Stages of dental development
There are four conventional stages of dental development in humans . The division into such periods is fair if we are talking about both milk and permanent teeth. MORE· The first stage is the laying of the beginnings of teeth. The formation of the dental rudiments of primary teeth occurs in the embryo in the sixth to eighth weeks of intrauterine development. First, an epithelial plate is formed, then enamel caps. The formation of the beginnings of permanent teeth occurs in the fifth month of intrauterine development of the fetus. The first to be laid are the incisors, then the small molars and canines. The last to be laid are the rudiments of the large molars (in the sixth month of the child’s life) and wisdom teeth – “eights” (only in the fourth or fifth year of the child’s life). · The second stage is differentiation. Differentiation of dental buds usually occurs at the twelfth (maximum fourteenth) week of fetal development inside the womb. During this period, cells are formed - builders of the surface tissue of the tooth (enamel) and cells - builders of dentin (the layer of the tooth located under the enamel). In medical science, such building cells are called adamantine blasts and odontoblasts, respectively. · The third stage is histogenesis. The next stage of dental development is histogenesis. This is the formation of hard dental tissues. The process of histogenesis begins in the fourth month of the baby’s intrauterine development. First, dentin is formed, and then the outer and most durable tissue of the tooth and the entire human body - enamel. · The fourth stage is the development of tooth roots . The development of the roots of both baby and permanent teeth begins after the baby is born. Typically, tooth root development begins shortly before tooth eruption begins. The development of tooth roots ends with the formation of the root apex - this occurs two years after the start of eruption.
Treatment of wedge-shaped defect
Let's first consider traditional methods of treatment.
Applications of various preparations: varnishes, ointments, remineralizing solutions, etc.
The main advantage of this method is compliance with the most important Hippocratic principle: “Do no harm.” Indeed, this method of treatment will not harm the teeth. And it can bring benefits in the form of getting rid of hypersensitivity. True, after 10-15 visits, a single application is only enough for a few hours/minutes. It is impossible to eliminate the resulting defect by application, but you can get rid of the pain for some time.
Using toothpastes that reduce sensitivity (desensitivity)
This method includes all the advantages of the previous one, plus it has one more advantage - low cost. One tube of paste costs much less than 10-15 visits to the dentist, but the effect is approximately the same. Just as in the first case, it will not be possible to eliminate the defect itself and its further development. The maximum that can be achieved is the disappearance of pain in the necks of the teeth.
Filling with various materials
Glass ionomer, compomer, flowable or universal composites.
The most common treatment option for wedge-shaped defects. There are even more advantages: the pain disappears immediately after the first visit, and most importantly, the defect itself is eliminated and a fairly good aesthetic result is achieved. The trouble is that the cause of the disease cannot be eliminated by the most modern, best, most durable, most expensive filling.
This means that the mechanical load on the neck of the tooth will continue its negative impact. As a result, the fillings either fall out entirely, or (most often) remain in place, but at the same time they tear off one of their surfaces from the tooth, forming a gap into which food debris and bacteria become clogged. The photo clearly shows a dark strip between one surface of the filling and the tooth, the so-called “mourning border”.
It is undesirable to leave everything as it is - in addition to the progression of the wedge-shaped defect, you can now also get caries in this place. The old filling is removed, a new one is placed, and everything begins for the second round.
Installation of veneers
A veneer here means a ceramic veneer that covers the entire anterior and chewing (cutting edge of the front teeth) surfaces of the tooth.
This method is even better than the previous ones. In addition to superior aesthetics, it is sometimes possible to eliminate the cause (and therefore prevent recurrence of the disease for some teeth). But this will call into question the strength of the veneer itself. The maximum load will fall on it, and this structure is fragile to a certain extent. It may not be able to withstand the efforts from which the tooth’s own enamel has even been lost.
Therefore, veneers for wedge-shaped defects are most suitable for wealthy housewives and other citizens who have enough time and finances to regularly replace those that fail with new ones.
Manufacturing of artificial crowns (metal-ceramic or all-ceramic)
A radical, but very effective solution to the problem. Provided that the edge of the crown covers the wedge-shaped defect with a margin. But often this very reserve is not there - the defect is already located at the level of the gum, and grinding a tooth below the level of attachment of the gingival margin for a crown is strictly contraindicated. In addition, while protecting some teeth, crowns can put others at risk.
It turns out that even such generally reliable structures as crowns do not always solve the issue completely. A wedge-shaped defect can continue its destructive development on a tooth covered with an artificial crown and on neighboring teeth.
All of the above treatment options have one common drawback - they do not normalize the bite or eliminate the cause of the disease. Therefore, even if some of you, dear ladies and gentlemen, were helped by just toothpaste or a banal filling that has served faithfully for several decades, then consider yourself lucky. “Lucky” is such a capacious term in medicine, meaning that, despite inadequate treatment, a change in the living conditions of the body led to spontaneous self-healing.
In this case, destruction, mobility, installation of a large composite restoration or removal of the antagonist tooth will lead to the elimination of the etiological factor of the wedge-shaped defect. But a patient, much less a doctor, should hardly count on such dubious “luck.”
One of the most important tenets of medicine is: “Treatment must be predictable.” That is, to give a positive result in the maximum possible number of patients. In our opinion, it is not possible for a doctor who considers a wedge-shaped defect to be a “disease of unknown etiology” or who knows the cause, but for some reason ignores it, to achieve such a result.
Teething
The usual
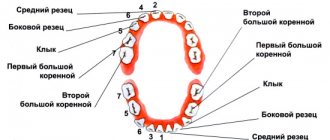
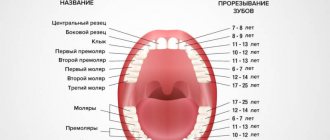
order of baby teeth erupting is as follows: The central incisors of the lower dentition erupt. Usually this process occurs when the baby is six months old. The central incisors of the now upper jaw erupt. The next to erupt are the upper lateral incisors - the neighbors of the central ones in the dentition. It is the turn of the lateral incisors of the lower jaw to erupt. The child is turning one year old and has already cut eight teeth. Before the child is one year and six months old, the child's four molars begin to emerge. After one and a half years, the following teeth erupt in the baby’s mouth - fangs . Then large molars erupt. The child turns two years and six months or exactly three years old , when all twenty milk teeth have erupted. The timing of the eruption of baby teeth may vary - minor deviations from the specified timing are not pathology . If the timing is significantly violated, then this may be a sign of disturbances in the gastrointestinal tract, cardiovascular system, a symptom of an infection in the child’s body or a metabolic disorder. Babies' teeth can erupt either individually or in pairs at once. Long before teething, the baby's salivation increases, and the baby begins to chew on toys or fists more. During the teething period itself, the baby shows increased activity: often cries or screams. The period of teething may be accompanied by a rise in temperature and a cold in the baby.
COST OF SERVICES
Dental clinic No. 2
The anterior teeth of the upper jaw are characterized by both functional and aesthetic parameters.
By their nature, these are the teeth that are visible both when talking and when smiling. That is why there are such a significant number of approaches trying to imitate as much as possible all the subtleties of the anatomy of the teeth of the upper jaw. Considering that in addition to shape, the technician must also understand the characteristics of color, texture, rotation and spatial position of the teeth, it is quite easy for him to get lost in all these details. That is why in this article we will focus not on individual modeling elements, but on a systematic approach to restoring the morphology and structure of the frontal group of teeth.
After completing the modeling of the basic shape, the technician can begin to restore the individual characteristics of the tooth, following the proposed protocol, thereby saving a huge amount of time.
The described approach is unique in both modeling all six anterior units and restoring the shape of a single tooth, regardless of whether the technician is working with wax or final structures, in conventional or digital mode. After all, the most important thing lies in the details, which are emphasized after modeling the basic form of future restorations.
Step by step protocol
1. When restoring several anterior teeth, modeling should always begin from the middle of the row, namely from the labial cutting edge of the central incisors. The middle of the restoration is determined by the median anatomical landmarks of the face: along the line connecting the bridge of the nose, the apex of the nose and the center of the chin. The second interpupillary line (photo 1) is modeled perpendicular to the midline of the face: the cutting edges of the incisors on the labial side should be parallel to the interpupillary line.
Photo 1. Facial landmarks and transfer of the interpupillary line to the horizontal plane of the central incisors.
2. After this, contact points are modeled: the position of those from the incisors to the canines shifts more and more towards the cervical area, as shown in the photo with a red line (photo 2 - 3).
Photo 2. The area of contact points shifts more cervically from the incisors to the canines.
Photo 3. The area of contact points moves more cervically from the incisors to the canines (red lines).
3. At the next stage, the lingual surfaces are modeled. Since all teeth take part in the act of chewing, it is therefore simply impossible to model their lingual surface without taking into account the interaction with antagonist teeth. The cutting edge of the teeth, in essence, is their cutting ridge; in the photo, the line of the cutting edge on the labial side is shown in red, and on the lingual side - blue (photos 4 - 5). These edges are the boundaries of the cutting ridge. We should not forget that the lingual edge of this ridge is not only an aesthetic, but also a functional component that interacts with the lower incisors during chewing, while the labial edge of the upper teeth is visualized when the patient smiles and talks. The labial margin of the restoration can be lengthened or repositioned as long as it does not compromise the function, esthetics and phonetics of the teeth being modeled. The cutting edges are rarely symmetrical and parallel (photos 4 - 5). Simply put, the function of the lingual side of the incisors is derived from their labial contour.
Figure 4. The incisal ridge consists of a labial edge (red line) and a lingual edge (blue line).
Figure 5. The incisal ridge consists of a labial edge (red line) and a lingual edge (blue line).
4. The mesial angle line, which is represented in the photo by a black line, is the next element for modeling (photo 6). If you look at the teeth from the front side, they can be divided into segments vertically (photo 3): the central one can be divided into three parts, the lateral incisors and canines into two. The line of the mesial angle of the central incisor begins near its contact point and ends in the cervical part of the tooth in the region of the mesial third of its lateral side. The line of this angle should correspond as much as possible to the line of the adjacent central incisor. A similar lateral landmark for the lateral incisor begins at or above the contact point and ends in the cervical region near the middle of the tooth side. The line of the mesial angle of the canines also begins above the contact point and moves towards the middle of the tooth.
Photo 6. Mesial angle line (black line).
5. After this, they begin to model the lines of the distal angles (photo 7), again moving from the area of the central incisors to the canines. These landmarks should coincide as much as possible between the teeth on the right and left sides. Of course, the width of a symmetrical tooth may differ, but they can be optically modified to ensure that the lines of the distal angles coincide as much as possible.
Photo 7. The distal angle line moves from the incisors to the canines.
6. The height of the cervical contour, drawn with a white line (photos 8 - 9), should follow the contour of the soft tissues (pink) as much as possible. Therefore, when modeling this parameter, it is necessary to use a duplicate of the soft tissue position. The apex of the cemento-enamel junction of the central incisor is located in the area of the distal third, and the lateral incisor and canine are in the area of the middle of the tooth (photo 6).
Photo 8. The height of the cervical contour (white line) follows the contour of the soft tissues.
Photo 9. The height of the cervical contour (white line) follows the contour of the soft tissues.
7. The last step in modeling is to adjust the labial component of the incisal edge. The shape of this formation (photo 10) can vary greatly, since it does not interact with the cutting edges of the lower incisors during chewing.
Photo 10. Shape of the labial edge.
Typically, the labial edges of the central incisors and canines follow a horizontal line, but during modeling the author uses a Kois Waxing Guide (Panadent) (Figure 11) to ensure that the incisors and canines are exactly in the same horizontal plane.
Photo 11: Kois Waxing Guide is used to check the horizontal plane of the incisors and canines.
If you outline the main forms of modeling without teeth, then everything becomes simple and clear (photo 12). It is important to correctly fill in these lines during restoration and connect the corresponding points correctly. After rough modeling, the technician begins to restore individual parameters. With the vestibular view of the teeth, the distal side of the canines disappears from the field of view or is very faintly traced (photo 13), so the visual shape of the dental arch can be expanded due to better visualization of the distal side of the third teeth.
Photo 12. View of the base lines without teeth.
Photo 13. In the vestibular view, the distal part of the canines is faintly visible.
Prognosis for hyperesthesia and preventive measures
If treatment is started early, the prognosis is favorable. A complex of clinical procedures plus compliance with medical recommendations leads to the onset of stable remission without pain, discomfort, or the risk of complications.
To prevent the development - initial or repeated - of hyperesthesia, it is recommended:
- bring your diet back to normal, limit your intake of foods that destroy enamel. To do this, it is necessary to exclude or limit carbonated drinks and excessively sour dishes in the diet, and use a straw when drinking juices;
- enrich your diet with foods containing calcium and phosphorus - they will help the body maintain optimal mineral balance and bone strength;
- After each meal, it is always recommended to rinse your mouth with a special mouthwash or regular warm water;
- undergo preventive examinations of the oral cavity every six months so as not to trigger the development of carious and non-carious diseases. The latter are especially dangerous, since outwardly they are invisible, and the dentist will identify them in time and provide assistance;
- monitor the condition of the stomach and the entire gastrointestinal tract, since their system directly affects the condition of the teeth.
Therapy for hyperesthesia
Hyperesthesia is treated comprehensively, in collaboration between the doctor and the patient, because it involves clinical manipulations, specific procedures and self-care.
First of all, the cause of hypersensitivity is eliminated - periodontitis, periodontal disease are treated, low-quality orthopedic structures and fillings are replaced, and cervical defects are eliminated. If there are indications, microplastic correction of the gums is performed, during which it is raised to a normal level and the exposed roots are covered.
Conservative therapy should normalize hydrodynamics in dentin microchannels. Remineralization will reduce the volume of microspaces and normalize phosphorus-calcium metabolism. The patient needs to undergo a course of treatment, during which every day 10 percent calcium gluconate is applied to the surface of the teeth and the enamel is coated with a fluoride-containing preparation.
In order for the life-saving ions to better penetrate the dental tissues, electrophoresis is used. Physiotherapy makes it possible to introduce certain ions and control their concentration. Electrophoresis is absolutely safe if it is carried out by a competent specialist, and the drugs injected into the tissue are non-toxic. Physiotherapy lasts about 2 weeks, but already at the beginning there is an improvement in well-being, and by the end of the course of treatment a stable remission occurs.
The duration of remission will depend on many factors - the characteristics of a person’s hard dental tissues and the quality of self-care for teeth. If conservative therapy with saline applications does not produce a pronounced effect, the enamel is covered with filling material, but this usually occurs in advanced or clinically complex cases.
Competent, predictable, reliable treatment of a wedge-shaped defect is optimization of occlusion
To do this, a comprehensive occlusion analysis is first required. This is done both through a detailed examination of the maxillofacial area and by studying the movements of jaw models in the articulator. Next, when traumatic factors are detected, the most rational way to optimize occlusion is chosen. There are three directions: orthodontic (installation of braces), orthopedic (production of artificial crowns for individual teeth, most often fangs) and selective grinding.
And usually you have to work in two of these three areas. The treatment process is slow (especially if orthodontic care is required), but in the end an excellent result is achieved. When the occlusion is in order, then any of the five above-mentioned techniques can be used. You can put a beautiful filling, or an even more beautiful veneer, an absolutely magnificent crown, or just get by with an applique if the defect is just beginning.
In conclusion, it is worth noting one important fact. By analyzing the occlusion, the gnathologist can detect early signs of other diseases. After all, a wedge-shaped defect is only a symptom, and far from the worst, of incipient dental dysfunction. Optimizing occlusion will not only eliminate wedge-shaped defects, but will also protect against such things as cracks and chips of your teeth, as well as previously installed fillings, veneers, crowns, periodontal trauma, gum recession, false pulpitis, myalgia, and joint pain.
Such a pleasant bonus is awarded to those patients who choose the most rational method of treating a wedge-shaped defect. We wish you not to make a mistake in your choice.
Clinical picture of hyperesthesia and degree of hypersensitivity
Hyperesthesia can manifest itself in different ways. A typical sensation is intense, albeit short-term pain (about 30 seconds), a “shooting” in the jaw due to hot or cold (more often), very salty, sweet, sour foods and drinks. Sometimes severe pain occurs when inhaling cold air.
With hyperesthesia, this reaction occurs constantly, the relief is short-term and insignificant. The patient often cannot identify the tooth that is causing pain. An external examination does not reveal any difference between the teeth in the row, there is no pathological pigmentation, the enamel appears hard and smooth.
Degrees of the pathological process:
- Discomfort is caused by heat or cold exposure, the threshold values of dentin excitability are 5-8 μA.
- Discomfort is caused by heat, cold, salty, sour, sweet; the threshold values of dentin excitability are 3-5 μA.
- Pain is provoked by all irritants, including simple touch; the threshold values of dentin excitability are 1.5-3 µA.
Hypersensitivity significantly complicates oral care; even ordinary cleaning becomes a challenge, and if the process is developed and neglected, it becomes impossible. The enamel and interdental spaces gradually accumulate deposits, which can lead to caries, gingivitis, and periodontitis.
In order not to provoke the development of serious complications, the consequences of hyperesthesia, you need to contact a specialist already at the first stage of the process, with mild sensitivity.