Fibrin is an essential protein. Properties, functions, fibrin and inflammation
Contents
hide
1 Fibrin is an essential protein. Properties, functions, fibrin and inflammation
2 The role of fibrin in inflammation
3 Body protection
4 Function of fibrin
5 Experiments performed
6 Enzyme treatment
7 Method of treating patients with trophic ulcers
8 Classification of wounds. Wound process 8.1 Materials used in the article:
Fibrin is a protein that is the end result of blood clotting. It is formed as a result of the effect of thrombin on fibrogen.
Fibrin is an insoluble protein produced in the body in response to bleeding. This protein is a solid element consisting of fibrous threads. The progenitor of fibrin is fibrinogen. This is a protein produced by the liver. It is in the blood. When tissue is damaged, bleeding occurs. To stop it, thrombin begins to work. It affects fibrinogen, thereby provoking its transformation into fibrin.
First, the protein molecules combine into long strands that entangle the platelet, creating a rough mass. Gradually it hardens and contracts, forming a bloody clot. The compaction process is stabilized by a fibrin-stabilizing factor.
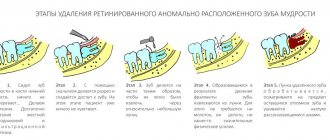
Why do complications occur after tooth extraction?
The most common reason for the development of complications is the patient’s failure to comply with medical prescriptions. Normally, the hole should heal within a few days. She shouldn't be sick for a long time. As a result of the fact that the blood clot closes it, it is reliably protected from viruses and food debris.
It happens that a person actively rinses the wound or constantly touches it with his tongue, fingers, and tries to remove the light coating. Then the clot displaces or does not form completely, the tissue becomes infected and alveolitis develops.
Untreated neighboring teeth can also lead to disease (which is why all carious “cavities” need to be treated before removal), and failure to comply with the rules of oral hygiene. If you properly prepare for extraction and follow all the doctor’s instructions, the risk of developing alveolitis after removal will be minimal.
The role of fibrin in inflammation
Fibrin production and inflammation are two closely related processes. Protein plays an important role in contact with deteriorating, damaged tissue. Thrombokinase released from the tissue comes into contact with fibrinogen.
When blood clots, all toxic substances become clogged in the clot. This feature of the effect of protein during the inflammatory process protects the body from the further spread of toxins and their negative effects. This reaction is called fixation. Thus, fibrin is also a protector of the body from toxins.
Deviation from the norm
The following symptoms indicate that an infection is developing:
- aching or throbbing pain that appears spontaneously;
- swelling near fibrinous plaque;
- redness next to the damage at a distance of one to two cm;
- increase in body temperature – more than 37 degrees.
This indicates that the process has begun to spread throughout the body. The clinical picture of fibrinous plaque on a wound may be supplemented by general disorders, for example, weakness or nausea, and the appearance of dizziness.
With aggravated purulent infection, the human body will react to changes very hard. Immediately after the appearance of swelling, phlegmon reactions only intensify. The most striking symptom is a feverish state. It is associated with deterioration of the patient's condition and increasing pain.
In addition, during diagnosis, changes in the structure of the blood may be noted. For example, increasing the leukocyte ratio or protein production. It is better to save photographs of tests and copies of data for further examinations for fibrinous plaque.
Body protection
The formation of insoluble fibrin helps protect the body from blood loss, as well as from inflammatory processes. However, such a reaction causes pain and swelling, tissue damage, and disruption of their functionality. This is subsequently eliminated by reparative processes. At their early stage, special substances are produced that cause fibrin depolymerization. Such a reaction, even at the very beginning of the inflammatory process, can inhibit the effect of protein on the pathological focus.
When white plaque is a harbinger of disease
It also happens that a whitish coating indicates the development of alveolitis after tooth extraction. This means that the tooth socket has become infected. In this condition, the patient is concerned about:
- severe pain in the area of the removed unit;
- increased body temperature;
- weakness, decreased performance;
- enlargement of the submandibular lymph nodes;
- headache;
- unpleasant putrid odor from the mouth and the same taste in the mouth.
If you experience these symptoms, you should make an appointment at the dental clinic as soon as possible.
Experiments performed
Scientists conducted experiments on animals, during which it turned out that proteases introduced from outside before the inflammatory process can prevent its development completely, and in some cases the pathology was mild. Experience has shown that the use of tryptic substances in most cases stops the development of inflammatory processes at the onset of the disease.
When prophylactic doses of enzymes were administered, protein formation decreased.
Fibrin is not just a protein, but the creator of a protective barrier around the pathological focus, which protects against disease. Subsequently, this insoluble component serves to build connective tissue. It also participates in regeneration processes. The formation of scar tissue depends on the duration of storage and the amount of fibrin produced by the body.
So what is fibrin and what is it for? This substance is produced by the body's cells in such an amount that is necessary to quickly stop bleeding and which will help quickly restore damaged tissue. In some cases, fibrin is a pest. If it is produced and deposited in large quantities, the protein can cause harm to the body. As far as is known, fibrinolysis is a long process that is not able to dissolve all excess protein. Moreover, this process requires certain conditions.
To get rid of excess fibrin, special enzyme treatment is prescribed.
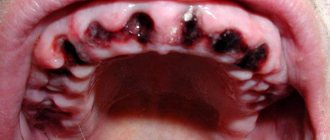
How and where can you see “ready” fibrin?
Fibrin can be seen on a wound that was initially purulent, drained and began to heal by secondary intention. After some time, during the healing process, a white coating forms along the edges of the wound - this is fibrin, which protects the site of the lesion and forms future tissue. However, on a wound in which the bleeding has just stopped, fibrin, although present, is unlikely to be detected with the naked eye.
Fibrin can be seen in an ulcer formed on the skin or mucous membranes (for example, in a duodenal ulcer during endoscopic examination), and the presence of this substance at the bottom of the ulcer indicates that it has already begun to prepare for healing (stage 2 - remission stage inflammatory process).
The presence of fibrin in a smear from the urogenital tract (both men and women), viewed under a microscope, may indicate that an inflammatory process is taking place in this area. However, this is an indirect sign. And in order to establish (or suspect?) a diagnosis, a complete description of the biocenosis present in the smear is necessary, that is, fibrin in such cases does not seem to be an independent object of study and means little for diagnosis.
Fibrin threads can also be observed in blood taken without a preservative solution. As the blood coagulates, it forms a clot, releasing serum. In plasma (blood taken with a preservative), fibrinogen is preserved, which is how it differs from serum, so plasma does not lose the ability to form fibrin filaments, which is achieved by adding calcium chloride to this biological medium. These methods are used to prepare hemagglutinating sera that determine human blood groups.
Enzyme treatment
Recently, special attention has been paid to the properties of enzymes. This is especially true for proteases. To treat fibrin enzymes, substances of this type are used. They help dissolve excess protein, thereby preventing serious complications such as blood clots.
The properties of proteolytic enzymes are different. They are able to have fibrinolytic and immunomodulatory effects on the body, as well as improve blood circulation and work as decongestants and anti-inflammatory substances.
Since thrombus formation is based on the production of fibrin, a protease is needed that causes the breakdown of this substance. Without such an enzyme, it is impossible to break the protein into molecules, therefore, there will be no improvement in blood microcirculation.
With local exposure to protease, it is possible to remove necrotic plaque, resolve fibrinous formation, and liquefy viscous secretions.
Content:
- When white plaque is the norm
- When white plaque is a harbinger of disease
- Why do complications occur after tooth extraction?
- How to recognize the problem
- Diagnostic measures
- Treatment of alveolitis
After tooth extraction, it is important to monitor the condition of the mucous membrane.
Very often a white coating appears in the extraction area. It frightens patients because it seems something strange to them, and to some it resembles an accumulation of purulent masses. It should be noted that white plaque in the socket after tooth extraction can be either normal or a complication. In the first case we are talking about natural regeneration, in the second - about alveolitis.
Method for treating patients with trophic ulcers
Owners of patent RU 2578382:
The invention relates to medicine and can be used to treat patients with trophic ulcers. To do this, the surface of the ulcer is treated with a swab moistened with saline solution. After this, cryotherapy is carried out with an applicator maximally cooled with liquid nitrogen to a temperature of -180°C with different diameters of the flat working surface. The exposure time is no more than 5 seconds. The method ensures bloodless, painless and rapid transformation of a chronic wound into an acute one and active closure of the defect, including by removing the necrotic component, fibrin films, biofilms from the surface of the ulcer, reducing colonization and contamination of microorganisms, removing phenotypically altered cells of the edge and base of the wound. 1 salary f-ly, 2 ill., 1 pr.
The invention relates to medicine, in particular to clinical and experimental medicine, and can be used in the treatment of patients with trophic ulcers and non-healing wounds.
Trophic ulcers, regardless of ethology, attract the close attention of various specialists. This is due to both the enormous material costs of treatment and the high social significance of this issue. Regardless of wound etiology, the principles of local management are largely similar. Adequately selected local treatment plays an important role. Currently, new high-tech dressing materials have appeared, the use of which, without a doubt, helps accelerate the healing of chronic wounds. However, the use of these agents without preliminary treatment of the wound is ineffective, since in all cases at the bottom of the ulcer there is fibrin, purulent-necrotic masses and single flaccid granulations in greater or lesser quantities (RU2388418, A61B 17/00, 2010; RU2340305, A61B 18/02 , 2008; RU2278689, A61K 38/17, 2006; RU2203061, A61K 31/47, 2003; Chernetskaya Yu.G. Application dosage form of hydrogels with miramistin and chymotrypsin. Man and Medicine, 2004, p. 848).
To clean the wound and prepare it for active closure of the defect by skin grafting or the use of collagen-containing preparations, the following treatment methods are used: surgical, autolytic, chemical and physical methods.
Classic surgical treatment should include removal of necrotic tissue, fibrin film, and excision of wound edges containing phenotypically altered cells. Surgical treatment transforms a chronic wound into an acute one, shortens the time to epithelialization, reduces exudation, and reduces the risk of infectious complications. It should be noted that full surgical treatment is impossible in the presence of soft necrosis and neuro-ischemic lesions on the extremities (ABI). The group of inventions relates to the pharmaceutical industry, namely to the use of pterostilbene (PTER), or pterostilbene in combination with quercetin (QUER), or any acceptable salt thereof for the prevention of skin cancer or for the prevention and/or treatment of skin diseases selected from psoriasis, atopic dermatitis and allergic dermatosis, by topical administration.
Treatment of non-healing wounds taking into account their cause
When starting to treat injuries of this kind, it is necessary to understand the cause of their occurrence. Further actions will depend on this.
1. First of all, it is necessary to examine the wound for foreign bodies, necrotic tissue, and bleeding and, if necessary, clean it. Please note that it is strongly recommended not to remove foreign bodies yourself! Such attempts may cause additional tissue damage and increase the risk of infection. You need to seek help from a doctor.
2. If local blood circulation is impaired, it is necessary to eliminate the source of pressure on the tissue (change the position of the patient’s body with bedsores, wear looser clothes/shoes for “diabetic” wounds).
3. When treating trophic ulcers on the legs, it is necessary to use compression stockings or bandages - they will help “support” the blood vessels and normalize blood circulation, as well as “pull” the edges of the wound towards each other for faster healing.
4. In case of exhaustion and vitamin deficiencies, it is necessary to provide a normal balanced diet in order to provide the body with the necessary substances for tissue regeneration and the production of collagen - a substance that is actively involved in the early stages of the healing process and helps tighten the edges of the wound.
5.If you have diabetes (of any type), you need to monitor your blood glucose levels.
After creating optimal conditions for wound healing, you can begin to treat and treat it.
Classification of wounds. Wound process
A wound is any tissue damage accompanied by a violation of the integrity of the integument of the body. Such damage can be caused by various factors: mechanical, thermal, chemical, radiation. Combined wounds occur when several types of damaging factors are simultaneously exposed. Simultaneous or time-limited exposure to external damaging factors leads to the formation of acute wounds. Chronic wounds are the result of long-term, ongoing adverse effects on tissue. The nature of this effect is often endogenous, for example, disturbances of arterial or venous blood supply, innervation, or constant leakage of exudate from the purulent cavity. Another common cause of chronic wounds is prolonged local pressure on tissue.
Wounds are one of the most common traumatic injuries. Victims are injured in domestic, industrial, combat and criminal conditions. It is characteristic that most of the victims are of young working age. In addition, wounds are caused during surgical interventions. In the latter case, the main feature is the ability to create conditions that minimize the risk of wound complications. What is common to all wounds except post-operative wounds is that they are always contaminated with microorganisms and are often complicated by the development of infection.
Wound process
The main clinical signs of wounds immediately after their application are the presence of a defect in the skin or mucous membranes, bleeding and pain. Subsequently, the clinical picture corresponds to the phases of the wound process.
The formation of any wound is accompanied by a sequence of local and general reactions of the body. General reactions are more pronounced in the formation of acute wounds. They consist in the typical manifestations of stress syndrome - an increase in all vital processes under the influence of the sympathetic nervous system and hormones, an increase in basal metabolism and catabolism. When tissue breakdown products and microbial toxins are absorbed into the bloodstream, stimulating leukocytes to release cytokines, systemic inflammatory reactions may occur: fever, an increase in the number of leukocytes, tachycardia, and others. In the absence of complications, these phenomena completely stop after 4-5 days.
Local reactions of the body are aimed at restoring the integrity of damaged tissues. The healing of wounds of various organs and tissues has its own characteristics, depending on their morphological structure. The wound process can vary significantly in duration, but is always accompanied by the formation of a connective tissue scar. Without scar formation, only superficial wounds heal without damaging the germ layer of the skin. There are 3 phases of the wound process (Fig. 11. 1).
The inflammation phase begins immediately after injury and, in the absence of complications, lasts an average of 4-5 days. It is characterized by typical vascular reactions - vasoconstriction followed by vasodilation, exudation with the release of plasma proteins, migration and release of blood cells into the damaged area, fibrin loss with delimitation of the damaged area, edema and infiltration of surrounding tissues. Subsequently, fibrin undergoes fibrinolysis, and the wound is cleansed of necrotic tissue and microorganisms with the participation of leukocytes and their enzymes.
The regeneration or proliferation phase lasts on average 2-4 weeks. Regeneration processes begin as early as 1 day after injury, and their duration depends on the size of the wound defect and the morphology of the damaged tissue. Migration of fibroblasts, formation of collagen and ground substance, new formation of blood vessels with the development of granulation tissue at the site of the tissue defect occurs. Exudation and swelling gradually decrease, granulation tissue from the bottom of the wound fills the entire defect. Granulation tissue contains many newly formed vessels and is practically not innervated. During the normal course of the wound process, the surface of granulating wounds is bright, “juicy”; when dressings, high contact bleeding and slight pain are characteristic.
The phase of epithelialization and reorganization of the scar, depending on the morphology of the tissue, lasts from several weeks to a year. Epithelization begins from the edges of the wound simultaneously with the formation of granulation tissue. This process is regulated by the action of epidermal cheilon, which is a contact inhibitor of proliferation. Immediately after the formation of the scar, its restructuring begins: elastic fibers are formed and a new fibrous network develops, and the water content in the scar tissue decreases.
The course of the wound process is influenced by various general and local factors. Common factors include: age, nutritional status and immune status of the patient, various disorders of homeostasis, concomitant diseases, including diabetes mellitus, taking anti-inflammatory drugs, cytostatics, massive antibiotic therapy. Local factors influencing the course of the wound process include the state of the blood supply and the degree of tissue trauma in the damaged area, the level of microbial contamination of the wound and the quality of wound care.
According to the degree of contamination and the presence of signs of infection, all wounds are divided into 3 types: aseptic, contaminated and infected.
· Only surgical wounds with “clean” surgical procedures are aseptic.
· Contaminated are wounds contaminated with microflora, but without signs of suppuration. These include all accidental wounds after they are inflicted and some surgical wounds.
· Infected are purulent wounds, that is, wounds with signs of an infectious-inflammatory process. They are divided into primary infected - formed after operations for acute purulent processes, and secondary infected - wounds that festered during the healing process.
The wound process ends with wound healing. The following types of wound healing are distinguished:
· Healing by primary intention – healing without suppuration. It occurs with the development of a linear scar without the formation of visible interstitial tissue. Such healing is typical for wounds with smooth viable edges, separated from each other by no more than 1 cm, and with microbial contamination of tissues below a critical level. Surgical wounds usually heal by primary intention when primary sutures are applied.
· Delayed primary - healing according to the type of primary intention. This is healing without suppuration with delayed closure of the wound with sutures.
· Healing by secondary intention – healing through suppuration and granulation with the development of a rough scar and the formation of visible interstitial tissue. Occurs with extensive tissue defects that do not allow primary comparison of the wound walls and with the development of wound infection.
· Healing under a scab – healing without a scar. Occurs with superficial wounds without damage to the germ layer of the skin. Under the scab, consisting of fibrin and blood cells, rapid regeneration of the epidermis occurs.
The course of the wound process described above is typical for wounds that were the result of a one-time exposure to a damaging factor. With long-term or constant adverse effects leading to disruption of the functioning of the integument of the body and complicating healing, which occurs in the case of the formation of chronic wounds, it is characteristic that there are signs of all three of its phases at once. The bottom of a chronic wound is simultaneously covered with fibrin and granulations; there may be areas of necrosis and purulent discharge. Granulations are sluggish, pale. The edges of the wound and the surrounding tissue are compacted. Marginal epithelialization often occurs. Typically, palpation of the damaged area is not painful.
The surrounding tissues have changes characteristic of the disease that caused the formation of a chronic wound. If the damaging factors are not eliminated, chronic wounds, even with intensive treatment, do not heal for a long time, and after healing they recur - in the same or in a neighboring area. With long-standing chronic wounds there is a risk of their malignancy.
Causes of non-healing wounds
The immediate cause of non-healing wounds is insufficient activity of restoration processes in the body, slow tissue regeneration. Moreover, the conditions under which regeneration slows down can be varied.
Among the general factors (i.e., affecting the state of the body as a whole), the following can be identified:
• weakened immunity due to concomitant disease or chronic immunodeficiency state;
• chronic intoxication of the body;
• metabolic disease;
• diabetes; this condition can be considered a severe form of metabolic disorder, namely glucose metabolism. Disturbances in the normal absorption of glucose lead to increased tissue fragility and a slowdown in the regeneration process;
• circulatory disorders - both general and local. The cause may be atherosclerosis, deformation of vascular walls, and diseases of the cardiovascular system. Local circulatory disorders can be caused by prolonged compression of tissues and pinching of small blood vessels (an example of a chronic wound against the background of constant compression of tissues - bedsores);
• hypo- or avitaminosis of vitamins A, C, K and group B, which play an important role in the process of tissue regeneration;
• lack of calcium or zinc in the body;
• exhaustion – nutritional (due to insufficient or malnutrition) or senile;
• presence of cancer.
A specific factor in the appearance of chronic wounds is poor circulation in the legs, most often due to varicose veins. Against the background of impaired blood circulation, trophic ulcers develop on the legs (usually in the shins) - difficult-to-heal tissue defects.
Local factors affecting the wound itself and the area around it include:
• infection;
• the presence of necrotic tissue in the wound (they increase the risk of suppuration and, accordingly, the duration of healing);
• presence of foreign bodies in the wound;
• the presence of bleeding in the wound (also increases the risk of infection);
• repeated damage to an unhealed wound.
The risk of a wound becoming chronic increases if, in addition to the skin, other tissues are damaged - subcutaneous tissue, nerves, muscles, tendons, bones.
Operations
If there is phlegmon or an abscess, namely acute suppuration, surgical intervention cannot be avoided. The area is opened and non-viable yellow tissue is excised. This color indicates their death. Then they are sent for examination. Surgeons dry and wash the problem area several times.
Then special tampons are used. They are soaked in saline solution. In case of severe pain against the background of fibrinous plaque, you cannot do without formulations with novocaine. After the operation, stitches are placed. They can be removed after nine days, but only if healing is good and fast.