Pain after tooth extraction: how long does it last, and is it normal? These and other questions concern patients after dental procedures. Pain syndrome is normal in several cases: early postoperative period, complex removal, simultaneous implantation.
Normally, pain can persist from several days to a week, and its intensity should decrease. The appearance of symptoms such as increased pain, swelling, inflammation, bleeding or the appearance of purulent exudate is a reason to immediately consult a doctor.
How does a postoperative wound heal?
How long the area hurts after tooth extraction depends on many factors. The healing process after tooth extraction is a complex and lengthy process. Removal occurs with a rupture of the dentofacial connection, namely the connection with the alveolar process and the jaw bone.
The recovery process lasts about two to three weeks. Much depends on the surgical protocol, the clinical situation and the characteristics of the body.
Main stages:
- Formation of a blood clot. Forms 1.5-3 hours after extraction. The function of the clot is to protect the wound area from pathogens and secondary infection.
- Active tissue regeneration. The affected mucous membranes are restored, after 3-4 days swelling and inflammation decrease.
- Formation of granulation tissue. After 4-6 days, granulation tissue forms on top of the clot - the basis of a new epithelial layer.
- Granulation proliferation. After a week, the granulation tissue grows, completely covering the socket.
Already on the eighth to tenth day, the wound is completely healed and by the end of the second week a new epithelial layer is formed.
After two weeks, bone tissue begins to renew. After six months, the bone tissue in the area of removal becomes completely healthy.
Prevention of complications after tooth extraction
Tooth extraction is a radical measure when other treatment methods have proven ineffective. To avoid long subsequent recovery, you must follow your doctor's recommendations.
In the first hours after the procedure, do not smoke or eat. These are important rules that many people ignore, which leads to infection in the socket.
On the day of tooth extraction, do not actively rinse your mouth.
This may damage or flush out the blood clot that helps the socket heal. Do not drink alcohol until the wound is completely healed. Alcohol increases bleeding. Avoid strenuous physical activity, and visiting public places such as swimming pools and lakes is also prohibited. It is impossible to warm up the injured jaw area, so in the first week do not visit the sauna, bathhouse or take a hot bath.
Causes of pain
The occurrence of pain after tooth extraction is associated with damage to nerve endings, vascular structures and soft tissues. The peak intensity of pain occurs in the first hours after the cessation of anesthesia. The symptom persists for about 12 hours.
In case of incisions in the gums or damage to the bone tissue, as well as after implantation after removal, toothache may persist for 2-3 days. Pain syndrome also occurs in the case of displacement of the dentition towards the formed void. Therefore, doctors recommend prosthetics as soon as possible after extraction.
Causes of inflammation of the trigeminal nerve on the face
Usually the disease is caused by infection or bacteria. List of reasons why inflammation of the facial nerve may occur:
- Temporomandibular joint injuries
- Tumors (benign and malignant) of the brain and facial area
- Anomalies of skull development
- Skull injuries - birth, fracture, base, damage to the face or jaw
- Polio
- Pulmonary tuberculosis
- Otitis
- Sinusitis
- Chronic caries
- Inflammation after tooth extraction or treatment
- Hypertension
- HIV and AIDS
- Poisoning
- Inflammation of the middle ear
- Severe hypothermia of the head
- Changes in hormonal levels in women
- Gum inflammation
- Ramsay Hunt syndrome
- Stroke
- Bell's palsy
Causes range from minor to life-threatening illnesses. Each of the reasons determines the further treatment of the patient. In some cases, special tests are performed for diagnosis - auditory, lacrimal, infectious, salivary or gustatory. In this way, the functioning of the receptors and sensory organs is checked.
Pain during difficult removal
The duration of pain after complex extraction (wisdom teeth, impacted or dystopic incisors) is associated with damage to a larger tissue area. Often such an operation involves making an incision in the gum, sawing out the roots, extracting tooth fragments, and draining an abscess, which increases the scope of the surgical intervention. If your ear hurts after wisdom tooth removal, this may indicate nerve damage.
In some cases, patients complain of persistent discomfort and pain for up to a week. Clinical manifestations such as swelling, swelling of the gums, enlarged submandibular lymph nodes, fever, and malaise are also common.
Paresthesia after surgery
Paresthesia occurs if a nerve is damaged during tooth extraction. It is characterized by numbness of the facial muscles or tongue. This usually happens after removal of the figure eights, because they are located in close proximity to the facial nerves. Typically, this symptom goes away on its own within one or two weeks, but in severe cases it can linger for a long time or become permanent. This is a fairly rare consequence of the operation.
Paresthesia occurs infrequently
Types of pain
The nature and type of pain depends on the type and surgical intervention, the duration of the operation, and the complexity of the clinical process. Clinicians distinguish the following types:
- Aching. It is felt immediately after the anesthesia wears off. Keeps for about 2-4 days. The jaw may ache when opening the mouth or chewing.
- Intense, enduring. Occurs during extraction of a complex tooth with drainage or opening of a purulent cavity.
- Phantom. Occurs after traumatic surgery and may be felt from time to time. Phantom pain occurs with weak immunity and a low pain threshold.
It is difficult to say how intense the pain will be in each specific case, which is why it is so important to follow medical recommendations to prevent complications.
What is the facial nerve?
The trigeminal nerve, also known as the facial nerve, is the largest of the twelve cranial nerves. It originates in the ear, after which it branches, the first path reaches the frontal part, the second is located at the jaw. The nerve goes around almost the entire surface of the human face; it literally controls it.
Every person has two facial nerves - one on each side of the head. It is in contact with other cranial nerves and has supersensitive fibers.
Doctors divide the disease into two types - primary and secondary. The primary one manifests itself as a complication from a cold, in this case the normal nutrition of the nerve is disrupted. Secondary occurs with severe intoxication against the background of inflammatory or infectious diseases, as well as tumor processes.
What else can pain indicate?
Severe pain after removal may indicate the development of complications. Pulsating pain that radiates to the ears and submandibular lymph nodes is not normal. The most common causes of complicated postoperative pain are the following factors:
- Violation of treatment protocol. Unfortunately, mistakes do occur, especially in the removal of complex teeth. The techniques and approaches used in different clinics may differ from the standards. Errors include leaving fragments of materials or a splintered tooth root behind.
- Alveolitis. Occurs in the absence of a blood clot. The disease complicates natural healing and interferes with normal tissue regeneration. That is why doctors do not recommend touching the wound with your tongue or rinsing your mouth intensively.
- Dry hole. One of the common complications and the cause of long-term pain after tooth extraction. Despite the moisture of the mucous membranes, bone tissue is visible at the bottom of the wound opening. This problem is typical for smokers during periods of hormonal surges. The doctor seals the wound with a swab containing medication.
- Trigeminal neuritis. Long-term pain persists when a tooth in the mandibular row is removed if the trigeminal nerve is damaged during the manipulation. Damage may be accidental due to structural anomalies or multiple branching of nerve structures.
The likelihood of complications developing is low if the removal protocol, medical recommendations after extraction, and timely response to alarming manifestations are followed.
Why can odontogenic sinusitis occur?
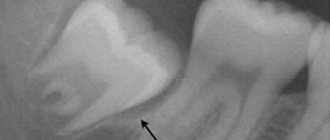
The maxillary (maxillary) sinus is a cavity with bony walls that is located inside the upper jaw. The cavity communicates with the nasal cavity through the anastomosis, which is located on the side wall of the sinus facing the nasal cavity. The lower wall has contact with the upper teeth. Quite often (in about 15% of cases) the apex of the tooth root lies directly under the mucous membrane of the bottom of the maxillary sinus, and there is no bone septum between them.
When an infection enters the maxillary sinus, inflammation of its mucous membrane or sinusitis occurs.
There are two ways of infection:
- rhinogenic - through the nasal cavity. In this case, the infection penetrates from the nasal cavity through natural or artificial (after surgery) communication;
- odontogenic - through the tooth or tissue around it.
Odontogenic sinusitis most often develops slowly against the background of chronic infection in the area of the tooth root. As a result of chronic inflammation, a cyst forms in the root area, which destroys the barrier between the sinus and the tooth. Pathogenic microbes gradually penetrate the sinus mucosa, causing inflammation.
Also, odontogenic sinusitis can occur as a result of the actions of the dentist. Often, after the removal of the upper tooth, the thin barrier between the sinus and the oral cavity may be damaged. As a result, a gateway for dental infection appears. In this case, the anatomical features of the patient with a thin bone septum between the sinus and the tooth root or its complete absence are of key importance.
Infection can occur when cleaning the canals and filling them. In some cases, the filling material gets inside the sinus, causing the formation of fungal sinusitis, and the zinc contained in the filling material promotes the growth of mold fungi (Aspergillus, Mucora). Also, odontogenic sinusitis can develop after the sinus lift procedure and the installation of dental implants in the upper jaw.
How can you reduce pain?
In the early postoperative period, it is important to follow basic recommendations that reduce the risk of negative manifestations:
- maintain the integrity of the blood clot - do not touch the wound with your tongue, rinse vigorously with solutions or water, just take an antiseptic or herbal decoction into your mouth, hold for a few minutes and spit;
- after a complex removal, take broad-spectrum antibiotics - this is important to prevent the infectious process;
- taking symptomatic medications for up to 2-3 days - in the first days, medications help reduce pain and inflammation;
- use a gel with a cooling effect for intense pain;
- do not eat for two hours after surgery, and eat solid food in the area of manipulation for 5-7 days.
You can reduce the pain if you chew a piece of ginger or propolis on the healthy side of the jaw, apply ice through a handkerchief to your cheek or chin, and rinse with the following ingredients:
- tea tree (10 drops per 500 ml of boiled water);
- steep chamomile decoction;
- decoction of eucalyptus and string;
- soda-salt solution (1 tsp soda, 1 tsp salt, 500 ml water).
The temperature of rinsing solutions should be comfortable - neither cold nor hot. Herbal solutions are best used as an alternative 3-5 days after surgery. In the early period, it is better to rinse the wound and oral cavity generously with water-based antiseptics.
The appearance of pain after tooth extraction is associated with trauma to the deep layers of the jaw structures. The tooth can hurt from several hours to 3-7 days, depending on the severity of the clinical situation and the scope of medical intervention. If questionable symptoms or other signs indicating complications appear, it is recommended to consult a doctor.
Treatment of otitis media
If you have otitis media, treatment can only be prescribed by an otolaryngologist. Treatment of otitis media depends on the stage of the disease and the patient’s condition.
In acute eustachitis, treatment of otitis media is aimed at restoring the functions of the auditory tube. Sanitation of the paranasal sinuses, nose and nasopharynx is carried out in order to eliminate infection - rhinitis, sinuitis, etc.).
Vasoconstrictor nasal drops (otrivin, nazivin, etc.) are prescribed; in case of excessive mucous discharge from the nose, drugs with an astringent effect (collargol, protargol) are prescribed. Catheterization of the auditory tube is carried out using aqueous solutions of corticosteroids, and pneumomassage of the eardrums.
In the stage of acute catarrhal otitis media, catheterization of the auditory tube is carried out with the introduction of aqueous solutions of corticosteroids and antibiotics (penicillins, cephalosporins) into the cavity of the middle ear. Local anesthesia is prescribed (otipax drops, Anauran, Otinum). An intra-ear endaural microcompress according to Tsytovich is carried out: a cotton or gauze turunda soaked in a drug with an analgesic and dehydrating effect is inserted into the external auditory canal. Painkillers with an antipyretic effect (nurofen, solpadeine, etc.) are also prescribed. If there is no effect from symptomatic therapy, antibiotic therapy is prescribed within 48-72 hours.
Purulent otitis in the pre-perforated acute stage requires the same set of procedures as in the second stage, but supplemented with the following measures:
- prescription of penicillin antibiotics (amoxicillin, etc.), cephalosporins or macrolides;
- paracentesis (incision of the eardrum) when the eardrum appears to bulge.
It is important to prevent complications of the disease at this stage. After spontaneous opening of the eardrum or paracentesis, the disease progresses to the next stage.
The post-perforation stage of acute purulent otitis media involves the following treatment regimen:
- started antibacterial therapy continues;
- catheterization of the auditory tube is performed with the introduction of corticosteroids and antibiotics;
- a thorough toilet of the external auditory canal is carried out daily - cleaning it from purulent contents;
- transtympanic infusion of drops with an antibacterial and anti-edematous effect is prescribed (alcohol-based drops (otipax, 3% boric acid solution) are not used in this case).
In the scarring stage of AOM, spontaneous restoration of the integrity of the membrane occurs, and all functions of the ear are completely restored. However, this period requires mandatory observation by an otolaryngologist: there is a danger of chronic inflammation in the middle ear, its transition to a purulent form, or the development of an adhesive scar process in the tympanic cavity. It is also possible to develop mastoiditis.
1 Audiometry in MedicCity
2 Audiometry in MedicCity
3 Audiometry in MedicCity
In case of acute otitis media, timely contact with an otorhinolaryngologist is very important. The only measure to prevent complications is correct and timely diagnostic and treatment measures for otitis media. Sometimes the consequences of acute otitis media are adhesions in the tympanic cavity (adhesive otitis media), dry perforation in the eardrum (dry perforated otitis media), purulent perforation (chronic suppurative otitis media), etc. In addition, AOM can lead to such complications as such as mastoiditis, labyrinthitis, petrositis, meningitis, sepsis, venous sinus thrombosis, brain abscess and other life-threatening diseases of the patient.
FAQ
• Is it painful to remove a tooth?
Painless tooth extraction using local anesthetics is carried out by absolutely all dental clinics. But if “freezing” is not enough, then it is better to go to a private clinic that provides all types of pain relief.
• How do you know when a tooth needs to be removed?
If it is very loose or the crown is completely destroyed, then most likely it will be removed. In other cases, accurate diagnosis is necessary.
• Is it possible to have a tooth removed if you have a cold?
Surgical intervention is unacceptable in the presence of an acute infection, including acute respiratory infections or influenza. This is due to the high probability of infection of injured tissues.
• Is it possible to remove a tooth if you have sinusitis?
The operation is not performed during exacerbation of the disease.