What are “tooth surfaces”?
Now you can almost accurately determine the cost of your future treatment without leaving your home. You just need to visually examine which surfaces the caries has spread to. The exception is hidden carious cavities that cannot be seen.
1. Treatment of one tooth surface (except contact surfaces)
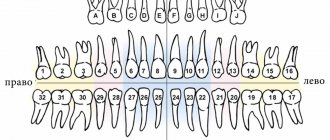
This position means that the indicated price applies to the treatment of any caries (superficial, medium or deep) located on any* one(!) of the tooth surfaces: chewing, vestibular (the surface of the tooth that comes into contact with the cheek or lip), lingual (for teeth of the lower jaw), palatal (for the teeth of the upper jaw). The lingual and palatal surfaces of the tooth “look” into the oral cavity and can be touched with the tongue when the dentition is closed. * The cost of treating the contact surface of the tooth, despite the fact that it is one surface, is not included in this position, since it requires more complex treatment with the restoration of close contact with the adjacent tooth. The contact surface of a tooth is any surface of a tooth that makes contact between a tooth and an adjacent tooth on the same jaw. Typically, a tooth has two such surfaces: medial and distal. The mesial surface of the tooth is in contact with the tooth in front, and the distal surface with the tooth behind in the dentition. It is to clean these surfaces that we use dental floss or floss.
2. Treatment of caries on two tooth surfaces or 1st contact surface
This item indicates the cost of treating any caries that affects one contact surface of a tooth or any two surfaces of a tooth (including two contact surfaces). Most often, caries occurs on contact surfaces, since many do not use dental floss and the surfaces remain uncleaned.
3. Treatment of caries on three tooth surfaces
This item indicates the cost of treating any caries that affects any three tooth surfaces at once.
4. Temporary restoration with composite materials of a tooth with destruction of more than ½ of the surface
This item indicates the cost of restoring the crown of a tooth with destruction or carious lesions on four or five tooth surfaces at once. Such a restoration is called “temporary”, since with such tooth destruction there are direct indications for an orthopedic structure - a crown, in order to preserve the tooth from further destruction: breaking the remaining wall or cracking the tooth, which may lead to tooth extraction. Temporary restoration is done if the patient is not ready for prosthetics in the near future for one reason or another.
Crown of the tooth
The crown of a tooth (lat. corona dentis) is the part of the tooth protruding above the gum. The crown is covered with enamel - hard tissue, 95% consisting of inorganic substances and subject to the most powerful mechanical stress. There is a cavity in the crown of the tooth - dentin (hard tissue 2-6 mm thick) comes closer to the surface, then pulp, which fills both part of the crown and the root part of the tooth. The pulp contains the blood vessels and nerves of the tooth. Teeth cleaning and removal of dental deposits are carried out specifically from the crowns of the teeth.
Tooth neck
The neck of the tooth (lat. collum dentis) is the part of the tooth between the crown and root, covered by the gum.
Tooth roots
The root of the tooth (lat. radix dentis) is the part of the tooth located in the dental alveolus.
Fissure
On the chewing surface of the back teeth, between the cusps of the teeth there are grooves and grooves - fissures. The fissures can be narrow and very deep. The relief of the fissures is individual for each of us, but dental plaque gets stuck in the fissures of everyone. It is almost impossible to clean the fissures with a toothbrush. Bacteria in the oral cavity, processing plaque, form acid, which dissolves tooth tissue, forming caries. Even good oral hygiene is sometimes not enough. In this regard, fissure sealing has been successfully used throughout the world for 20 years.
Tooth enamel
Tooth enamel (or simply enamel, Latin enamelum) is the outer protective shell of the crown part of human teeth. Enamel is the hardest tissue in the human body, which is explained by the high content of inorganic substances - up to 97%. There is less water in tooth enamel than in other organs, 2-3%. Hardness reaches 397.6 kg/mm? (250-800 Vickers). The thickness of the enamel layer differs in different areas of the crown of the tooth and can reach 2.0 mm, and disappears at the neck of the tooth. Proper care of tooth enamel is one of the key aspects of human personal hygiene.
Dentine
Dentin (dentinum, LNH; lat. dens, dentis - tooth) is the hard tissue of the tooth, constituting its main part. The coronal part is covered with enamel, the root part of the dentin is covered with cement. Consists of 72% inorganic substances and 28% organic substances. Consists mainly of hydroxyapatite (70% by weight), organic material (20%) and water (10%), permeated with dentinal tubules and collagen fibers. Serves as the foundation of the tooth and supports tooth enamel. The thickness of the dentin layer ranges from 2 to 6 mm. Dentin hardness reaches 58.9 kgf/mm?. There are peripulpal (internal) and mantle (external) dentin. In peripulpal dentin, collagen fibers are located predominantly condensally and are called Ebner fibers. In mantle dentin, collagen fibers are arranged radially and are called Korff fibers. Dentin is divided into primary, secondary (replacement) and tertiary (irregular). Primary dentin is formed during the development of the tooth, before its eruption. Secondary (replacement) dentin is formed throughout a person’s life. It differs from the primary by a slower pace of development, a less systemic arrangement of dentinal tubules, a larger number of erythroglobular spaces, a larger amount of organic substances, higher permeability and less mineralization. Tertiary dentin (irregular) is formed during tooth trauma, tooth preparation, caries and other pathological processes, as a response to external irritation.
Dental pulp
Pulp (lat. pulpis dentis) is loose fibrous connective tissue that fills the tooth cavity, with a large number of nerve endings, blood and lymphatic vessels. Along the periphery of the pulp, odontoblasts are located in several layers, the processes of which are located in the dentinal tubules throughout the entire thickness of the dentin, performing a trophic function. The processes of odontoblasts include nerve formations that conduct pain sensations during mechanical, physical and chemical influences on dentin. Blood circulation and innervation of the pulp are carried out thanks to dental arterioles and venules, the nerve branches of the corresponding arteries and nerves of the jaws. Penetrating into the dental cavity through the apical opening of the tooth root canal, the neurovascular bundle breaks up into smaller branches of capillaries and nerves. The pulp helps stimulate regenerative processes, which manifest themselves in the formation of replacement dentin during the carious process. In addition, the pulp is a biological barrier that prevents the penetration of microorganisms from the carious cavity through the root canal beyond the tooth into the periodontium. The nerve formations of the pulp regulate the nutrition of the tooth, as well as the tooth’s perception of various irritations, including pain. The narrow apical opening and the abundance of vessels and nerve formations contribute to the rapid increase in inflammatory edema in acute pulpitis and compression of the nerve formations by the edema, which causes severe pain.
Tooth cavity
(lat. cavitas dentis) The space inside the tooth formed from the cavity of the crown and root canals. This cavity is filled with pulp.
Cavity of the tooth crown
(lat. cavitas coronae) Part of the tooth cavity, located under the crown and repeating its internal contours.
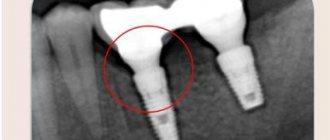
Tooth root canals
The root canal of a tooth (lat. canalis radicis dentis) is an anatomical space inside the root of a tooth. This natural space within the coronal part of the tooth consists of a pulp chamber, which is connected by one or more main canals, as well as more complex anatomical branches that can connect the root canals to each other or to the surface of the tooth root.
Nerves
(lat. nervae) Neuron processes passing through the apex of the tooth and filling its pulp. The nerves regulate the nutrition of the tooth and conduct pain impulses.
Arteries
(lat. arteriae) Blood vessels through which blood from the heart flows to all other organs, in this case - to the pulp of the tooth. Arteries nourish dental tissues.
Vienna
(lat. venae) Blood vessels through which blood returns from organs back to the heart. The veins enter the canals and penetrate the pulp of the tooth.
Cement
Cement (lat. - cementum) is a specific bone tissue that covers the root and neck of a human tooth, as well as the teeth of other mammals. Serves to firmly secure the tooth in the bone alveolus. Cement consists of 68-70% inorganic components and 30-32% organic substances. Cementum is divided into acellular (primary) and cellular (secondary). Primary cement is adjacent to the dentin and covers the lateral surfaces of the root. Secondary cement covers the apical third of the root and the bifurcation area of multi-rooted teeth.
Tops of tooth roots
(lat. apex radicis dentis) The lowest points of the teeth, located on their roots. At the tops there are openings through which nerve and vascular fibers pass to the tooth.
Apical foramina
(lat. foramen apices dentis) Places of entry of vascular and nerve plexuses into the dental canals. The apical foramina are located at the apex of the tooth roots.
Alveolus (alveolar socket)
(alveolar socket) (lat. alveolus dentalis) A notch in the jaw bone into which the roots of the tooth enter. The walls of the alveoli form strong bone plates impregnated with mineral salts and organic substances.
Alveolar neurovascular bundle
(lat. aa., vv. et nn alveolares) A plexus of blood vessels and nerve processes passing under the alveolus of the tooth. The alveolar neurovascular bundle is enclosed in an elastic tube.
Periodontium
Periodontium (lat. Periodontium) is a complex of tissues located in the slit-like space between the cementum of the tooth root and the alveolar plate. Its average width is 0.20-0.25 mm. The narrowest section of the periodontium is located in the middle part of the tooth root, and in the apical and marginal sections its width is slightly greater. The development of periodontal tissue is closely related to embryogenesis and teething. The process begins in parallel with the formation of the tooth root. The growth of periodontal fibers occurs both from the side of the root cement and from the side of the alveolar bone, towards each other. From the very beginning of their development, the fibers have an oblique course and are located at an angle to the tissues of the alveoli and cementum. The final development of the periodontal complex occurs after tooth eruption. At the same time, the periodontal tissues themselves are involved in this process. It should be noted that, despite the mesodermal origin of the constituent components of the periodontium, the ectodermal epithelial root sheath takes part in its normal formation.
Gingival grooves
(lat. sulcus gingivalis) Crevices that form where the crown of the tooth adheres to the gums. The gingival grooves run along the line between the free and attached parts of the gum.
Gum
Gums (lat. Gingiva) is a mucous membrane that covers the alveolar process of the upper jaw and the alveolar part of the lower jaw and covers the teeth in the cervical area. From a clinical and physiological point of view, the gums are divided into interdental (gingival) papilla, marginal gum or gingival margin (free part), alveolar gum (attached part), mobile gum. Histologically, the gum consists of stratified squamous epithelium and the lamina propria. There are oral epithelium, junctional epithelium, and sulcal epithelium. The epithelium of the interdental papillae and attached gingiva is thicker and can become keratinized. In this layer, there are basal, spinous, granular and stratum corneum. The basal layer consists of cylindrical cells, the spinous layer consists of polygonal cells, the granular layer consists of flattened cells, and the stratum corneum is represented by several rows of completely keratinized and nucleated cells that are constantly exfoliated.
Mucous papillae
(lat. papilla gingivalis) Fragments of gums located at their elevation in the area between adjacent teeth. The gingival papillae are in contact with the surface of the dental crowns.
Jaws
(lat. maxilla - upper jaw, mandibula - lower jaw) Bony structures that are the basis of the face and the largest bones of the skull. The jaws form the mouth opening and determine the shape of the face.
Prevention of wear of hard dental tissues
For the purpose of prevention, it is necessary to identify and eliminate risk factors that are important in the occurrence of tooth wear. These include the patient's use of highly abrasive hygiene products, frequent consumption of drinks and foods with low pH, eating disorders, bruxism, disorders of occlusal relationships, and somatic pathology.
Basic strategies for preventing wear of hard dental tissues, based on the main risk factors:
1. A balanced diet with minimizing the consumption of foods and drinks with low pH.
Careful assessment of dietary habits is important in assessing the erosive potential of a diet. The patient should be familiarized with a list of foods with low pH (salad dressings, vinegar, alcoholic beverages, carbonated soft drinks, herbal teas, fruit juices). The patient is advised to keep a food diary for at least 4 days, including weekends. Identification of consumption of foods and drinks with low pH in any combination more than 4 times [17] per day allows the patient to be classified as at risk of dental erosion.
2. Control of hygiene skills and informed choice of hygiene products.
Scientists assign the leading role in the erosive and abrasive wear of tooth tissue to mechanical factors: the active use of certain abrasive hygiene products, irrational brushing of teeth [18-21].
Patients at risk (gastrointestinal diseases, eating disorders, hazardous occupations, bruxism, etc.) should use toothpastes with a low degree of abrasiveness (RDA index = 30-50) and a soft toothbrush. It is not recommended to cleanse immediately after consuming fruits and drinks with low pH, vomiting, regurgitation or reflux.
To prevent erosion, at least 1 hour should pass between meals or drinks.
3. Strengthening hard tissues and normalizing saliva function. Strengthening hard tissues is possible due to fluorides and calcium phosphate technologies.
Scientists have recognized effective technologies for increasing the acid resistance of hard dental tissues using fluoride-containing preparations [22]. When exposed to erosion, there is no need for remineralization of the subsurface layer. The main thing is to strengthen the thin surface layer. Therefore, when treating erosions, high concentration fluoride applications are a more appropriate application. Fluoride gels provide good protection for eroded enamel from the abrasive action of a toothbrush.
The use of bicarbonate-containing toothpastes is one of the ways to introduce buffering agents into the oral cavity [23]. It is recommended to apply alkaline pastes or gels before bed to protect teeth from erosion due to reflux that occurs during sleep.
Adding calcium and phosphate to sour drinks can significantly reduce their erosive potential. Juices and carbonated drinks containing calcium and phosphates have appeared on sale.
Measures to increase the secretion of stimulated saliva, such as chewing sugar-free gum, are accordingly anti-erosive and support remineralization.
4. Referral to related specialists for timely detection and treatment of somatic pathology (endocrine pathology, hormonal disorders, gastrointestinal diseases, serious eating disorders: anorexia, bulimia, bruxism).
The appearance of tooth wear may be associated with endocrine pathology, disorders of hormonal and mineral homeostasis. Yu. M. Maksimovsky (1981) assigns an important role in the development of erosions to hyperfunction of the thyroid gland. Dental erosions in patients with thyrotoxicosis were detected twice as often as in persons with normal thyroid function; a direct connection was established between the intensity of dental damage and the duration of thyrotoxicosis {24}. In women, dental erosions are detected in a higher percentage of cases {25}. Examination of patients with non-carious lesions of teeth should be carried out jointly with a gynecologist and endocrinologist. The examination algorithm by related specialists includes hormonal indicators (estradiol, TSH, prolactin, cortisol).
If gastroesophageal reflux is suspected, patients need a referral to a physician or gastroenterologist. The dentist should be alerted to erosions on the oral surface of the chewing group of the teeth of the upper jaw and the patient’s specific complaints (sour taste in the mouth, halitosis, increased salivation, permanent cough, stomach pain, feeling of a “lump” in the throat, burning sensation, hoarseness, belching, heartburn) . Patients with a history of asymptomatic gastroesophageal reflux report wet spots on the pillow and a sour taste in the mouth after sleep.
Eating disorders include three main diagnoses [26]: anorexia, bulimia, and other unspecified eating disorders (a combination of several disorders). Anorexia is characterized by a conscious refusal to eat, a prolonged lack of appetite, and the disappearance of the basic instinct - hunger; bulimia - uncontrolled eating of large portions of food, followed by spontaneous vomiting.
Early detection of eating disorders is important for the outcome of the disease, secondary prevention, prevention of complications and reduction of harmful consequences in relation to the dental health and general somatic status of the patient. Patients with eating disorders often avoid medical professionals, and if they do, they hide the true origin of the problem. Therefore, knowledge of the manifestations of these disorders in the oral cavity is extremely important for the dentist.
Aesthetic restoration of teeth with a combination of carious lesions and increased abrasion
Modern advances in the development of dental materials significantly expand the capabilities of dentists. Recognition of aesthetic dentistry as a separate area with its own theoretical, scientific and practical developments has ensured the rapid implementation of advanced treatment methods. Routine “filling” is being replaced by restoration, which guarantees high quality restoration of teeth with defects of carious and non-carious origin.
Moreover, it has become possible to treat combined lesions using methods that require minimal excision of hard tooth tissue and ensure preservation of pulp vitality.
Such work is based on the principles of aesthetic dentistry (I.K. Lutskaya, 2011) [2].
The main principle, or starting point, of aesthetic dentistry should be the achievement of treatment results that are as close as possible to the natural parameters of the dentition.
Thus, therapeutic restorations and orthopedic structures are subject to the requirement of maximum similarity with the optimal characteristics of teeth in color, shape, and relief.
Surgical crown lengthening or gingivectomy should not visually increase the original size of the teeth, cause gum recession or “gaping” of interdental spaces [4].
Achievement of the basic principle is ensured through optimal therapeutic effects, which involves the selection of means and methods that do not violate or minimally damage intact structures. First of all, the methods of bleaching, then minimal preparation (microabrasion), and grinding of the non-prismatic enamel layer are considered as therapeutic methods. Preparation, and especially depulpation, is carried out strictly according to indications. Any manipulations must ensure high aesthetics, mechanical strength, and reliable adhesion of restorations to tooth tissues [4].
The principle of conscious cooperation implies that the patient conscientiously and regularly performs the procedures prescribed by the dentist.
Thus, home whitening is prescribed by a doctor and performed by the patient independently, strictly following the instructions. The choice of shades of color, size and shape of the structure is carried out jointly by the dentist and the patient to reach consensus. The scope of surgical intervention is also carried out after obtaining the informed consent of the patient.
Working with photocomposites and modern ceramics has its own fundamental requirements, approaches, and principles that provide scientific validity to the manipulations performed.
The principle of color imitation ensures the modeling of a restoration (structure) with high aesthetic parameters, implying the selection of shades of material that correspond in optical properties to dentin and enamel, followed by imitation of the color of lost tooth tissues [5].
The principle of reproducing natural volumetric parameters implies preliminary planning of the dimensions, shapes, and surface relief of the restoration (structure), followed by the reconstruction of macro- and microstructures [1].
When modeling a restoration, its morphological features must repeat the parameters of an intact tooth, therefore it is necessary to maintain the geometric shape, signs of belonging to the side, and mamelons.
Such large structural elements are modeled with opaque materials.
Individual characteristics, such as surface relief, cutting edge shape, and transparency, are formed using enamel shades in compliance with the rule of preserving the volume of natural tissue.
The principle of adhesive preparation (English: prepare) means increasing the area of contact between the filling and the tooth in order to ensure high-quality bonding of the composite with the dental tissues. The objectives are achieved by excision of hard tissue to intact structures, creating a bevel of the enamel or giving the cavity a certain shape, as well as acid etching and the use of an adhesive system.
The principle of minimizing the effects of polymerization shrinkage is based on the property of the material to decrease in volume during the curing process.
At the stage of tooth preparation, reducing the effects of shrinkage is achieved by excision of thinned protrusions and rounding of the internal corners of the cavity. The absence of a complex design reduces tension in the tooth tissues. The risk of detachment of the filling, the formation of a gap at the border with the tooth, and the appearance of hyperesthesia is reduced when using gaskets made of chemically cured materials: during polymerization, they are “attracted” towards the heat source - the pulp.
During the curing process of a composite, one of the methods for reducing shrinkage is the “soft start” method: reducing the exposure time of the first stage of photopolymerization.
Knowledge of the principles of aesthetic dentistry allows you to choose the most correct methods of influence, ensuring maximum efficiency.
Clinical case
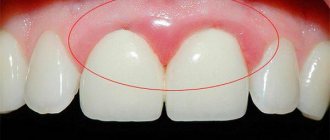
The patient, 35 years old, complained of aesthetic defects of the upper central incisors. Carious cavities are localized on the mesial surfaces of the 11th and 21st teeth. There is a significant decrease in the height of the crowns of the upper central incisors due to increased uneven abrasion of hard tissues (Fig. 1).
Rice. 1. Carious cavities on the mesial surface of teeth 1.1 and 2.1, uneven wear of hard tissues.
The use of composite material for dental restoration involves the following sequence of stages: mechanical cleaning of the tooth surface; choice of photopolymer shades; planning the size and shape of restorations; tooth preparation; use of an adhesive system; filling the defect with a composite; polymerization; coating of teeth with fluoride varnish.
Taking into account the complexity of the work and aesthetic requirements, a nanohybrid composite is used for dental restoration, representing a new class of filling materials characterized by high aesthetic properties: Grandio SO (VOCO). It combines the qualities of photopolymer with the innovation of nanotechnology. For its production, polymer resins with high molecular weight and microfillers with an average particle size of 20-30 microns were used.
Combining nanomers (zirconium silicate particles less than 100 nm in size) with glass-ceramic composite particles made it possible to increase the share of filler in the material to 87%, which reduced the content of organic resins in the matrix and, accordingly, reduced polymerization shrinkage to 1.57%. Filling the material with nanoparticles ensures high marginal stability, easy polishability and good color fastness of the restoration. Thanks to good adaptation to enamel and dentin shades, the so-called chameleon property, the stage of selecting composite shades is greatly simplified. In some cases, one shade of material from one color group (for example, red-brown, group A) of varying degrees of transparency (opaque, enamel, transparent) can be used. In more complex clinical situations, 2-3 syringes with different color characteristics will be required.
Nanocomposites are indicated for filling cavities of classes I-V according to Black, restoring teeth with traumatic injuries and hard tissue defects of non-carious origin. A large selection of shades and color stability of the nanomaterial allow it to be used for aesthetic filling of anterior teeth with correction of shape and color; restore teeth with class II cavities of significant size; used for splinting, making inlays, onlays, adhesive prostheses, restoring the tooth stump for a crown.
The first stage is the mechanical treatment of teeth with fluoride-free paste (Fig. 2). Cleaned surfaces are washed with a stream of water.
Rice. 2. Cleaning teeth from plaque.
The shades of the photopolymer are selected in natural light (the patient is in a sitting position) using the colors supplied with the material (Fig. 3).
Rice. 3. Selection of shades of tooth color.
The surfaces of the teeth are kept moist, which preserves their natural appearance. The opaque composite OA 2 is selected to match the color of the central area, this will avoid the transparency of the filling. To create a natural look, shine and transparency, enamel shades of the restoration are used, which are selected separately for the central (A 2) and proximal sections (A 2 and I), and the incisal edge (A 1 and I). Using opaque alone can create the appearance of a flat or lifeless tooth. The absence of opaque will make the restoration “transparent”. Enamel and clear shades are required to cover the main area of the restoration, the incisal edge and proximal surfaces. A transparent cutting edge with a width of more than 1 mm is assumed.
When choosing tooth shades, the phenomenon of irradiation is taken into account - a change in the size of the surface depending on color and lightness, when warm light colors (yellowish) create the illusion of convexity, and cool colors (blue) create depressions. As a result, the cutting edge of light yellow shades will be perceived as voluminous, while the bluish edge will be perceived as flat and displaced orally. In this case, it is planned to use 4 syringes of composite material: opaque OA 2, enamel A2 and A1, transparent I.
Planning the size, shape and relief is a strictly defined sequence of actions describing the specific anatomical formation of the tooth.
Teeth are measured with a micrometer. The height of the clinical crown of the central incisors is defined as the distance from the marginal level of the gums along the vertical midline to the conventional line of the cutting edge, overlapping the occlusal surface of the lower incisors by 1.5 mm.
Mesiodistal dimensions in the neck area are measured by the distance between two points at the level of the apexes of the interdental papillae, in the equator area - at the level of the middle third of the crown height, in the incisal edge area they are assessed by the distance between the protruding points of the mesial and distal edges of the crown. In this case, odontometry indicates that the width of the tooth in the equatorial region is equal to the height of the tooth and is 8.9 mm in the 11th tooth, 9.0 mm in the 21st tooth.
In the area of the cutting edge, it is not possible to measure the horizontal size of the tooth, since it is erased. The map indicates signs of belonging to a party. The sign of crown curvature is weakly expressed. Due to chipping and increased wear of teeth, the dimensions of the mesial angle are not determined. Based on visual assessment and measurement results, it is planned to change the square geometric shape of the crowns to rectangular by increasing the vertical size by lengthening the cutting edge. The planned vertical dimensions of the incisors are 9.7 mm for the right incisor and 9.8 mm for the left (the height of the teeth differs due to the higher dome of the gingival margin in tooth 21) (Fig. 4).
Rice. 4. Odontometry: tooth width in the equatorial region in 1.1 teeth is 8.9 mm, in 2.1 teeth 9.0 mm. The planned tooth height is 9.7 mm for the right incisor and 9.8 mm for the left.
It is planned to recreate the predominance of the distal angle of the crown over the mesial angle, which is a sign that the tooth belongs to a certain side. The sign of crown curvature is not pronounced: the mesial surfaces have a slight oral location compared to the distal ones, they have a penumbra, and are visually perceived as darker. It is intended to create a slight convexity of the vestibular surface closer to the mesial edge. The individual characteristics of teeth are smooth vestibular surfaces. The length of the contact points between the teeth is planned in such a way that there is enough space for the interdental papilla (from the top of the gingival papilla to the incisal edge). The cutting edge of the teeth is smooth.
To prevent chipping of the filling material, occlusal contacts and the incisal path are aligned using carbon paper.
Teeth preparation is carried out with diamond burs and begins with a thorough necrotomy of the walls and bottom of the carious cavity. In this case, diamond burs (NTI company) are used to process the enamel, first with medium (100 microns), then with fine grain (40-50 microns). The water jet is applied continuously to the drill to avoid irritation of the pulp. Dentin is prepared with carbide burs. The vestibular wall of the carious cavity is partially excised, since it is represented by a thin layer of enamel that does not have underlying dentin. As a result, class IV cavities are formed (Fig. 5).
Rice. 5. Teeth after necrectomy.
All corners are rounded with a spherical bur. On the vestibular surface of each incisor, an enamel bevel approximately 3.5-4.0 mm wide is made in order to recreate the sign of crown curvature and move the convexity of the vestibular surface closer to the mesial edge. The surface is smoothed with a fine-grained diamond bur (40-50 microns). Bevels will ensure an increase in the contact area between the tooth and the composite, as well as the aesthetics of restorations due to a smooth transition of the material at the filling-tooth interface. On the palatal surface, the enamel is ground at an angle of 45°.
The prepared surfaces are thoroughly washed with a stream of water and dried with an air stream. The dentin is covered with glass ionomer cement. Then the enamel is covered with etching gel (30 sec.) (Fig. 6).
Rice. 6. Acid etching of enamel.
After time, the gel is thoroughly washed off, and the enamel surface is dried with a stream of air (Fig. 7). The adhesive is evenly applied to the prepared surfaces, rubbed in with a brush, left for 30 seconds to soak, distributed with a gentle stream of air and polymerized for 20 seconds.
Rice. 7. Central incisors after the acid etching stage.
Filling begins with filling the cavity. The opaque composite (OA 2) is introduced into the cavity in a layer of no more than 2.0 mm in thickness, carefully pressed against the bottom and walls, and photopolymerized for 30 seconds.
The adaptation of the material in the area of the missing vestibular wall of the cavity requires special attention: the level of the opaque layer is located 1.0-1.5 mm below the level of the tooth surface (the difference will allow the formation of the enamel layer) (Fig. 8).
Rice. 8. Adaptation of the opaque layer of the Grandio SO (VOCO) material.
After filling the carious cavity, they begin modeling the half-veneer, which is carried out in compliance with a gradual transition from recreating large details (the geometric shape of the vestibular surface) to reproducing medium ones (signs of the angle and curvature of the crown), and then to modeling smaller elements (the area of the cutting edge). Each subsequent layer is applied on top of the previous one and distributed in different directions using a wide trowel or spatula. The boundary of each layer is created in the form of buoyant waves (Fig. 9).
Rice. 9. The enamel shade of the composite is distributed.
The mesial surface is modeled with an opaque composite throughout the middle and lower tier of the tooth crown. The main landmark is the border of the transparent tooth enamel: in this case, there is about 1.0 mm of free space around the entire perimeter of the tooth, except for the cutting edge, where the width of the transparent layer will be 1.5 mm.
To recreate the sign of crown curvature, a portion of opaque photopolymer is applied in the form of a vertical roller at the border of the mesial and median sections, and then smoothed so that the maximum convexity is maintained closer to the mesial surface (Fig. 10).
Rice. 10. Scheme for modeling the sign of crown curvature.
Modeling of the sign of the crown angle is carried out in the lower tier of the tooth, taking into account the degree of its severity: the distal angle is larger in size than the mesial one. In this case, the latter is modeled in the area of the mesial lower third of the tooth crown, with the filling material distributed towards the cutting edge and mesial contour and giving the corner the desired shape (Fig. 11).
Rice. 11. Modeling the crown angle sign.
The vestibular surface is covered with a thin layer of enamel (A 2) and then transparent (I) photopolymer. Modeling of the side surfaces is also completed with enamel (A 1) and transparent composite, which is distributed taking into account the individual degree of transparency of the enamel: evenly along the entire perimeter of the restoration. At the cutting edge, the width of the transparent layer is 1.0 mm (Fig. 12).
Rice. 12. Imitation of a translucent cutting edge.
Immediately after the production of aesthetic structures, they are processed: the surface hybrid layer is removed (with bur No. H390S-018-FG, NTI) (Fig. 13), the relief is contoured, and occlusal contacts with antagonist teeth are verified.
Rice. 13. Contouring of aesthetic restorations.
Polishing is carried out with discs without significant pressure on the surface of the restoration, in the direction from the equator towards the cutting edge. To achieve shine, polishing heads containing fine aluminum oxide powder as an abrasive are used, sponges and polishing pastes are used (Fig. 14).
Rice. 14. Polishing the surface of the restoration.
At the final stage, odontometry is carried out: the vertical size of the teeth after restoration exceeds the horizontal ones and amounts to 9.7 mm and 9.8 mm for the right and left incisors, respectively, the teeth have acquired a rectangular shape (Fig. 15).
Rice. 15. Final odontometry: vertical tooth size 9.7 mm and 9.8 mm for the right and left incisors, respectively.
Finishing of proximal surfaces is carried out with strips - strips on a metal or plastic base with varying degrees of granularity of the abrasive material applied to them. The finished work is shown in Figure 16.
Rice. 16. General view of the finished restoration.
Illumination of teeth with short-wave light demonstrates the same spectral composition and fluorescence intensity of the filling material from which the half-veneers are made and the hard tissues of the tooth (Fig. 17).
Rice. 17. When illuminated with short-wavelength light, the restorations fluoresce in the same way as the hard tissues of the tooth.
The final stage of treatment is the treatment of the enamel surrounding the restoration with fluoride-containing preparations.
Quality assessment is carried out in accordance with the aesthetic quality index (EQI) [3]. The score is given separately for each of the 12 parameters presented in the table: 3 points - the result fully corresponds to the plan; 2 points - the result partially corresponds to the plan; 1 point - the result does not correspond to the planned one. Then all points are summed up. The highest possible number of points is 36.
Quality rating: 33-36 points - excellent; 29-32 points - good; 24-28 points - satisfactory; below 24 points - unsatisfactory.
Calculation of the aesthetic quality index (EQI):
EIC = n/36
where n is the total score; 36 - maximum score;
0.9-1 - excellent result;
0.7-0.8 - good result, minor correction of the restoration is needed;
<0.7 - unsatisfactory result, the structure needs to be replaced.
An assessment of the aesthetic restorations we performed showed: EIC = 1, which is interpreted as an excellent treatment result.
Table No. 1. Assessment of the quality of the manufactured structure according to EIK (aesthetic quality index)
Criteria | Intact, symmetrical tooth | Design | Score in points | |
| planned | manufactured | |||
| 1 | 2 | 3 | 4 | 5 |
| 1. Tooth dimensions: height (LCO2), mm | 8.9 mm | 9.7 mm | 9.7 mm | 3 |
| transverse size (MDCO2), mm in the cervical region | 8.9 mm | 8.9 mm | 8.9 mm | 3 |
| in the equator region | 8.9 mm | 8.9 mm | 8.9 mm | |
| in the area of the cutting edge | 8.9 mm | 8.9 mm | 8.9 mm | |
| 2. Geometric tooth shape: rectangular (square) | square | rectangular | rectangular | 3 |
| triangular | ||||
| oval | ||||
| 3. Crown angle sign: expressed not expressed | not expressed | expressed | expressed | 3 |
| 4. Sign of crown curvature (displacement of the point of greatest convexity): | 3 | |||
| mesially | ||||
| closer to the midline | ||||
| displaced distally | distally | mesially | mesially | |
| absent | ||||
| 5. Sign of root deviation: expressed not expressed | expressed | expressed | expressed | 3 |
| 6. Gingival contour: flattened | 3 | |||
| rounded | ||||
| domed | domed | domed | domed | |
| 7. Cutting edge: straight | straight | straight | 3 | |
| convex | ||||
| concave | concave | |||
| serrated | ||||
| 8. Relief of the vestibular surface: expressed | ||||
| not expressed | not expressed | not expressed | not expressed | 3 |
| 9. Degree of gloss of the enamel (presence of distortions): evenly matte | 3 | |||
| “matte” in the cervical area | ||||
| brilliant | shine | shine | shine | |
| 10. Type of tooth transparency: enamel is transparent in all areas of the tooth crown | 3 | |||
| pronounced transparency of the proximal surfaces of the tooth | ||||
| Only the cutting edge is transparent | ||||
| transparent cutting edge and proximal surfaces | + | + | + | |
| 11. Tooth color assessment using the VITA scale: in the cervical region | A 2 | A 2 | A 2 | 3 |
| in the equator region | A 2 | A 2 | A 2 | |
| at the cutting edge | A 1 + I | A 1 + I | A 1 + I | |
| on proximal surfaces | A 2 + I | A 2 + I | A 2 + I | |
| 12. The presence of individual characteristics of the tooth (stains due to hypoplasia, fluorosis, etc.) | — | — | — | |
| 13. Assessment of the quality of the manufactured structure according to EIK (aesthetic quality index) | n/36 | 36/36 = 1 | ||
Conclusion
The use of photocomposites in aesthetic dentistry makes it possible to expand the indications for dental treatment using therapeutic methods. In accordance with the basic requirements for aesthetic restorations, the main stages of treatment are carried out using light-curing materials, including the selection of optimal shades, modeling of restorations, and their processing. Efficiency is assessed in accordance with the aesthetic quality index, which reflects the main parameters of size, shape, surface topography, optical properties of the tooth and restoration.
Literature
- Lomiashvili L. M. On the way to creating the secrets of tooth shapes
/ L. M. Lomiashvili // Klin. dentistry. - 2006. - No. 2. - P. 12-15. - Lutskaya I.K. Fundamentals of aesthetic dentistry.
/ I. K. Lutskaya. - Mn.: Let's lie. school, 2005. - 332 p. - Criteria for assessing aesthetic restorations: instructions for use No. 078-0906:
approved.
Ministry of Health of the Republic of Belarus 06/26/2007 / I.K. Lutskaya, N.V. Novak, T.A. Zapashnik, V.P. Kavetsky // Modern methods of diagnosis, treatment and prevention of diseases
: collection. instruction—method. doc. - Minsk: RNMB, 2007. - T. 5. - Issue. 8. - pp. 75-79. - Nikolaev A.I. Physico-mechanical properties of modern filling materials: significance for practical dentistry.
III. Dry shine and strength of composites / A. I. Nikolaev, L. M. Tsepov, P. G. Adamov // Maestro of Dentistry. - 2003. - No. 3. - P. 28-32 - Pogorovskaya I. Ya. Comparative assessment in vitro of color indicators and color stability of composite and glass ionomer materials for aesthetic restoration of teeth
/ I. Ya. Pogorovskaya, I. M. Makeeva, E. A. Emilenko. - M., 2001. - P. 83-84.
How to identify distal occlusion: symptoms of occlusion
The most characteristic signs, especially for non-specialists, are facial, caused by improper formation of the skeleton and unbalanced development of the neck muscles. Because of this, the so-called bird profile appears with distorted proportions and retraction of the lower lip.
There are also more specific, but still quite noticeable points:
- protrusion (protrusion) of the frontal incisors;
- insufficient closure of the teeth of the lateral group.
Since the anomaly progresses from a very early age, the child gradually develops infantile swallowing and mouth breathing. The chewing muscles are not strengthened well enough, over time the functions of the TMJ are weakened, and all this provokes the appearance of periodontal and dental diseases.
Signs of distal bite
It is quite possible to identify occlusion independently, not only by the incorrect position of the teeth when closing, but also by other signs: by certain facial features, features of facial expressions, even by body position or behavior. There are so many nuances that they can be divided into 3 main types.
Intraoral
It is relatively easy to determine the anomaly by looking at the upper frontal incisors. Normally, they should overlap the lower ones by about one third. In case of violations, they are lowered more strongly, and even pushed forward - so much so that there is some distance between the rows, in scientific language it is called the sagittal gap.
External
You should think about how to correct a distal bite in an adult (or at least make an appointment with an orthodontist for a consultation) if:
- the facial profile is convex, “bird-like”;
- the chin is disproportionately small, sloping, with an impressive fold;
- the nose, small in itself, protrudes significantly;
- in a relaxed state, the lips do not close.
The problem is also reflected in posture: the body is always slightly tilted, the neck seems longer, the stomach sticks out, the shoulders are hunched.
Functional
If a person has this disorder, it is more difficult for him to breathe through his nose, chew food, swallow, even speak (often unclear diction, lisp). Although he usually does not notice these inconveniences, since the anomaly develops gradually, from the age of 4-6 years, and the body simply adapts to it.
Treatment of wear of hard dental tissues
Normalization of occlusal relationships is the first and most important stage. Measures to correct occlusion include restoration of the occlusal surfaces of teeth, orthodontic treatment, and more.
Treatment of bruxism requires a comprehensive interdisciplinary approach [27]. Depending on the severity of manifestations and causes, psychiatrists, neurologists and physiotherapists take part in treatment. There is a need to manufacture an occlusal splint or mouth guard and use intraoral devices.
Therapeutic and orthopedic treatment methods are used to eliminate hard tissue defects. When restoring the vestibular surfaces of teeth, the leading requirement is aesthetics; for the occlusal surfaces, mechanical strength is the main requirement.
With increased abrasion, preference is given to orthopedic treatment methods - crowns and onlays.
In the case of cervical defects, it is recommended to prepare hard tissues to a depth of 0.5 mm, form a bevel, and restore with composites or GIC [28]. The enamel is ground around the defect using fine-grained diamond burs coated with 80 microns (with a red marking strip); some authors recommend reducing the enamel etching time to 5 seconds. [29].
An innovative method for closing defects is the use of direct composite onlays, manufactured in a factory. For example, COMPONEER manufactured by Coltene/Whaledent (Switzerland) - thin composite onlays (0.3-0.7 mm) with a uniform surface - allows you to close defects in the hard tissues of teeth [30] (Fig. 9a - d).
Rice. 9a. Patient 1 before treatment.
Rice. 9b. Patient 1 after treatment: metal-ceramic bridges in the area of the lateral group of teeth, Enamel White Opalescent composites on teeth 14,13,12,11, base A1/B1; lower incisors - restorations from Synergy D6.
Rice. 9th century Patient 2 before treatment.
Rice. 9y. Patient 2 after treatment: Enamel White Opalescent compositors on teeth 12, 11, 21, 22, S0 Miris base and W paint on teeth 12 and 21.
Diagnostics
Most people aged 50 years and older experience the physiological type of abrasion. The doctor needs to determine in time when the natural process turns into a pathological one. One of the main methods remains measuring the actual parameters of crowns. In addition, it is important to carefully study the shape of the dental units and determine areas of contact with antagonists. The height of the coronal part is compared with age standards established scientifically.
Diagnostic measures include assessment of fissures and enamel condition. The doctor pays attention to the patient’s facial expressions and appearance. It is important to talk in detail about your complaints and describe your feelings.
To assess how correctly the temporomandibular joint functions, electromyography is indicated. X-ray examination, electroodontodiagnosis and other procedures are carried out.
What is distal bite (occlusion)
This is a pathology in which the upper jaw is not located at the same level as the lower jaw, but is significantly pushed forward, as a result of which the teeth close incorrectly, with displacement. And not only the front ones, but also the lateral ones, which creates a block that prevents the healthy development of all incisors.
It arises and develops as a result of one, several or a whole group of interrelated factors (discussed in detail below), which entails other anomalies, most often diastema. Over time, it also causes weakening of the chewing muscles, respiratory problems and other complications that are dangerous to the body.
Medical Internet conferences
Introduction. Currently, dental erosion occupies a significant place among diseases of hard dental tissues. There are many opinions about the origin of erosive defects, and this issue has not been fully studied. This topic gives rise to a lot of controversy and questions among scientists and doctors, and therefore requires more attention. Research results indicate a significant increase in the prevalence of dental erosion in the last 10 years. Thus, when examining a population group, 47.2% of people with dental erosion were identified, while 10-15 years ago there were no more than 5-7% of such patients. When analyzing the frequency of non-carious dental lesions, based on patients’ visits to the dental clinic, 29.5% of people with dental erosion were identified. Meanwhile, 10-15 years ago there were only 24 such patients. Moreover, the disease was observed mainly in women (84.9%) aged 25-30 years. The combination of erosions with hormonal disorders (including dysfunction of the thyroid and gonads) accounted for more than 75% of cases.
Objective: to analyze literature data on the etiology of erosive defects and their impact on the quality of life of patients.
Tasks:
1) characterize the hypotheses of the origin of erosions of hard dental tissues
2) to study the mechanism of occurrence of erosions of enamel and dentin
3) assess the quality of life of patients with erosive dental defects
4) create a draft treatment plan for patients suffering from erosive dental changes.
Materials and methods: scientific articles and works, domestic and foreign scientific literature on dentistry were analyzed, clinical cases of erosion of hard dental tissues of varying severity of the pathological process were analyzed.
Results and discussions. Hard tissue erosion (erosion) (from the Latin erosio - “corrosion”) is the progressive loss of tooth enamel and dentin. In foreign literature, both narrow terms are used: “attrition”, “abrasion”, “erosion”, “abfraction”, and broader ones: “toothwear” and “tooth surface loss”. In European literature, the most common point of view is that erosion is a more important factor in the loss of hard dental tissues than abrasion due to contact of tooth surfaces. Occurs after teething. The affected area can be located on the vestibular and palatal surfaces and has a round, cup-shaped shape with dense, smooth, flat edges. This is a differential diagnostic feature when making a diagnosis. The upper incisors are primarily affected, less commonly the canines and premolars. It is extremely rare that erosions occur on the teeth of the lower jaw. Probing and percussion are painless. EDI 2-4 µA. The oral mucosa is without visible pathological changes.
2. The causes of erosion have not been clearly established.
According to ICD-10, the pathological condition of hard dental tissues is divided into two large groups:
· “Disorders of development and teething”
· “Other diseases of dental hard tissues.” K03
Tooth erosion refers to diseases of the hard tissues of teeth. K03.2
K03.2 Tooth erosion:
K03.20 Professional;
K03.21 Caused by persistent regurgitation or vomiting;
K03.22 Due to diet;
K03.23 Caused by drugs and medications;
K03.24 Idiopathic;
K03.28 Other specified dental erosion;
K03.29 Dental erosion, unspecified.
The first four causal factors of this classification reflect the chemical theory of the development of dental erosion present in the medical literature of previous years, which in turn considers the impact of aggressive chemical agents on the enamel as the leading causes:
I. External factors:
1) type of diet: consumption of acid-containing foods and drinks (marinades, pickles, citrus fruits, fruit and berry juices, sweet carbonated drinks, etc.)
2)work in hazardous industries associated with inhalation of acid fumes, metal and mineral dust particles
3) The effect of a number of medications on tooth enamel, for example, acid (acetylsalicylic and ascorbic), gastric juice preparations, hydrochloric acid.
II. Internal factors:
4) Dental erosion can be caused by chemically aggressive contents of the stomach and duodenum with a low pH content in chronic gastroesophageal regurgitation that occurs with gastroesophageal reflux disease, as well as with combined duodeno-gastroesophageal reflux disease. Erosive lesions are observed in individuals with hiatal and diaphragmatic hernias and those suffering from bulimia.
Damage from internal factors usually occurs on the palatal surfaces, and from external factors - on the buccal surfaces.
D. A. Entin saw the cause of erosion in neurodystrophic processes that cause decalcification of hard tooth tissues. However, no one can explain why erosions occur in some cases and wedge-shaped defects in others. Their occurrence may be associated with a violation of mineral metabolism due to endocrine or other disorders in the body and, accordingly, in the dental pulp. This is confirmed by the results of clinical observations and data from radioimmunological studies, which indicate the presence of clear preceding and concomitant dysfunctions of the thyroid gland in patients with erosions of dental enamel. Thus, Yu. M. Maksimovsky et al., analyzing the causes of erosions, assign an important role to endocrine disorders and, above all, hyperfunction of the thyroid gland. It was noted that dental erosions in patients with thyrotoxicosis were detected 2 times more often than in persons with normal thyroid function; a direct connection was established between the intensity of dental damage and the duration of thyrotoxicosis. As the duration of the disease increases by 1 year, the number of patients with erosion of hard dental tissues increases by 20%.
Dr. Kim McFarland, a dental surgeon and professor at the College of Dentistry at the University of Nebraska Medical School in Lincoln, USA, notes an increase in the number of patients with erosion of tooth enamel over the past 25 years, which is associated with uncontrolled consumption of carbonated sugary drinks.
A number of researchers (Baume, Port and Eidler) associate tooth erosion with excessive mechanical stress on the enamel, namely the use of hard toothbrushes, whitening toothpastes and powders with increased abrasiveness, as well as improper brushing techniques - a predominance of horizontal movements.
The combination of several predisposing factors accelerates the course of erosion and aggravates its severity. For example, drinking large amounts of very low pH drinks causes tooth surface loss when combined with brushing immediately after an acid attack on the teeth.
Yu. M. Maksimovsky details the clinical manifestations of erosions and distinguishes three degrees of damage, based on the depth of the hard tissue defect:
I degree (superficial, initial) – with damage to only the upper layer of enamel
II degree (medium) – with damage to the enamel throughout the entire depth up to the enamel-dentin border.
III degree (deep) – with damage to the entire enamel and the upper layer of dentin.
E.V. Borovsky et al., distinguish two stages of damage: initial (enamel erosion) and severe (enamel and dentin erosion).
In degrees 1 and 2, the lesion is white with a shiny surface; in degrees 3, brown or light yellow pigmentation appears.
Dental erosion is usually characterized by a chronic course, but there are two clinical stages of erosion: active and stabilized.
The active stage is characterized by a progressive course and loss of tooth tissue, accompanied by hyperesthesia and the disappearance of the shine of the erosion surface. In the active phase, changes in the size of erosion occur every 1.5-2 months.
The stabilized form of erosion of hard tooth tissues is characterized by a calmer, slower course, and the shiny surface of the enamel in the affected area is preserved. There is no change in its size for 9-11 months. A transition from a stabilized form of erosion to an active one is possible, especially if the background pathology worsens.
3. Pathogenesis
Unlike dental caries, where there is superficial, subsurface demineralization of the enamel, during erosion, superficial foci of demineralization are formed, which gradually cover the tooth enamel layer by layer. The microhardness of the enamel in the area of erosion is significantly reduced, and foci of demineralization of the enamel surface are noted. When studying the ultrastructure of enamel during tooth erosion using a scanogram, it was noted that the enamel in the area of erosion and in adjacent areas is characterized by a reduced degree of mineralization and the presence of destructive changes: in some areas, enamel prisms are clearly visible, interprismatic spaces are pronounced, and in others, enamel prisms and interprismatic spaces indistinguishable due to demineralization. Hydroxyapatite crystals of various shapes. In areas adjacent to erosion, they do not have clear boundaries or have a regular shape, but are large. Crystals of enamel hydroxyapatite with varying densities are visible on the surface of the enamel, indicating uneven mineralization. There are also distinct changes in dentin during tooth erosion: areas with a dense arrangement of crystals are observed. Dentinal tubules can be obliterated or non-obliterated. The structure of the substance that obliterates the dentinal tubules is specific and close to that during abrasion, however, along with the indicated areas of demineralization, accumulations of bacteria were found that mask the contours of the enamel prisms.
Comparative electron microscopy (SEM) of the central erosion zone also showed the presence of significant structural changes in both the superficial and deeper layers of damaged dental tissue. The active stage of the process is characterized by the loss of both enamel substance and dentin in large areas that have undergone destructive changes.
In the cervical region of teeth with erosive defects, an intermittent but quite clearly visible boundary between the crown and root is visible. In all studied cases, the crown enamel was layered on the root cement.
4.Quality of life of patients with dental erosion.
Enamel is the protective shell of the tooth. The process of enamel erosion is irreversible and creates problems for a person for life.
Patients complain of an aesthetic defect, the presence of a defect in the cervical area, tooth sensitivity, and tissue loss.
According to our data (based on the number of visits to the clinic), about 15% of patients are aged 16-42 years.
We observed 3 patients with varying degrees of dental erosion.
1) Patient A., 23 years old; preliminary diagnosis: dental erosion, stabilized form; mild severity according to ICD-10 K03.2. Complaints about dissatisfaction with the color of teeth. Objectively: on the vestibular surface in the cervical area of 1.1 and 2.1 teeth there is a defect affecting only the upper layer of enamel, the oral cavity is sanitized, the oral mucosa is without pathological changes, IG - 1.7 (satisfactory).
History: consumption of freshly squeezed citrus juices, professional cleaning with Air-flow 2 times, tried to use whitening toothpastes.
2) Patient K., 28 years old; preliminary diagnosis: active stage of dental erosion, moderate to severe degree according to ICD-10 K03.22
Complaints about tooth sensitivity, aesthetic defects, yellow teeth.
Objectively: on the vestibular surface in the cervical region, 1.1 teeth have a pronounced defect within the enamel and 2.1 teeth have affected the entire enamel and the upper layer of dentin. The oral cavity is sanitized, the oral mucosa is without pathological changes IG-2.2 (unsatisfactory).
History: consumption of citrus fruits, incorrect selection of oral hygiene products and items, incorrect method of brushing teeth with a predominance of horizontal movements.
3) Patient L., 42 years old; preliminary diagnosis: active form of dental erosion, severe degree according to ICD-10 K03.21
Complaints about the presence of defects in the cervical area, tooth sensitivity and aesthetic defects.
Objectively: erosive defects in the frontal group of teeth of the upper and lower jaw, in the cervical area there are lesions of brown pigmentation. The oral cavity is sanitized, the oral mucosa is without pathological changes, IG-1.6 (satisfactory)
History: occupational hazards, chronic gastroesophageal regurgitation, traumatic occlusion, crowded teeth.
Thus, regardless of the severity of erosion, the quality of life of these patients suffers to one degree or another. Even if practically nothing bothers the patient at first, in the future, in the absence of correction of etiological factors and specialist interventions, the symptoms increase like an avalanche (according to patients with more pronounced defects), which forced us to try to create an algorithm for treatment and preventive measures (draft treatment plan) for this group patients.
5. RECOMMENDATIONS
Enamel erosion is not just an external problem, but a serious disease, and therefore the attitude towards treatment is no less serious.
- A thorough ascertainment of the patient’s history and current condition with the involvement of related specialists (therapist, gastroenterologist, endocrinologist, pediatrician, etc.), gastronomic preferences, and features of professional activity will significantly identify the possibility of correcting patient-dependent factors or, at a minimum, recording them in the outpatient dental record. sick.
- Treatment of patients with erosion should be comprehensive and long-term.
- Strict diet (except citrus fruits, berries, sweets, carbonated drinks, fresh juices containing vitamin C, canned foods). Include protein in your diet to strengthen the protein matrix of enamel and collagen fibers.
- Select products (pastes containing organic calcium, with hydroxyapatite) and hygiene items (correction of the rigidity and structure of the brush bristles, excluding the use of toothpicks), as well as teach the correct method of brushing teeth (vertical movements).
- Remineralizing therapy (Rocs medical minerals gel, Remars gel, Clinpro™ White Varnish,) Tooth Mousse, “Belagel Sa/R” “VladMiVa”) in a clinical setting in the form of applications and mouth guards (preferably individually). At home daily, perhaps constantly, but necessarily regularly, depending on the degree - office-based in combination with fluoride applications to prevent concomitant caries and to strengthen the crystal lattice of hydroxyapatite.
- Avoid ultrasonic teeth cleaning, home and professional whitening, and Air-Flow teeth cleaning.
- For professional hygiene, use pastes with minimal abrasiveness “fine”.
- Restoration if necessary, after complex treatment. It is possible to use the Icon technique, as well as the use of a desensitizer (SHIELD FORCE PLUS).
- clinical examination with photographic recording of the result.
Conclusions:
1. In the etiology of erosion of hard dental tissues, the following factors interact: exogenous (occupational hazards, dietary habits) and endogenous factors (metabolic disorders, endocrinopathies, bruxism, diseases of the gastrointestinal tract) in combination with improper oral care.
2.The main mechanism is demineralization of the enamel.
3. Regardless of the severity of erosion, the quality of life of these patients suffers to one degree or another. Even if at first there is practically nothing bothering the patient, in the future, in the absence of correction of etiological factors and specialist interventions, the symptoms increase like an avalanche.
4. The algorithm of treatment and preventive measures for this group of patients should include:
-correction of both external and internal etiological factors;
-specialized treatment by a dentist before the required restoration with the use of remineralizing and fluoride-containing drugs up to restoration (using filling materials from the group of compomers or GIC);
- general treatment with mandatory medical examination for a long time (lifelong).