From this article you will learn:
- Wisdom tooth removed - how long will it hurt?
- what are the complications?
- How long does it take for gums to heal after wisdom tooth removal?
The article was written by a dental surgeon with more than 19 years of experience.
According to statistics, after the removal of a wisdom tooth, inflammation of the socket of the extracted tooth occurs in 25-30% of cases. For example, after the removal of any other groups of teeth, inflammation occurs only in 3-5% of cases. This is due: firstly, to the higher complexity of removing wisdom teeth, and secondly, to the fact that they are surrounded by a large amount of soft tissue.
The last circumstance is very important, because the presence of moving soft tissues in the area of the extracted tooth socket often leads to the loss of the clot - its loss or even destruction. If the socket of the extracted tooth is not closed by a blood clot, inflammation will inevitably develop in it.
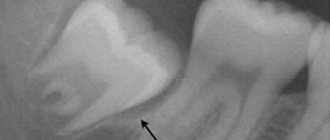
Gums after wisdom tooth removal (normal) –
When wisdom teeth are removed, stitches are almost always required. This is necessary because these teeth are located deep in the soft tissues and in this place the mucous membrane is very mobile. The absence of sutures in this situation can lead to prolapse of the clot and inflammation. But if the patient has a long jaw and there is enough space for the wisdom tooth, the socket will look traditional (Fig. 3).
To learn how the sockets of extracted teeth should normally heal, and how to speed up this process, read the article: “How long should gums take to heal?”
Carrying out the procedure
The tooth extraction procedure is carried out using effective, modern painkillers, so, as a rule, there is no pain during the operation itself.
The operation begins immediately after the anesthesia takes effect. A scalpel is used to loosen the ligament supporting the tooth.
If the procedure was traumatic, or the edges of the wound are too wide, the dental surgeon may use self-absorbing sutures. But most often, the wound is simply closed with a gauze pad with a special hemostatic agent. To stop bleeding, you need to lightly but firmly press the tampon onto the wound with closed jaws. After 20 minutes, the gauze can be spat out.
Main treatment methods
Your dentist will tell you what treatment and gum care should be like after tooth extraction. Only he can select the right drugs that are suitable specifically for your case.
Among the most common treatment methods are the following:
- Careful rinsing with preparations and tinctures with various herbal ingredients and antiseptics.
- Local application of soothing ointments and gels.
- Drug treatment. Your doctor may prescribe antibiotics, painkillers, and anti-inflammatory drugs. But we do not recommend using any medications without a prescription.
Gum condition
Pain in the gums may occur after the anesthetic drug wears off, that is, after 3-4 hours. After the procedure, the patient is often worried about the return of painful sensations and the release of ichor (for 4–6 hours. After the operation, the wound looks quite scary, especially if a wisdom tooth was removed.
In the absence of pathology, the healing process occurs in several stages.
How to rinse your mouth
Recommendations after molar tooth extraction always include a ban on rinsing on the first day after surgery - this procedure can remove a blood clot from the socket.
In the following days, rinsing with herbs - a decoction of oak bark, chamomile, calendula - will be useful to relieve inflammation and speed up the healing process. Among the medications you can use miramistin, furatsilin or chlorhexidine. A water-salt solution is also suitable.
The rinsing technique is simple: take the solution or decoction into your mouth, hold it for 20 minutes and carefully spit it out. No sudden movements.
Day after the procedure
At the initial stage, the hole remaining in the place of the pulled out tooth is filled with a scarlet blood clot. It is not recommended to remove it, as it performs several functions:
- protects the wound from infections;
- eliminates bleeding from blood vessels;
- promotes the formation of new tissue that will fill the empty space.
To avoid breaking up the blood clot, it is recommended not to brush your teeth on the day of surgery. Smoking is accompanied by inhalation of smoke, which creates negative pressure in the oral cavity. This may help pull the clot out of the socket. It is not recommended to blow your nose or spit. Rinsing your mouth should also be avoided; you can simply put the solution in your mouth and hold it for a while without rinsing. Gentle rinsing can be indicated only in the presence of inflammatory and purulent processes.
What happens in the oral cavity during the extraction of the eighth tooth?
When deciding how to treat a particular patient, the doctor takes into account the characteristics of his physical and emotional state. Particular attention is paid to the presence of allergies to medications.
If there are no contraindications to extraction, the doctor administers an anesthetic. When the area becomes insensitive, the gum bends back and grabs the wisdom tooth with forceps. Begins to make rocking movements, allowing you to loosen the periodontal connection and extract the diseased tooth.
Since during the operation the vessels through which blood flows to the pulp tissues are damaged, bleeding occurs. Nerve impulses indicating trauma are transmitted to the brain. Then pain appears. But due to the action of the anesthetic, the patient does not feel it at first.
The hole formed as a result of the operation is heavily supplied with blood. Leukocytes rush here. Swelling occurs and inflammation develops.
Immediately after surgery, the doctor closes the wound with a sterile cotton swab. It helps stop bleeding and creates conditions for the formation of a dense blood clot. The latter is needed to prevent the penetration of pathogenic microorganisms into the tissues of the wound surface. Do not remove the tampon before the doctor says!
After three days
The blood clot begins to change and thicken. Gray and white fibrin stripes appear on it, after which the formation of new gum tissue begins. Painful sensations may still occur. But they are much weaker and have a pulling character. The patient may experience bad breath. This is considered normal and is due to the formation of a blood clot. Failure to brush your teeth also leads to the formation of bacteria and an unpleasant odor.
To rinse the mouth, you must use special solutions recommended by your doctor. The appearance of pain from touching the gums, increased pain during eating, serves as a signal for the need to return to the dentist's office. If the tissue of the edges of the hole has acquired a red tint, you should also immediately consult a specialist.
Sinusitis, maxillary sinus cyst, loss of sense of smell after visiting the dentist
The roots of the teeth of the upper jaw can normally be adjacent to the maxillary (maxillary) sinuses of the nose and even survive in them . Sinusitis, maxillary sinus cyst and loss of smell are possible when infection or filling material penetrates from the teeth into the paranasal sinuses. Unfortunately, this is not uncommon. Moreover, some cases of persistently recurrent sinusitis are associated with infection penetrating from the roots of the teeth . In this case, a possible symptom is a strong unpleasant odor from the nose and mouth.
Odontogenic sinusitis after treatment by a dentist
Odontogenic sinusitis (scheme). Teeth and maxillary sinus. On the left is the norm. On the right – the root of the “seven” (tooth 2_7) is destroyed, inflammation around the destroyed root, pus in the maxillary sinus.
Filling material in the maxillary sinus and sinusitis after filling the “six” canals (tooth 2_6). Pain in the left side of the face after visiting the dentist.
1 – roots of teeth, 2 – normal, air in the right maxillary sinus (front view, the air looks black in the picture), 3 – in the left maxillary sinus there is a fragment of filling material surrounded by an inflammatory shaft. The patient had been mistakenly receiving treatment for trigeminal neuralgia for a long time.
Cysts of the maxillary (maxillary) sinuses in diseases of the roots of the teeth.
1 – roots of the teeth, 2 – cysts of the maxillary sinuses, growing from the roots of the teeth (cysts are round “bubbles”, they look gray in the picture).
How can we help you:
- Let's find the source of pain after dental treatment;
- We will treat inflammatory processes, sinusitis, sinusitis and neurological complications; if necessary, your health will be taken care of jointly by a neurologist and an ENT doctor. Treatment of sinusitis without puncture
After 2–3 months and beyond
The gum gradually hardens, and the space remaining from the tooth is filled with maturing bone tissue. By the beginning of the 4th month, the gum bone tissue completes its formation. The gum can be called completely healed.
If the wound heals with suppuration, then healing of the wound can last up to six months.
How long does it take for a dry socket to heal?
Many people are interested in the question of how long it takes for a dry socket to heal. In the absence of complications, the wound heals in 5 - 7 days, and within a month the hole is filled with epithelial tissue. If you have dry socket, the healing process may take longer than two weeks (with proper treatment, of course). As already mentioned, extensive inflammation may occur and even require surgical hospitalization of the patient: in this case, the healing of the dry socket may be very delayed.
Gum healing process
The speed of gum healing depends on several factors:
- individual characteristics of the patient’s immunity;
- the success of the operation;
- location of the extracted tooth.
If the tooth is in a hard-to-reach place, has crooked roots, or its crown has been significantly damaged, then the removal procedure becomes more complicated. During manipulation, the tooth may begin to crumble, leaving fragments in the gum. In this case, it is necessary to cut the gum tissue, detach it from the bone, remove the tooth in parts, and use a drill. These traumatic procedures prolong the period of gum healing after surgery.
Slight swelling of the gums is considered normal. The temperature may rise slightly (due to an immune reaction). The swelling usually subsides within three days.
Noticeable swelling of the gum is also observed after cutting it. This swelling goes away in about one week.
The jaw hurts and clicks after prosthetics or dental treatment
Dysfunction of the temporomandibular joint. The lower jaw is connected to the skull by two temporomandibular joints. Impairment of the function of these joints is possible after the installation of a denture, crown, bridge, any treatment or tooth extraction if this leads to malocclusion and/or damage to the temporomandibular joint. This is a typical complication after dental prosthetics. Read more about treating TMJ dysfunction here
Temporomandibular joint dysfunction
The green arrow indicates a healthy joint. The red arrow points to the joint that remains in the “open” position when the mouth is closed. This leads to wear and tear of the articular cartilage, pain and clicking when opening and closing the mouth. One of the reasons is the incorrect position of the upper right “eight” (tooth 1_8 lies horizontally).
How can we help you:
- Anti-inflammatory treatment will help relieve pain. If necessary, we inject anti-inflammatory medication directly into the lower jaw joint . This brings relief within a few minutes .
- Injection of botulinum toxin preparations (for example, Botox or Dysport) into spasmodic muscles. This is relevant in the case of an excessive increase in the tone of the masticatory muscles, if it is the muscles that are the “culprit” of dysfunction of the temporomandibular joint.
- Treatment by an osteopath. An osteopath works with the joints and muscles of the jaw using gentle manual techniques. This way you can solve a lot of problems that cannot be solved in classical dentistry. More about osteopathy
- Introduction of chondroprotectors (medicines for nutrition and restoration of cartilage) into the temporomandibular joint. Read more about cartilage restoration
Possible complications
Signs of alarm should be considered an enlargement of the cheek, further spread of swelling, a persistent increase in temperature, increased pain, nausea, and weakness. If the healing process is disrupted, the following complications may occur:
- Cyst formation. It is a fibrous neoplasm filled with fluid.
- Flux. Formed after infection penetrates into the socket and then into the periosteum. The resulting inflammation is characterized by severe swelling of the cheek on the side of the diseased gum. There is severe pain and redness of the gums. The formation of flux requires immediate medical attention. Therefore, it is necessary to carefully protect the site of the extracted tooth from possible infection.
- Alveolitis. This is a complication that occurs during the inflammatory process of the hole in the jaw bone. The infection occurs due to a violation of the integrity of the protective blood clot. The onset of the disease is characterized by inflammation of the outer layers of the socket, spreading into the deep layers of the bone. Alveolitis is accompanied by aching pain during eating, swelling and redness of the gums. There is a putrid odor from the mouth. The patient feels chills, headache, and fever. The occurrence of the disease most often occurs during the extraction of molars located on the lower jaw. It is necessary to obtain medical attention in a timely manner to avoid the spread of infection to other organs. One of the dangerous complications of the disease is osteomyelitis.
Removing wisdom teeth is a more complex procedure, so gum inflammation often occurs after surgery. At the same time, discoloration or swelling of the gums should not cause concern to the patient. Often after surgery there are difficulties opening and closing the mouth. This is a consequence of surgery. To get to a hard-to-reach place, the doctor asks the patient to open his mouth as wide as possible. The pressure exerted on the tissues leads to their swelling. On the 3rd day, the discomfort usually goes away completely. The appearance of purulent contents in the hole, increased temperature, acute pain, heavy bleeding - all these signs require immediate contact with the dentist.
How does the regeneration process proceed after extraction of the “eight”
The socket of an extracted wisdom tooth is always deep. This is due to the structural features of the “eights” - they have tortuous and long roots, which cannot be extracted from the gum tissue atraumatically. Blood flows from the wound for some time. This is due to the rupture of local microvessels. Then she curls up. Then a dense blood clot forms. It is needed to protect tissues from infection.
After the operation, the doctor applies a sterile gauze swab to the hole. To fix it, the patient must close his jaws. This helps stop bleeding as quickly as possible. You need to keep the tampon in place for as long as your doctor tells you. Under no circumstances should you spit it out at the first opportunity.
In the first two days, the clot filling the hole has a rich burgundy color. Under no circumstances should you touch it, let alone try to remove it. It serves as a barrier that prevents germs, bacteria and food debris from entering an unhealed wound.
Starting from the second or third day, the appearance of the clot changes. A light coating forms on its surface. Many people get scared because they think they are releasing pus. There is no need to worry - this is a normal process. The change in the shade of the socket is associated with the formation of new protective epithelial tissue, the basis of which is fibrin protein.
Gradually, the clot dissolves on its own and disappears. A healthy pink mucous membrane is found underneath. This indicates that regeneration was completed successfully.
Recommendations after tooth extraction
There are recommendations that, if followed, significantly speed up the gum healing process. Not only the speed of wound healing depends on them, but also the absence of possible complications. The doctor’s main recommendations in the postoperative period may be the following:
- you need to avoid foods that are too hot, spicy, or irritating to gum tissue;
- in the first days you need to carefully avoid damaging the clot; It is necessary to be extremely careful in maintaining oral hygiene;
- about 3 hours after the tooth extraction procedure you need to refrain from eating;
- in the next three days you need to eat only soft food, without consuming sweets, alcohol, or hot drinks;
- on the first day after the procedure, it is recommended to sleep on a high pillow;
- During the week, it is recommended to avoid visiting the sauna, solarium, sunbathing on the beach, and reduce physical activity;
- on the first day, it is forbidden to brush your teeth to avoid damaging the blood clot;
- Do not try to pick the clot with your finger, toothpick or tongue;
- a cold compress should be applied to the surgical area for 20 minutes, every 2 hours;
- It is recommended to use oral baths and then rinse with antiseptic agents.
The postoperative period requires careful attention to the patient's health status. A complication resulting from neglect of the rules will require much more time, money and effort to heal the wound.
What to do before deleting the eight
There are a number of rules to make surgery safer and reduce the risk of postoperative complications. Among them:
- Eat one to three hours before visiting the dentist (but if general anesthesia is planned, you cannot eat!). A preliminary meal before extraction, performed under local anesthesia, promotes better blood clotting and improves the patient’s physical condition.
- Carry out removal in the first half of the day (preferably in the morning). In the morning hours, the human body copes better with stressful situations. In addition, if the procedure is scheduled for the evening, the patient may experience insomnia due to persistent pain and nervous tension.
- Do not drink alcoholic beverages on the eve of surgery. They negatively affect the rheological properties of blood, which means that the risk of swelling and bleeding will increase.
- In case of severe anxiety, take a sedative of herbal origin. It is important that the person is not allergic to the drug used.
To remove the figure eight, you need to choose a clinic and a dental surgeon whose reputation is beyond doubt. Then the patient will be able to relax better, which means the procedure will be more comfortable.
Doctors providing this service
Modern surgical dentistry makes it possible to avoid tooth extraction in most cases, but tooth extraction is still sometimes necessary.
An operation to remove a tooth should be performed only as a last resort, when other methods to save the tooth are no longer possible or when the tooth may cause other, more serious complications.
Indications for tooth extraction
A fairly common indication for tooth extraction is the need to sanitation the oral cavity in the presence of chronic periodontitis in the acute stage, when it is impossible to eliminate the inflammatory focus at the apex of the tooth.
In some cases, tooth extraction is performed to avoid more serious complications. For example, if you have teeth that can cause a cyst, inflammation or neuritis of the trigeminal nerve. If a tooth constantly injures the tongue or the mucous membrane of the cheek, and also interferes with a normal bite, it is also better to remove such a tooth. Multi-rooted teeth, which are the cause of odontogenic osteomyelitis, are removed. When fitting a removable denture, sometimes it becomes necessary to remove teeth, but there must be strict indications for this.
Surgical operations to remove a tooth are performed under effective anesthesia, taking into account all contraindications.
Teeth are removed when they are severely damaged by caries, affected by advanced periodontal disease (“sick gums”), have been broken so that they can no longer be restored, are incorrectly positioned in the mouth (for example, an embedded wisdom tooth), or in preparation for orthodontic treatment.
Before starting tooth extraction, the dentist examines the oral cavity, takes x-rays of diseased teeth, and evaluates their condition.
After a tooth is removed, the teeth adjacent to it begin to gradually shift, sometimes quite significantly, and this can greatly affect the general condition of the teeth. Removing even a single tooth can create serious chewing problems. To avoid these complications, the dentist will recommend replacing the extracted tooth with an artificial one.
Considering all the advances in operative surgery today, most patients prefer to replace the existing dentition defect by placing a dental implant (advantages of using dental implants), dental bridges or removable partial dentures.
Wisdom teeth removal
The removal of wisdom teeth is due to slightly different reasons. Naturally, the above reasons for tooth removal also apply to the removal of wisdom teeth, however, this case has its own characteristics.
Problems with wisdom teeth often arise as soon as they erupt. They erupt at the age of 18-25 years (sometimes much later), when the dentition is formed by 28 teeth, which leads to incorrect placement of wisdom teeth in the dentition (the lower wisdom teeth are more often displaced), immersion (incomplete eruption with a tilt in the vertical, horizontal, distal or medial direction). In addition, misaligned wisdom teeth can cause damage to adjacent teeth, putting pressure on them and causing root damage and resorption, as well as displacement and malocclusion.
There are no dental rules determining the most acceptable age for wisdom tooth removal. However, practice shows that the sooner you get rid of these teeth, the fewer complications you can expect from them in the future.
If the wisdom tooth is in the wrong position or has not fully erupted, this leads to pericoronitis (inflammation of the tissues surrounding the tooth), because Part of the tooth is located under the gum and food debris accumulates in the gum pocket, which is an excellent breeding ground for various microorganisms. Wisdom teeth are often affected by caries, because... Between it and the second molar, food debris also accumulates and plaque forms due to the fact that this space is difficult to clean with a toothbrush. In this case, caries affects not only the wisdom tooth, but also the second molar adjacent to it.
- refrain from eating for 2-3 hours after removal;
- do not drink alcohol or take a sauna on the day of surgery;
- do not touch the hole with your tongue or any objects;
- do not eat hot food;
- do not rinse your mouth.
How to properly care for your gums
To prevent complications from occurring, you should follow a few simple recommendations:
- Do not heat the gum. Strong heat can stimulate the spread of the inflammatory process.
- Use a soft brush. At the same time, when brushing your teeth, try not to touch the gums at the extraction site.
- Use additional cleaning products. These include irrigators and dental floss.
- Try to use toothpastes with soothing herbal ingredients.
It is very important not to self-medicate. If any problem arises, you should consult a doctor as soon as possible.
What can you do at home -
After the acute symptoms of inflammation have subsided, there is no need for antiseptic turundas inside the socket, because they do not help the wound to heal (epithelialize) faster. At this stage, the best treatment method will be to fill the hole with a special Dental adhesive paste (Solcoseryl). This drug has an excellent analgesic effect (after 2-3 hours the pain will practically stop, and after 1-2 days it will go away completely), and also speeds up healing many times over.
Scheme of use - this paste is added to a hole that has been washed with an antiseptic and slightly dried with a dry gauze swab (completely filling the hole). The paste is perfectly fixed in the hole and does not fall out of it. There is no need to remove the paste from the hole, because... it slowly dissolves on its own, giving way to growing gum tissue. The only thing that may be required is to periodically add it to the hole.
How to rinse the hole from food debris -
In some situations (when the turunda has fallen out of the hole, and there is no way to see a doctor right away), it may be necessary to wash the hole. After all, after each meal, the hole will become clogged with food debris, which will cause new inflammation. Rinsing will not help here, but you can easily rinse the hole with a syringe.
Important : from the very beginning you must bite off the sharp edge of the needle from the syringe! Next, bend the needle a little and fill a 5.0 ml syringe with a solution of Chlorhexidine 0.12-0.2% (it is sold ready-made in every pharmacy for 20-30 rubles). Screw the needle tightly so that it does not fly off when pressing the syringe plunger! Place the blunt end of a bent needle into the upper part of the socket (do not insert too deeply to avoid injuring the tissue), and rinse the socket under pressure. If necessary, do this after every meal.
In principle, after this the hole can be dried with a gauze swab and treated with Solcoseryl. We hope that our article on the topic: Alveolitis after tooth extraction, symptoms, treatment - turned out to be useful to you!
Sources:
1. Higher prof. the author’s education in surgical dentistry, 2. Based on personal experience as a dental surgeon, 3. National Library of Medicine (USA), 4. “Outpatient surgical dentistry” (Bezrukov V.), 5. “Propaedeutics of surgical dentistry” (Soloviev M. .).
How to remove a tooth
There are two extraction methods used in dentistry: simple and complex. Their choice depends on which teeth are being removed - premolars and molars with tangled branched roots are removed using a complex method. It is very difficult to pull out such elements entirely due to the fact that the tooth socket is penetrated by retaining ligaments and alveolar processes. Errors during the procedure or insufficient experience of the specialist lead to serious complications. Therefore, even despite the acute condition, always find out in advance where you can have a tooth removed from a good doctor with positive recommendations.
Factors complicating the operation:
- complete destruction of the coronal part;
- high fragility;
- acute inflammatory diseases;
- Unerupted or misaligned wisdom teeth.
The technology of the procedure depends on which teeth are removed. In some cases, tissue incision and suturing are performed.