Dental demineralization is a widespread problem among both adults and children. It not only worsens the appearance of the dentition, but is also a prerequisite for the development of caries, its initial stage. Demineralization of tooth enamel is a pathological process of loss of mineral components by dental tissue, resulting in dullness, hypersensitivity, fragility of teeth, roughness, porosity of their surface, and often the presence of cracks (photo below). The main sign of pathology is the presence on the surface of the teeth of matte white, slightly grayish, or brownish spots of varying sizes, which are located in most cases in the cervical areas, but can cover the entire crown (photo below). Due to the presence of such spots, the pathology is also called focal demineralization of the enamel.
In this article we will tell you the reasons for focal demineralization of enamel, what it looks like in the photo, what features it differs in children, and we will also introduce you to treatment methods and what needs to be done for this disease.
What is dental demineralization
The hardness of tooth enamel is ensured by the content of inorganic substances in it.
It is mainly hydroxyapatite, consisting of calcium and phosphate atoms. Fluoride also adds strength to enamel, protecting it from the harmful effects of acids and microbes. Demineralization refers to the loss of minerals from the enamel. This process causes teeth to become dull and brittle. The enamel becomes thinner and becomes sensitive. Hyperesthesia develops - increased sensitivity of teeth to hot, cold or sour foods. In addition, loss of minerals increases the risk of developing tooth decay. Such teeth become easy prey for bacteria.
Development forecast
Under conditions of proper nutrition and corrected hygiene, in 20-30% of patients, the destruction of enamel stops spontaneously, and the enamel is restored naturally.
In other cases, the loss of minerals leads to the development of caries: the lesion begins to progress from the stage of focal demineralization. On average, 12-18 months pass from the very beginning of the process until the appearance of a carious cavity.
With timely treatment, caries may not develop, teeth can be kept intact and healthy.
Focal loss of minerals is the only reversible stage of caries.
Symptoms of dental demineralization
The main symptoms of demineralization include:
- loss of wet shine in enamel;
- roughness on the surfaces of teeth;
- the appearance of dull spots on the teeth;
- coloring matte spots with food pigments or dyes;
- fragility (porosity) of enamel.
Demineralization in an adult: photo
Causes of tooth demineralization
The main mechanism for the occurrence of pathology lies in the action of acids. In this case, the destructive process occurs according to 2 scenarios:
- under the influence of acids from the outside;
- when acids form in the oral cavity.
In the first case, when a person consumes a lot of acidic foods or drinks (for example, fruit juices, vinegar), the surface layer of enamel becomes thinner over the entire area of the tooth. In the case of acids formed by cariogenic bacteria in the oral cavity, subsurface demineralization of individual lesions/spots occurs. Therefore, focal demineralization in children and adults is a clear sign of the onset of caries.
Among the factors contributing to demineralization are:
- Poor oral hygiene is a major factor contributing to mineral loss.
- Excessive passion for carbohydrate foods - sweets, sweet sodas, juices, flour products. Bacteria process carbohydrates, forming organic acids - lactic, pyruvic, acetic, malic and others.
- Presence of dental diseases.
- Wearing dentures and other orthodontic structures.
- Malocclusion and other dental problems.
- Hormonal changes that contribute to the leaching of minerals from teeth and bones. Most often this concerns women during pregnancy and menopause.
- Metabolic diseases, such as diabetes.
- Diseases of the gastrointestinal tract that impair the absorption of nutrients, in particular minerals.
- Helminthic diseases, in which a significant part of the nutrients and microelements is consumed by parasites.
- Bad habits – smoking, alcohol abuse.
Important: fresh juices . Many people mistakenly believe that there is no harm from fresh juices, because they are a natural drink full of vitamins. However, it is not. Fresh juices contain a lot of sugar. For example, to prepare a glass of apple juice you need to take 3-5 apples. In addition, such juices contain a lot of fruit acids, which is harmful to the enamel.
Focal demineralization of tooth enamel is a widespread disease that occurs in more than 97% of the population of our country [14]. The development of new methods for diagnosing focal demineralization of tooth enamel is determined by the requirements of clinical practice related to the early and timely diagnosis of this pathology in order to use the least invasive treatment methods. The question of assessing the relationship between objective diagnosis of demineralization and adequate treatment in each specific case, taking into account the characteristics of the course of the disease, is also relevant. Most existing methods for diagnosing focal demineralization of tooth enamel are relatively imperfect, since they are based on subjective perception. In this regard, it is relevant not only to introduce objective diagnostics of enamel demineralization into practice, but also to create a clear scale for assessing its degree, which would reflect the depth and area of the lesion.
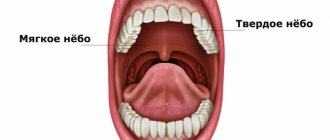
Focal demineralization of enamel is a systemic lesion of the cervical areas of teeth in the form of spots as a result of underdevelopment of tooth tissue and a decrease in the amount of calcium in it. This condition is formed during the period of maturation of tooth tissue after its eruption and corresponds to the ICD-10 code K02.0 - “Enamel caries. Stage of “white (matte) spot” [initial caries].” Caries in the spot stage is characterized by changes in color (matte surface) and then texture (roughness) of the enamel resulting from demineralization, which have not spread beyond the enamel-dentin border, in the absence of a carious cavity [2].
A feature of focal demineralization is that almost all teeth are affected. This process is the only reversible one. Enamel is a mesoporous substance; it does not contain cells and is not capable of regeneration when damaged, but there is a constant exchange of mineral ions in it, which come from saliva through the pores and are adsorbed on its surface, which makes it possible to carry out remineralization therapy [2]. The fundamental local factor in the development of this pathology is a local change in pH on the tooth surface due to the accumulation of dental plaque on it containing acid-forming streptococci ( Streptococcus mutans
,
S. sanguis
,
St.
mitis ,
St.
salivarius ), which are characterized by anaerobic fermentation, and some lactobacilli [21]. Caries develops cyclically, the rate of its development depends, firstly, on the frequency of action of lactic acid produced by microorganisms on the tooth, and, secondly, on the degree of demineralization, i.e., on the penetration of calcium and phosphorus ions into the hard tissues of the tooth (the process catalyzed by fluorine). In addition to fluoride deficiency, for demineralization of tooth tissue to occur, the pH of the oral environment must be below a critical point. On average, the critical pH point is estimated at 5.5 (Stefan curve) [1, 3].
Pathomorphological changes are characterized by varying degrees of enamel demineralization. On thin sections of the enamel, the lesion looks like a triangle with the base facing its surface. When studying enamel in polarized light, G. Gustafsonson (1975) identified 5 zones, depending on the intensity of demineralization. The zone of hypermineralization with the disappearance of structural details of the enamel is located deepest in the thickness of the enamel. In the 2nd zone, a decrease in its hardness was noted due to the partial dissolution of minerals, in the 3rd - an increase in mineralization. In the subsurface, 4th demineralization zone, minerals are washed out almost completely. In the superficial, 5th zone, complete disintegration is possible, but the enamel remains fairly mineralized and intact for a long time, even if the carious process extends to more than half the thickness of the enamel. A. Darling (1958) indicates that if in normal enamel microspaces constitute 0.5% of its volume, then in the body of the lesion they reach 25% of the volume, in dark enamel - 4%, and in transparent enamel - 2% [1].
With a white spot area of up to 3 mm2, changes reach 1⁄2 the thickness of the enamel layer. With more extensive lesions, changes in the enamel are observed down to the enamel-dentin junction. The formation of brown pigment in the spot is associated with the accumulation of the amino acid tyrosine with its further conversion into the pigment melanin. Under a white carious spot, changes in the enamel-dentin junction have not yet been detected; under a brown one, its damage may already be observed [1, 3, 21].
Focal demineralization of enamel is a borderline pathology for which both conservative and invasive treatment is possible. At the same time, there are no clear algorithms for determining a particular treatment plan, despite the wide variety of definitions of the degree of demineralization in enamel caries.
Existing methods for determining demineralization are divided into qualitative and quantitative. Qualitative assessments include clinical assessment. The main quantitative methods for determining enamel demineralization include the following:
1. TER-test (enamel resistance test; V.R. Okushko, L.I. Kosareva, I.K. Lutskaya, 1983). This test reflects the predisposition to caries (based on the functional resistance of enamel to acid). The TER test method boils down to isolating the tooth from saliva, cleaning it from plaque, and drying it. Then 1 drop with a diameter of 1-2 mm of 1% HCl is applied to the prepared tooth. After 5 seconds, the drop is washed off with distilled water, dried, and 1 drop of a 1% solution of methylene blue is applied. The dye is removed with a dry cotton swab in one erasing motion. The etched area is painted blue, the intensity of staining is assessed on a 10-point scale (1-10 points; the maximum score corresponds to the least caries resistance of the enamel)[6].
2. KOSRE-test (clinical assessment of the rate of enamel remineralization according to the method of T.L. Redinova et al.). This test is based on assessing both the condition of tooth enamel and the remineralizing properties of saliva. The enamel surface of the tooth being examined is thoroughly cleaned of plaque with a dental spatula and a 3% hydrogen peroxide solution and dried with compressed air. Then a drop of hydrochloric acid buffer pH 0.3-0.6 is applied to it, always in a constant volume. After 1 minute, the demineralizing solution is removed with a cotton swab. The etched area of tooth enamel is also exposed for 1 minute to a cotton ball soaked in a 2% solution of methylene blue. The compliance of enamel to the action of acid is assessed by the intensity of staining of the etched area of tooth enamel. The degree of staining is judged by the blue topographic tint scale (10-point scale: the least stained part is 10%, the most saturated is 100%). After 1 day, the etched area of tooth enamel is re-stained without repeated exposure to the demineralizing solution. If the etched area of tooth enamel becomes stained, this procedure is repeated again after 1 day. The loss of the etched area's ability to stain is regarded as a complete restoration of its mineral composition. The degree of resistance of tooth enamel to the action of acid is taken into account as a percentage, and the remineralizing ability of saliva is calculated in days. Resistance to caries is characterized by low compliance of tooth enamel to acid action (<40%) and high remineralizing ability of saliva (from 24 hours to 3 days), and caries susceptibility is characterized by high resistance of tooth enamel to acid action (≥40%) and low remineralizing ability. ability of saliva (>3 days) [5].
3. Determination of the initial level of mineralization of erupting teeth using the electrometric method (L.P. Kiselnikova, 1990). The degree of mineralization was assessed using the Dentest electrometry apparatus (ZAO Geosoft). The principle of the electrometric method is that in the hard tissues of fully mineralized teeth and without signs of demineralization, the electrical conductivity is 0. In teeth with reduced mineralization processes, the electrical conductivity values increase. The lower the degree of mineralization, the higher the electrical conductivity. An electric current of 1.8 to 4 μA passes through areas of focal demineralization, localized on the visible surfaces of permanent teeth with enamel mineralization ending. Permeability impairment from 1 to 8 points on the methylene blue staining intensity scale corresponds to an increase in the current value from 1.68 to 5.17 μA. With an increase in the size of the spots, the magnitude of the current passing through the tooth tissue significantly increases from 2.55 to 3.31 μA [7].
The electrometric method makes it possible to determine the general mineralization of the tooth crown, but can only be used to a limited extent for local changes. The absolute values of electrical conductivity vary significantly depending on the tooth, the local thickness of the enamel layer, the ability to carry out insulation and other parameters. The electrometric method is applicable for the relative assessment of changes in the mineralization of a spot on a specific tooth in a specific patient with complete repetition of measurement conditions, which during a clinical appointment can lead to quite serious errors in the results obtained.
4. Determination of focal demineralization of tooth enamel using infrared fluorescence using the DIAGNOdent apparatus.
The DIAGNOdent device (KaVo, Biberach, Germany) was introduced in 1998 by Hebst and Gall as an aid to the detection of caries and focal demineralization of tooth enamel on occlusal surfaces in addition to inspection and radiographic examination. This device works using light emanating from a diode laser; wavelength 655 nm, peak power 1 mW. Light travels through the fiber assembly to the tip of the handpiece. The tip of the handpiece is placed on the surface of the tooth and the laser beam passes through the tooth. Both organic and inorganic molecules in the tooth absorb light. Infrared fluorescence is used. Fluorescence, as well as return light, passes through the tip and enters through the ascending tissues to the photodiode sensor. The fluorescent light is measured and its intensity indicates the size and depth of the tooth's decay or focal demineralization. Fluorescence intensity is presented in the range from 0 to 99. According to prof. Reich (Univ. Hamburg), digital values from 5 to 25 correspond to carious damage to the enamel, 25-35 to damage to half the thickness of dentin, ≥35 to deeper damage to dentin. According to O.A. Krasnoslobodtseva and L.Yu. Orekhova (2000), the indicators for caries in the spot stage corresponded to 9.0±2.0, for superficial caries - 15.0±3.0; average caries - 50.0±30.0. Differences in digital indicators characterizing the condition of dental tissues are explained by different degrees of initial mineral maturity of the diagnosed teeth (EA Kidd, D. Beighton, L. Zoitopoulos, 2001). The reason for the fluorescent glow in the tooth is the presence of protoporphyrins and mesoporphyrins, waste products of bacteria (Hibst and Paulus, 1999, 2000). DIAGNOdent is widely used to detect caries on occlusal surfaces and focal demineralization on smooth tooth surfaces (Aljehani et al., 2006, 2007; Antonnen et al., 2003; Bamzahim et al., 2004, 2005; Lussi et al., 2003, 2006 ). Studies have shown that the sensitivity of the DIAGNOdent device for detecting caries and focal demineralization of enamel ranges from 0.17 to 0.78, and in some cases from 0.72 to 0.98 (Lussi et al., 1999; Shi et al., 2000) [8, 16].
Most studies highlight that DIAGNOdent is much more sensitive to pathology detection than traditional methods. But the increasing number of false-positive diagnoses makes it impossible to use this device as the only reliable one (Bader et al., 2004). Therefore, a definitive diagnosis cannot be made based on DIAGNOdent data alone.
5. Transillumination of focal demineralization of enamel - bright illumination of the coronal part of the tooth to study its structural components; carious lesions stand out as a dark shadow against the background of tooth enamel. The transillumination method also makes it possible to identify enamel cracks and assess the condition of tooth tissue around previously applied fillings [4, 12—14].
This method can only identify pathology, but does not evaluate it qualitatively and quantitatively, which deprives it of objectivity.
Treatment of focal demineralization of tooth enamel has been studied for decades and has a serious scientific basis. Theoretically, remineralization therapy for focal demineralization is justified by the preservation of the protein matrix in the tooth enamel in the early stages of caries (white carious spot), as well as the possibility of remineralization. Many studies have noted that after a course of restorative therapy, the enamel surface becomes more uniform and microporosity decreases. Thanks to the remineralization of enamel, it is possible to stabilize the initial process of its demineralization and even eliminate the chalk stain. The pigment spot remains preserved when the process stabilizes [9].
There are a huge number of remineralizing products - remineralizing pastes, gels, mousses. Let's look at some of them.
Profilak JSC "StomaDent" is created on the basis of domestically produced cedar balsam using a special technology that allows you to maintain the active component - fluorine in a dispersed state, preventing its precipitation.
Significant factors that unite fluoride-containing varnishes are the transformation of hydroxyapatite into fluorapatite and the formation of calcium fluoride in the outer layer of the tooth. After applying fluoride-containing varnishes, the tooth surface is protected by an acid-resistant layer of calcium fluoride.
Clinical studies of the use of fluoride-containing varnishes have proven their high effectiveness in the progression of proximal caries. They should be used immediately after the eruption of permanent teeth, since there are no contraindications for their use.
The use of Profilak is also indicated:
— for the prevention of tooth root caries (2-3 times a year);
— for the treatment of hypersensitivity of teeth (course of 1-3 procedures over 7-10 days);
— on low-calcified teeth (4–8 times a year) [15–17].
Remineralizing gel ROCS Medical Minerals. It is a source of bioavailable calcium, phosphorus and magnesium compounds that strengthen enamel. Thanks to special additives, it forms a stable invisible film on the teeth, ensures gradual penetration of minerals into the tooth tissue, and allows prolongation of the exposure of active components. After brushing your teeth, apply it to your teeth with a brush and refrain from eating or drinking for 30 minutes. Recommended course duration is 2 weeks. From 1 to 3 courses are conducted per year. It is possible to use the gel on an ongoing basis, as it is harmless and does not cause side effects [20].
GC Tooth Mousse is an application cream containing calcium and phosphorus, used by dentists in accordance with the recommended indications. GC Tooth Mousse is a water-soluble cream containing Recaldent™* CPP-ACP (casein phosphopeptide - amorphous calcium phosphate). In the oral environment, CPP-ACP binds tightly to biofilm, plaque, bacteria, hydroxyapatite and soft tissue, delivering calcium and phosphorus. Saliva increases the activity of CPP-ACP, and the pleasant taste of the mousse increases salivation. The longer CPP-ACP and saliva are in the oral cavity, the more effective the result. Recaident™ CPP-ACP is derived from cow's milk casein and should not be used in patients with milk protein allergies. There are known cases of recovery from enamel hypersensitivity after taking GC Tooth Mousse [18, 19].
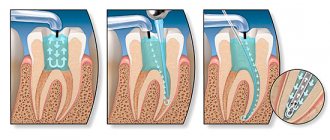
One of the innovative areas for the treatment of focal demineralization is the method of caries infiltration of an area of pathological enamel with a viscous-flowing composite material Icon, developed by the German company DMG in 2009. The method is based on layer-by-layer “impregnation” (infiltration) of the focus of enamel demineralization with a light-curing resin, which is carried out after preliminary etching of the surface, relatively highly mineralized “pseudo-intact” layer of enamel. According to foreign authors [22], the infiltrate penetrates into the intercrystalline pores of the enamel throughout the entire volume of the affected area and, after hardening, strengthens (“reinforces”) the demineralized area of the enamel, generally preventing further progression of the disease [10]. Currently, laboratory and clinical studies are being actively conducted all over the world, which confirm the prospects of using the infiltration method for the treatment of caries in the spot stage [11].
Analysis of publications devoted to methods of diagnosis and treatment of focal demineralization of tooth enamel allows us to conclude that, despite numerous studies in this direction, many unclear questions remain. There are many recommendations and subjective methods for diagnosing this pathology of tooth enamel, but there are no objective standards and a method that gives an accurate quantitative assessment of the lesion. The question of optimizing the indications for the use of certain methods and means of remineralizing tooth enamel, depending on the degree of demineralization of its structure, remains open.
The authors declare no conflict of interest.
Diagnosis of the disease
Diagnosis of suspected demineralization comes down to the following procedures:
- Inspection . The doctor cleans the teeth of plaque and dries them. The presence of white matte spots on the teeth indicates pathology.
- Enamel staining . The doctor stains the cleaned and dried teeth with blue dye. Unlike healthy areas, areas of demineralization are stained. Moreover, the brighter the shade, the more serious the damage to the enamel.
- Application of ultraviolet light . When teeth are illuminated with ultraviolet light, healthy areas glow blue, while damaged areas glow dark.
- Using a laser . The method is based on the fact that areas with different mineralization reflect laser waves of different lengths.
Weakening of tooth enamel
Demineralization is a process in which enamel loses the minerals it needs - calcium and phosphorus.
Normally, they come from saliva and oral fluid through small pores on the enamel and accumulate in areas where there is not enough of them. Then mineralization occurs: mineral components are formed from calcium and phosphorus, which are attached to the protein “skeleton” of the tooth and compact it. When a deficiency of minerals occurs in hard dental tissues, the enamel softens and microdefects appear in it - narrow funnels with a diameter of up to 10 nanometers. They gradually enlarge, merge and form focal demineralization, and in severe cases inflammation of the pulp occurs.
On the website Stom-Firms.ru, read when demineralization of teeth develops, what methods of its treatment and prevention are available.
Demineralization of baby teeth in children
Demineralization of teeth is a common occurrence among children. Two factors are decisive here - poor oral hygiene and a passion for sweets.
As a rule, in children and adolescents, demineralization takes the form of irregularly shaped spots. The color of such formations varies from white to brown. Most often, the pathological process in a child begins in the cervical area, then spreading to other areas.
Important. If demineralization spots have acquired a brown color, this indicates an advanced process. In this case, not only the enamel is affected, but also the dentin tissue.
Demineralization of teeth in a child: photo
Etiology
The main reason at the local level is the presence in the mouth of:
- Cariogenic bacteria - these can be streptococci, lactobacilli and some other species.
- Residues of carbohydrate foods, mainly sugars, where these microorganisms multiply well and comfortably.
As a result of their “violent activity,” the acid-base balance of the oral cavity decreases to a critical level of pH 5.5 and below. Normally, the indicator should be at a pH level of 6.8–7.4. That is, the environment becomes too acidic.
Next, the acids dissolve crystals of hydroxyapatite, a substance that makes up 75% of all enamel minerals. The destruction occurs so quickly that the teeth do not have time to “absorb” all the necessary elements supplied with food.
There is also a second reason - drinking water with a low fluoride content (less than 0.5 mg/l). If the body systematically lacks fluoride, thinning of the enamel will occur regardless of the acidity of the oral fluid.
Demineralized enamel also lacks phosphorus, magnesium, sodium, chlorine, and potassium.
Factors that provoke enamel demineralization
- failure to comply with hygiene rules;
- insufficient secretion of the salivary glands;
- eating soft foods high in simple carbohydrates;
- inflammation of the gums;
- wearing dentures or orthodontic appliances, which prevents the thorough removal of hard deposits;
- crowded teeth - if they overlap each other, it becomes difficult to clean the interdental spaces;
- diseases such as rickets, diabetes, pathology of the adrenal glands;
- hormonal changes.
How to reduce demineralization
You can pause the pathological process (and even reverse it) by following some recommendations:
- Nutrition . Eat foods that contain calcium, phosphorus, vitamin D and fluoride. These are milk and dairy products, fish, meat, legumes, grains, as well as broccoli and eggs. Limit your intake of carbohydrate-rich foods, especially sweets, sugary sodas and juices.
- Ultraviolet . Walk outdoors in sunny weather. Sunlight is necessary for the formation of vitamin D.
- Hygiene . Brush your teeth 2 times a day. If you have a fluoride deficiency, then toothpastes with fluoride will be useful. This element strengthens tooth enamel.
Important: fluorosis . Fluoride is one of the key elements needed to maintain enamel strength. However, an excess of fluoride is no less harmful than its deficiency. When there is too much fluoride, fluorosis develops. This pathology often occurs in regions with high levels of fluoride in drinking water.
Treatment of enamel demineralization
Remineralization is the opposite process of demineralization. It can be natural and artificial. We talked about natural remineralization above. It comes down to replenishing missing minerals with food.
As for remineralization in dentistry, such therapy is carried out in several stages:
- professional teeth cleaning;
- drying the enamel with a stream of warm air;
- treatment of enamel with preparations with a high concentration of minerals, in particular calcium salts;
- fluoridation of teeth - application of preparations with sodium fluoride (gels or fluoride varnish are used).
The treatment plan is worked out in advance by the doctor, based on diagnostic data. The number of remineralization sessions is selected separately in each case.
What is remineralization therapy
The remineralization therapy technique involves applying specialized compounds to the surface of tooth enamel that restore the structure. Usually we are talking about drugs based on fluorine, calcium, phosphates and other useful components.
In dentistry, rem therapy is performed in several ways:
- An express method, the essence of which is to put on disposable mouth guards filled with gel with a fluoride-containing base;
- Application of specialized varnishes that eliminate minor damage and restore the enamel structure;
- Reusable trays for remineralization at home.
The duration of such therapy depends on the degree of damage to the enamel, but usually several sessions are enough to achieve the expected result. Remineralizing dental therapy is a unique and affordable technique, but such treatment is carried out only in combination.
Prevention of enamel demineralization when using braces
Demineralization of teeth during orthodontic treatment is a common phenomenon. Demineralization after braces is associated with difficulties in maintaining hygiene when wearing braces. To minimize the risk of damaging the mineral composition of the enamel, it is recommended to adhere to the following rules:
- thorough dental and oral hygiene - brushing your teeth after every meal using special orthodontic brushes;
- nutrition correction mentioned above;
- professional teeth cleaning with sanitization before installing braces;
- remineralization when wearing braces using mineral gels, pastes and fluoride varnish;
- taking a calcium supplement;
- regular check-ups with a doctor.
Indications for retherapy
Rem therapy for teeth helps restore damaged enamel. If treatment is carried out at the initial stage, the carious changes that appear can be eliminated without drilling and filling.
Dental indications for remineralizing therapy:
- Primary carious changes - the appearance of chalky spots;
- Hypersensitivity is the first sign of thinned enamel;
- Carrying out bleaching - as part of this procedure, a lightening pigment is introduced into the enamel, slightly disturbing the molecular structure;
- Recovery after orthodontic treatment – for example, after removing braces;
- Complicated oral care – for example, in patients with impaired motor function;
- Pregnancy - enamel becomes thinner as a result of hormonal changes;
- After teething - in this case, the mineral composition has not yet been formed, which creates favorable conditions for various dental diseases.
In addition, indications for the use of such therapy include erosion, tooth abrasion, and hypoplasia.