitis (or laryngotracheitis, or less commonly laryngotracheobronchitis), accompanied by hoarseness, a “barking” cough and shortness of breath, often of an inspiratory nature. That is, croup is understood as the presence of a certain syndrome with a triad of clinical symptoms: stridor—barking cough—hoarseness. The syndrome is formed in diseases manifested by the development of an acute inflammatory process in the mucous membrane of the larynx and trachea. Therefore, the term “croup” is applicable only to infectious diseases! Domestic pediatricians traditionally divide croup into “true” and “false”, depending on the level of damage to the larynx, although this division is extremely arbitrary, since the mucous membrane of the larynx along its entire length, as well as the mucous membrane of the underlying parts of the respiratory tract, is often involved in the process. “True” croup develops as a result of damage to the true vocal cords (folds). The only example of “true” croup is diphtheria croup, which occurs with the formation of specific fibrinous changes on the mucous membrane of the vocal cords. “False” croup includes all stenotic laryngitis of a non-diphtheria nature, in which the inflammatory process is localized mainly on the mucous membrane of the subglottic (subglottic) zone of the larynx. “Acute laryngitis” is coded J04.0 in ICD-10, “acute laryngotracheitis” is J04.2, “acute obstructive laryngitis” is J05, and “chronic laryngitis” and “chronic laryngotracheitis” are J37.0 and J37.1, respectively. . In any case, it should be understood that acute obstruction of the upper respiratory tract (narrowing of the lumen of the larynx with breathing disorders and the development of acute respiratory failure) is primarily an emergency condition that requires emergency diagnosis and treatment at the prehospital stage.
This condition most often occurs in children of early and preschool age (from 6 months to 3 years, and in 34% of cases - in children of the first 2 years). Acute obstruction is associated with the anatomical and physiological characteristics of the respiratory tract in young children: the narrowness of the lumen of the trachea and bronchi (funnel-shaped instead of cylindrical), the tendency of their mucous membrane and the loose fibrous connective tissue located underneath to develop edema, the peculiarities of the innervation of the larynx, which are associated with the occurrence of laryngospasm, and relative weakness of the respiratory muscles. Swelling of the mucous membrane with an increase in its thickness by only 1 mm reduces the lumen of the larynx by half! The development of acute obstruction of the upper respiratory tract in adults is a fairly rare phenomenon and is usually associated with diphtheria.
There are infectious and non-infectious causes of acute obstruction of the upper respiratory tract. Infectious causes include viral infections (caused in 75% of cases by influenza and parainfluenza viruses of type I, as well as rhinosyncytial viruses, adenoviruses, less commonly measles and herpes viruses) and bacterial infections (with the development of epiglottitis, retropharyngeal and peritonsillar abscess, diphtheria). In this case, the mechanism and routes of transmission of the pathogen are determined by the epidemiological features of the main infectious disease. Aspiration of foreign bodies, laryngeal injuries, allergic edema, laryngospasm can be non-infectious causes of the development of acute obstruction of the upper respiratory tract.
In the genesis of airway obstruction, three factors play a certain role: edema, reflex spasm of the laryngeal muscles and mechanical blockage of its lumen with inflammatory secretion (mucus) or a foreign body (including food, vomit, etc.). Depending on the etiology, the significance of these components may vary. In practical work, in order to conduct adequate therapy and provide effective assistance to a child, it is important to be able to quickly differentiate them.
The main reason for the development of croup is an inflammatory process in the area of the subglottic space and vocal cords (acute stenotic laryngotracheitis). The phenomenon of narrowing of the lumen of the upper respiratory tract during croup is formed sequentially, in stages, and is directly related to the reaction of the laryngeal tissue to an infectious agent, including one that triggers an allergic reaction. When assessing the clinical picture, it is necessary to take into account the prevalence of edema of the inflamed mucous membrane, spasm of the muscles of the larynx and trachea and hypersecretion of mucus, since this is fundamental when choosing treatment tactics.
Breathing disorders due to narrowing of the lumen of the larynx most often occur at night, during sleep, due to changes in the conditions of lymph and blood circulation of the larynx, a decrease in the activity of the drainage mechanisms of the respiratory tract, the frequency and depth of respiratory movements.
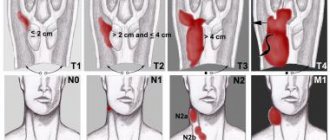
The clinical picture of acute stenosis of the upper respiratory tract is determined by the degree of narrowing of the larynx, associated disturbances in respiratory mechanics and the development of acute respiratory failure.
With incomplete obstruction of the larynx, noisy breathing occurs - stridor, caused by intense turbulent passage of air through the narrowed airways. With dynamic narrowing of the airway lumen, normally silent breathing becomes noisy (due to vibrations of the epiglottis, arytenoid cartilages, and partly the vocal cords). When swelling of the laryngeal tissues dominates, a whistling sound is observed; when hypersecretion increases, hoarse, bubbling, noisy breathing is observed; with a pronounced spastic component, the sound characteristics are unstable. It should be remembered that as stenosis increases due to a decrease in tidal volume, breathing becomes less and less noisy!
Inspiratory stridor usually occurs when there is narrowing (stenosis) of the larynx at or above the vocal cords and is characterized by noisy inspiration with retraction of the chest wall. Stenoses below the level of the true vocal cords are characterized by expiratory stridor with the participation of auxiliary and reserve respiratory muscles in breathing. Laryngeal stenosis in the subglottic space usually manifests as mixed inspiratory and expiratory stridor. The absence of voice changes indicates the localization of the pathological process above or below the vocal cords. The involvement of the latter in the process is accompanied by hoarseness or aphonia. A hoarse, “barking” cough is typical of subglottic laryngitis. Other signs of upper respiratory tract obstruction are nonspecific: anxiety, tachycardia, tachypnea, cyanosis, neurovegetative disorders, etc. Rapid breathing and elevated body temperature during croup can lead to significant fluid loss and the development of respiratory exicosis.
Based on the severity of narrowing of the lumen of the larynx, four degrees of stenosis are distinguished, which have significant differences in the clinical picture (see table). However, when making a diagnosis, the severity of the croup is determined primarily, and not the severity of the stenosis (the assessment of the latter is possible with direct laryngoscopy, which is impossible at the prehospital stage). In a comprehensive assessment of the patient’s condition, factors such as the participation of auxiliary muscles in the act of breathing (evidence of a significant narrowing of the airway lumen), symptoms of respiratory and cardiovascular failure, depression of consciousness and persistent hyperthermia should be taken into account.
Thus, the classification of croup is built taking into account:
- etiology of croup (viral or bacterial);
- stages of laryngeal stenosis (compensated, subcompensated, decompensated, terminal);
- nature of the course (uncomplicated or complicated - the appearance of a mixed infection due to the addition of a secondary bacterial purulent infection to the main process).
- with the development of diphtheria croup, the nature of the spread of the inflammatory process is also taken into account (spread to the mucous membrane of the trachea, bronchi and bronchioles is possible - the so-called descending croup).
- recurrence of the syndrome.
DIFFERENTIAL DIAGNOSIS
Diphtheria of the larynx
Diphtheria of the larynx is most often combined with manifestations of this infection in another location (diphtheria of the pharynx or nose), which greatly facilitates diagnosis. The main differences between diphtheria of the larynx and croup that developed against the background of acute respiratory viral infection are the gradual onset and severity of the course with increasing symptoms. The voice with diphtheria of the larynx is persistently hoarse with the gradual development of aphonia. In the treatment of diphtheria of the larynx, along with measures aimed at restoring airway patency, it is necessary to urgently administer anti-diphtheria serum to the child using the Bezredko method in a dose of 40-80 thousand IU per course of treatment, depending on the form of the disease.
Allergic swelling of the larynx
Allergic laryngeal edema is not always possible to distinguish from croup of an infectious nature only by clinical signs. Allergic laryngeal edema develops under the influence of any antigen of inhalation, food or other origin. There are no specific guidelines for ARVI. Fever and intoxication are not typical. These children have a history of various allergic sympathies: skin manifestations of allergies, food allergies, Quincke's edema, urticaria, etc. During therapy with inhaled glucocorticoids with the addition of b2-adrenomimetics (salbutamol - Ventolin), anticholinergics (ipratropium bromide - Atrovent ), combined drugs (a combination of fenoterol and ipratropium bromide - berodual), and also, according to indications, antihistamines, rapid positive dynamics of stenosis occurs.
Laryngospasm
Laryngospasm occurs mainly in children of the first 2 years of life against the background of increased neuromuscular excitability, with manifestations of current rickets with a tendency to tetany. Clinically, spasm of the larynx manifests itself unexpectedly; the child experiences difficulty breathing with a characteristic sound in the form of a “cock crow”, while fear, anxiety, and cyanosis are noted. Mild attacks of laryngospasm are relieved by spraying the child’s face and body with cold water. You should try to induce a gag reflex by pressing on the root of the tongue with a spatula or spoon, or provoke sneezing by irritating the mucous membrane of the nasal passages with a cotton swab. If there is no effect, diazepam should be administered intramuscularly.
Epiglottitis
Epiglottitis is an inflammation of the epiglottis and adjacent areas of the larynx and pharynx, most often caused by Haemophilus influenzae type b. The clinical picture is characterized by high fever, sore throat, dysphagia, muffled voice, stridor and respiratory failure of varying severity. Palpation of the larynx is painful. When examining the pharynx, a dark cherry color of the root of the tongue, its infiltration, swelling of the epiglottis and arytenoid cartilages that close the entrance to the larynx are revealed. The disease progresses rapidly and can lead to complete closure of the lumen of the larynx.
At the prehospital stage, it is optimal to inject a third-generation cephalosporin antibiotic (ceftriaxone) as early as possible. Transport of the child to the hospital is carried out only in a sitting position. You should avoid taking sedatives. You need to be prepared for tracheal intubation or tracheotomy.
Retropharyngeal abscess
Most often, retropharyngeal abscess occurs in children under three years of age. It usually develops against the background of or after an acute respiratory viral infection. The clinical picture is dominated by symptoms of intoxication, severe fever, sore throat, dysphagia, stridor, and drooling. There is no barking, rough cough or hoarseness. Coughing is difficult due to severe pain in the throat. The child often takes a forced position - with his head thrown back. Examination of the pharynx presents significant difficulties due to the child’s severe anxiety and inability to open his mouth. Sedation is used for examination.
Treatment is not carried out at the prehospital stage. Urgent hospitalization to the surgical department is required. In the hospital, the abscess is opened and drained while receiving antibiotic therapy.
Foreign bodies
Foreign bodies of the larynx and trachea are the most common cause of asphyxia in children. Unlike croup, aspiration occurs unexpectedly in the context of apparent health, usually while the child is eating or playing. A coughing attack appears, accompanied by suffocation. The clinical picture depends on the level of airway obstruction. The closer to the larynx the foreign body is located, the greater the likelihood of asphyxia. This location of the foreign body is usually accompanied by the appearance of laryngospasm. The child is scared and restless. During auscultation, you can sometimes hear a popping sound, indicating the release of a foreign body.
After examining the oral cavity and entering the larynx, attempts are made to remove the foreign body by mechanically “knocking out” it. A child under 1 year of age is placed face down with the head end down 60°. With the edge of the palm they give him short blows between the shoulder blades. In children older than one year, sharp pressure with the hand on the abdomen from the midline inward and upward (at an angle of 45°) can be effective. In older children, blows to the back are alternated with sharp compression of the abdomen, clasping the child with the arms from behind (Heimlich maneuver).
If attempts to remove a foreign body using mechanical techniques are ineffective, the issue of urgent intubation or tracheotomy should be addressed.
Treatment of croup
Treatment of croup should be aimed at restoring the patency of the larynx: reducing or eliminating spasm and swelling of the laryngeal mucosa, freeing the lumen of the larynx from pathological secretions.
- Patients are subject to hospitalization in a specialized or infectious diseases hospital if it has an intensive care unit, but treatment should begin at the pre-hospital stage.
- The child should not be left alone; he must be calmed down and picked up, since forced breathing during anxiety or crying increases the symptoms of stenosis and the feeling of fear.
- The room temperature should not exceed 18°C. Effective coughing up of sputum is also facilitated by the creation of an atmosphere of high humidity in the room where the child is located (the “tropical atmosphere” effect), steam inhalation (isotonic NaCl solution through a nebulizer). A warm drink is indicated (hot milk with soda or Borjomi).
- Etiotropic therapy is effective for diphtheria croup - administration of anti-diphtheria serum IM or IV.
- Antibiotics - for diphtheria croup and croup complicated by secondary bacterial infection.
- Expectorant and mucolytic drugs administered primarily by inhalation, for example ambroxol (lazolvan), etc., contribute to the dilution and removal of mucus from the respiratory tract.
- Considering the significant participation of the allergic component in the development of croup, it is advisable to include antihistamines (for example, chloropyramine (suprastin), etc.) in the complex of therapeutic measures. Randomized double placebo-controlled study Gwaltney JM et al. [3] showed that in the treatment of acute respiratory diseases, a combination of antipyretic, antihistamine and antiviral drugs can effectively (33-73% compared with placebo) reduce the severity of various clinical manifestations of the disease, including the amount of mucus produced and pain in the pharynx and larynx . In another work, the same authors [2] demonstrated that clemastine, prescribed in the complex treatment of ARI, in contrast to pheniramine, only increases the sensation of dryness and soreness in the throat. And Gaffey MJ et al. [1] noted no effect from the use of terfenadine in a similar clinical situation.
- Glucocorticoids, for example prednisolone at a dose of 3-10 mg/kg - to relieve swelling of the laryngeal mucosa.
- Psychosedatives - with severe spasm of the laryngeal muscles. For routine treatment of spastic symptoms, tranquilizers are used.
- Intubation and tracheostomy are indicated when conservative therapy is ineffective and during resuscitation measures (asphyxia, clinical death).
So, until recently, therapy for croup was limited mainly to the supply of humidified air and the administration of systemic steroids. However, given the fact that croup most often develops in infants and young children, in whom both oral and injected steroids pose a serious problem, and also that the entire medical community is currently striving to reduce the possible risk of side effects of systemic steroid therapy, the use of inhaled glucocorticoids seems especially promising. To date, vast experience has been accumulated in the treatment of stenosing laryngitis/laryngotracheitis with inhaled budesonide (Pulmicort) through a nebulizer. The effectiveness of this type of therapy was, in particular, discussed by Ausejo et al. a meta-analysis of 24 (!) randomized controlled trials, which also compared the effectiveness of inhaled budesonide and systemic dexamethasone. It was shown that the use of budesonide through a nebulizer for croup compared with dexamethasone by injection significantly reduced the number of cases when the use of adrenaline was considered necessary (by 9%), and also influenced the duration of emergency care both at the prehospital and in-hospital stages . Nebulized administration of budesonide was effective in children with both mild-moderate and moderate-severe croup. Moreover, inhaled single doses (2 or 4 mg) of budesonide were significantly more effective than placebo and were comparable in effectiveness to dexamethasone (0.6 mg/kg). They invariably led to the leveling of lobar symptoms and a decrease in the duration of hospital treatment.
In order to reduce swelling of the mucous membrane of the larynx, which often spreads to the trachea and bronchi, and relieve spasm, b-adrenomimetics can be used simultaneously with budesonide (salbutamol - Salgim, Ventolin, anticholinergics - ipratropium bromide (Atrovent), a combination of b-adrenergic agonists and anticholinergics - berodual).
It should be noted that acute stenosing laryngotracheitis occupies a significant place in the structure of emergency medical calls to children. So, in Moscow last year, parents contacted the ambulance about 198 thousand times. And if we discard cases of acute respiratory infections and influenza (approximately 70 thousand), acute surgical pathology and trauma (58 thousand) and a group of intestinal infections (12 thousand), then of the remaining calls, every ninth or tenth was precisely about the child’s difficulty breathing ( attack of bronchial croup). Moreover, if the frequency of calls for exacerbation of asthma has decreased over the past 3 years, then for croup, on the contrary, it has increased (by about 1000 cases).
In our department of hospital-replacement technologies of the Scientific Center for Children's Health of the Russian Academy of Medical Sciences, where emergency care for children is also provided, over the past 2.5 years (since September 2000), acute stenosing laryngotracheitis has been treated for 100 children (67 boys and 33 girls) aged 6 months up to 7 years. Acute obstruction of the upper respiratory tract developed in 32 children against the background of ARVI, in 5 - during contact with a causally significant allergen, in 8 - against the background of ARVI and physical activity, in 1 - against the background of physical activity and contact with an allergen, in 54 - without visible provoking factors, including ARVI. The parents of all children came to our department, considering this alternative option for emergency care as more effective. All children received inhalations through a nebulizer (two or three times) of budesonide (Pulmicort) at a dose of 1000 mcg, ipratropium bromide (Atroventa) at a dose of 20 drops or the combined drug Berodual at a dose for children under 6 years old - 10 drops, for children over 6 years old - 20 drops drops), mucolytic drug lazolvan (in a dose of 20 drops in an isotonic NaCl solution.
The effectiveness of the first inhalation of budesonide was noted in 53% of children (within 15-25 minutes after inhalation, breathing calmed down, shortness of breath, painful non-productive “barking” cough disappeared, and anxiety decreased). 44 children needed 2–3-day courses of inhalation therapy, and only in 3 patients the effect was achieved on the 4–5th day. Thus, budesonide, administered in inhalation through a nebulizer, can be considered a highly effective drug for emergency treatment of acute upper respiratory tract obstruction in children of any age, including at the prehospital stage.
L. S. Namazova, Doctor of Medical Sciences N. I. Voznesenskaya A. L. Vertkin, Doctor of Medical Sciences, Professor of the Scientific Center for Children of the Russian Academy of Medical Sciences, MGMSU, NNPOSMP, Moscow
Literature
- Gaffey MG, Kaiser DL, Hayden FG Ineffectiveness of oral terfenadine in natural colds: evidence against histamine as a mediator of common cold symptoms // Pediatr. Infect. Dis. J. 1988. V. 7(3) Mar. P. 223-228.
- Gwaltney JM Jr., Park J., Paul RA et al. Randomized controlled trial of clemastine fumarate for treatment of experimental rhinovirus colds.
- Gwaltney JM Jr., Winther B., Patrie JT, Hendley JO Combined antiviral-antimediator reatment for the common cold // J. Infect. Dis. 2002. V. 186(2). Jul 15. P. 147-154.
Therapy for chronic form
Features of treatment methods for adults in chronic form are the following goals:
- complete relief from the inflammatory process that is present in the throat;
- voice restoration;
- preventing the disease from flowing into the formation of malignant tumors in the throat.
During periods of exacerbation, antibiotic therapy is prescribed with drugs that are used in the acute form. Antibacterial medications are used for severe inflammation and purulent exudation. This method of treatment is also used if surgical intervention is required to treat laryngitis in adults after the examination.
Antibiotics are prescribed exclusively by the attending physician, based on the symptoms, causes, indications and specific course of the disease. In the chronic form, such therapy is required to relieve the signs and symptoms of the pathological condition. To cope with the disease and reduce the frequency of exacerbations, the patient needs to lead a healthy lifestyle, get rid of bad habits that irritate the mucous membranes, respiratory tract, and throat.
What not to do
There are several common mistakes, by making which the patient puts his health at risk. Doctors categorically prohibit the following in case of illness:
- warming up the throat - the procedure is extremely dangerous, as it can contribute to the rapid spread of the inflammatory process, which is why there is a high probability of developing an abscess, phlegmon and sepsis;
- rubbing the throat area with vinegar or preparations containing alcohol is similar to warming;
- smoking during therapy - nicotine leads to serious damage to the mucous membrane, because of which, if you do not stop smoking, at least for the duration of the illness, treatment will be useless;
- the use of oil to treat the mucous membrane - by forming a film on its surface, oils only aggravate the condition, creating a favorable environment for pathogens;
- the use of alcohol infusions for gargling, since alcohol is a strong irritant to the throat, which will only further injure the mucous membrane;
- non-compliance with diet during treatment;
- self-medication.
Any violations in the treatment of the disease can lead to severe complications. If the patient does not comply with medical recommendations, then the specialist involved in treatment cannot guarantee a positive result.
Indications for treatment in the clinic and surgical intervention
In general, treatment methods in a hospital setting are used infrequently; patients are sent to the clinic only in the presence of an advanced condition and complications that threaten the patient’s life and require immediate intervention. Conditions that contribute to treatment in the clinic:
- severe swelling of the throat mucosa;
- extensive inflammatory processes, suppuration in the throat, epiglottis;
- potential for the development of stenosis.
These pathological conditions can provoke respiratory dysfunction and lead to life-threatening consequences. Therefore, laryngitis must be treated in a hospital under the close supervision of a doctor.
Indications for surgical treatment of laryngitis in adults:
- diagnosis of abscess laryngitis;
- development of purulent inflammation in the throat;
- narrowing of the throat and inability to breathe normally;
- lack of results from treatment with various groups of medications.
In all of these situations, it is necessary to perform surgery and apply modern laparoscopic treatment methods in order to save the patient’s life and prevent the occurrence of malignant tumors.
Indications
In case of laryngitis, to cope with the disease, you must follow the following recommendations:
- general hardening of the body in order to increase immunity;
- quitting smoking and drinking alcohol;
- a healthy lifestyle, proper nutrition and a balanced diet so that the body receives all the vital vitamins and microelements;
- regular exercise will be an excellent preventive measure, as it allows you to train the respiratory system;
- in the winter, when various diseases worsen, it is necessary, if possible, to avoid crowded places, since the reason that contributes to laryngitis is an increased tendency to contract viral diseases, influenza;
- carry out timely treatment of the throat, eliminate the causes and symptoms of diseases, and undergo regular examinations by doctors.
By following these recommendations, you can avoid the development of laryngitis and other pathologies, since the body will independently reject pathogenic bacteria and infections.
Contraindications
Let's consider the main contraindications for laryngitis:
- Smoking - this bad habit contributes to irritation in the throat, constant soreness and the flow of a dry cough into a wet one with sputum production. Laryngitis in acute and chronic form requires complete cessation of smoking, and this includes active and passive smoking;
- avoiding alcoholic beverages, which also irritate the mucous membranes. If you have laryngitis, you must avoid all alcoholic beverages. In particular, when treating laryngitis, you should not drink alcohol in parallel with taking antibiotics and other medications;
- sedentary lifestyle and lack of training of the respiratory system, constant presence in rooms with polluted air. These factors must be avoided to prevent the development of laryngitis.
Cost of initial appointment, research, treatment
JSC "Medicine" (clinic of Academician Roitberg) employs highly qualified doctors who can make an accurate diagnosis and carry out effective treatment of laryngitis using modern methods and drugs, regardless of the stage and course. The price of an initial appointment with an otolaryngologist in the clinic for laryngitis is indicated in the table below; administrators can provide more detailed pricing information by phone or in the clinic when making an appointment with a doctor.
Detailed prices for treatment and examination are indicated in the price list posted on the website of our clinic. The cost of treatment depends on the stage, characteristics of laryngitis, the presence of concomitant diseases and complications. In the presence of fever and green sputum, we are talking about an advanced or chronic stage of the pathology, so in some cases treatment in a hospital clinic may be required. Basically, for laryngitis, the doctor prescribes drug treatment, after which it is necessary to return for a second appointment to be examined by a doctor, take tests again and confirm recovery.
Why does acute laryngitis deserve special attention?
Acute laryngitis is a disease that cannot be ignored, hoping for “maybe”, especially since it is impossible to continue working during inflammation of the vocal cords, especially for people in “voice specialties” (actors, announcers, journalists, teachers, doctors, etc.) We must remember that the vocal apparatus must be treated very carefully, since a person is very social, and the main means of communication is the voice. Be sure to contact an ENT doctor to examine the vocal cords, prescribe treatment and issue a certificate of incapacity for work.
Advantages of treatment at the clinic of JSC "Medicine"
The modern clinic of JSC "Medicine" in Moscow is a multidisciplinary medical institution with a hospital and modern equipment for the diagnosis and treatment of various diseases. Patients can have no doubt in the clinic’s doctors, since they all have the appropriate certificates, many have undergone training and internship abroad, and therefore use modern technologies and effective methods of treating laryngitis and other pathological conditions in treating patients.
An undoubted advantage of the clinic is cooperation with insurance companies, which makes the process of treating laryngitis less expensive. When staying in a hospital, patients are provided with comfortable rooms with all amenities.
By contacting our multidisciplinary medical center, each patient receives an individual consultation with a doctor, high-quality treatment, and the appointment of an effective laryngitis treatment regimen. Doctors are focused on effective treatment, so they prescribe effective modern medications and procedures to quickly restore voice activity and relieve the patient of fever, sputum production due to laryngitis, and other painful sensations.