Difference between molars and premolars
The main difference between molar teeth and premolars is their location on the jaw.
Premolars are located closer to the front of the dentition, and molars are slightly moved inward. Their quantity also varies. There are always two premolars on each side of the upper and lower jaws. There can be either two or three molars. Still others are also called “wisdom teeth.” They grow later than others and often appear only at 20-25 years of age. This process is often accompanied by malaise and fever. However, not all people on earth have third ones. A certain genetic predisposition can cause the absence of wisdom teeth in the oral cavity.
Content:
- In what cases are molars removed?
- Reasons for the formation of a lump after wisdom tooth removal
- Dangerous symptoms
- How to treat a lump after tooth extraction
- What happens if you don’t treat a lump after a tooth extraction?
Most patients at dental clinics believe that pulling out a diseased tooth will relieve them of painful symptoms.
They treat the extraction procedure as a life-saving one. But, unfortunately, it is not always possible to solve the problem completely surgically. It happens that a small tumor soon forms in the vacant space. A seal on the gum after tooth extraction indicates the need to urgently visit a doctor. Below we will tell you why it occurs and how doctors fight it.
Features of the structure of molars
Molars have a characteristic structure. On the upper jaw they have three roots and four canals. The lower jaw has two roots and three canals. Moreover, the number of canals also differs depending on the location of the individual tooth. Thus, the first of them often have one more channel than the next two.
The main characteristic feature of this type of teeth is the area of their chewing surface. They bear the heaviest load when chewing food particles. The molars themselves also have differences among themselves, which are associated with the structure of the jaw.
Molar Differences
Often the surface of each molar tooth is shaped like a triangle. There is a certain number of tubercles on it, which take an active part in chewing food. The number of such tubercles may vary. Usually there are three, but sometimes there are more.
Such mounds are connected to each other by special ridges. On the upper and lower jaws the structure of these elements is different. In the upper dentition, the apex of the surface triangle is directed towards the tongue. This form is called a trigon. On the lower jaw, the apex of such a triangle is directed towards the cheek, which is called the trigonid. The size of the first and second types of teeth is practically the same.
Dangerous symptoms
If a lump appears after tooth extraction, you should inform your doctor about it. Particularly dangerous symptoms are:
- discharge of pus;
- severe swelling;
- acquisition of bluish tint by fabrics;
- pain on palpation;
- absence of a protective blood clot.
Trying to cure a disorder without medical help is not only unwise, but also dangerous. By engaging in amateur activities and experimenting with folk recipes, a person risks creating conditions for the further spread of the inflammatory process. Then it is possible that the extraction will be followed by a second operation. This time it will be aimed at removing tissues affected by the purulent process.
Possible damage to small molars
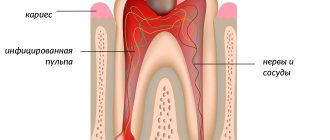
Carious lesions of primary and molar teeth in children are observed quite often. This is due to the bumpiness of their surface, which can trap food particles and bacteria. Since children at an early age do not always actively and correctly brush their teeth, these residues can lead to damage to the enamel and deeper spread of caries.
Depending on the degree of damage, caries can penetrate either exclusively into the enamel, or into dentin or even cement. In the latter case, we are talking about deep caries, which often requires serious treatment or even tooth extraction.
Another variant of damage is a change in tissue structure, which may be associated with metabolic disorders in the human body or other diseases. Such a disease can also be the result of poor nutrition or constant diets, in which the body does not receive enough nutrients.
At any age, a person can experience excessive tooth wear, which leads to the destruction of enamel and can cause other serious damage. Teeth can wear down in different situations, such as:
- if a person has bad habits of grinding his teeth, etc.;
- in case of improper or insufficient nutrition;
- in the presence of diseases of the endocrine system;
- due to a genetic predisposition to enamel depletion.
All of these lesions can be the result of both an incorrect lifestyle and various diseases or heredity. Regardless of the reasons, it is necessary to begin treatment of emerging injuries immediately so as not to aggravate the process.
Reasons for the formation of a lump after wisdom tooth removal
The problem occurs for various reasons. Most often, a lump is formed due to:
- Severe injury to gum tissue. In this case, the disorder may be non-infectious in nature and go away on its own in two to three days. Anti-inflammatory drugs prescribed by a dental surgeon will help get rid of it. A particularly traumatic operation is to tear out “eights”, the roots of which are very long and winding.
- Individual intolerance to drugs used to treat the wound. Allergies cause itching and swelling. Increased separation of watery exudate is possible. To relieve unpleasant symptoms, you must stop using medications. The dentist will help you choose a more suitable analogue.
- Attachments of the inflammatory-infectious process. It occurs if bacteria enter the open socket, which is possible with an unformed blood clot. A complication in the form of a “dry” socket is likely if the doctor violated the extraction technique or the patient did not follow the instructions of the dental surgeon during the recovery period.
- Formation of flux in the operated area. Periostitis is manifested by purulent discharge, swelling of soft tissues, and increased body temperature. After extraction, it occurs due to the fact that pathogenic flora penetrates into the open wound cavity.
Replacement of primary molars with permanent permanent molars
Molars are the first permanent teeth to appear in a child's mouth. This begins around the age of five. Growth begins with the first molar tooth, which appears in a free space in the depths of the jaw, closer to the milk one that has not yet fallen out.
The second molar usually grows in at the age of 12-13 years. It also takes up free space and does not replace a baby tooth. The latter, or “wisdom teeth,” may take up to 25 years to grow or may not appear at all.
As for dairy products, they begin to fall out from the age of 9. In their place, permanent teeth grow, which occurs at approximately 10-12 years of age. Usually these are the last molars, the growth of which must wait to fill the adult dentition (not counting “wisdom teeth”).
Is it possible to loosen baby molars?
The process of tooth loss always begins with softening of its root. This occurs as the jaw grows, freeing up more space for a permanent tooth. Thus, while the baby tooth is still in the hole, the molar is already beginning to take its correct place.
In this regard, dentists categorically do not recommend deliberately loosening baby molars. If they fall out prematurely, jaw growth may be stunted. As a result, there will not be enough space for permanent teeth, and they will begin to grow crookedly, getting out of the general dentition.
Signs of imminent appearance of molars
The first signs that molars are about to appear are noticeable even before the baby teeth fall out. These include the following:
- widening of the jaw, which can be seen when gaps appear between other baby teeth;
- the appearance of sufficient free space behind the outer lateral milk teeth;
- swelling of the gums.
In this case, the temperature does not necessarily have to rise or the child’s well-being deteriorates, as was the case with the growth of baby teeth. This is why the appearance of the first molars often goes unnoticed.
Helping your child replace teeth
The process of replacing teeth often takes place without pain or discomfort. The roots of baby teeth dissolve on their own, and the dental crown falls out freely. However, there are a number of recommendations that should be followed during this period.
The main one is systematic rinsing of teeth for disinfection purposes. This is necessary in order to avoid bacteria from entering the hole that will form at the site of the falling tooth. In addition, the sharp edges of a crown that has separated from the gum may cause minor damage to soft tissue. To prevent them from becoming inflamed, it is important to exclude any infection.
If your child experiences any pain during the tooth replacement stage, you should immediately consult a doctor. Under no circumstances should pain be eliminated using improvised methods.
Molars and prevention of their loss
Molars are stronger than baby teeth. However, they need proper care to prevent their loss, because new ones will not grow in place of a lost tooth.
Prevention of molar tooth loss involves proper oral hygiene. It includes systematic brushing of teeth, use of dental floss and mouthwash. In addition, you should carefully monitor the condition of your teeth and consult a doctor if even minor damage is detected.
Proper balanced nutrition is also mandatory. Especially in childhood and adolescence, you need to ensure that your body gets enough calcium and vitamin D.
Many people experience discomfort after having crowns installed. Gradually, the body adapts, but an incorrectly installed crown on a tooth can cause a lot of trouble. We will tell you how to determine whether it is installed correctly.
What criteria are used to check?
During the check, several parameters are determined:
- correct anatomical shape;
- cervical coverage density;
- position of the crown edge;
- color matching.
If a dental crown is installed correctly, it will last for more than two decades. If installed incorrectly, a number of problems may arise.
Correct anatomical shape
The crown should follow the anatomical shape of your own tooth. This applies to the masticatory cusps, contact points and the equator.
tubercles
The chewing surface has a relief. It consists of tubercles and depressions that perform a specific function: they ensure correct bite, grind and chew food. With a correct bite, the cusps of the upper tooth correspond to the sockets of the lower one, which ensures their complete closure or occlusion. If the occlusal surface is not recreated correctly, then complete closure will not occur. At the same time, the teeth will begin to shift, which can lead to overload of the ligamentous apparatus, impaired diction, distortion of facial geometry, and premature wear of the tooth.
Gradually, the patient begins to feel that the crown on the tooth has adapted to the dentition, but he does not notice a change in the bite. Such a violation can lead to problems with the temporomandibular joints and ligaments of the jaw.
Examination:
In the first few days, a new dental crown always causes discomfort, it just takes time to fully adapt. However, if this condition has lasted for more than a week, then there is a possibility of occlusion violation. The dentist checks the closure using special paper.
Equator
Molars have a convex lateral surface, thanks to which food rolls into the oral cavity, bypassing the gums. This convexity is called the equator. If the crown on the tooth does not have a lateral convexity, food enters the periodontal sulcus. The result is inflammation of the gums, followed by dystrophy, in which the tooth root is exposed.
Examination:
A sign of the absence of a convexity can be bleeding of the gums in the area where the crown is installed, its inflammation and bad breath.
Contact point
The adjacent teeth meet at a point called the point of contact. If it is not there, then the food gets stuck and remains in the interdental space. The result is inflammation of the interdental gingival papilla.
Examination:
You need to pass dental floss between the teeth, which should pass with some tension and a click. If it passes freely, but food constantly gets stuck there, then there is no contact point.
Cervical coverage
If the crown on a tooth exceeds the permissible size, saliva, food particles get under it, and microbes remain, which leads to the resorption of the cement. The crown does not protect the tooth, caries develops in it, and the edges of the gum become inflamed.
Examination:
An indirect sign of a wide dental crown can be tooth pain in response to cold or hot food, as well as bad breath and an inflammatory reaction of the gums in this area.
Crown edge position
The edge of the crown should descend into the gum by 0.1-0.3 mm. Otherwise, saliva will wash cement into the resulting gap. If the crown goes deeper, a periodontal pocket may form.
Examination:
When a crown is normally installed on a tooth, its edge is not visible; it comes out of the gum.
Color matching
The color of a ceramic or metal-ceramic dental crown should not differ too much in shade from the adjacent teeth.
Examination:
Consider the dentition. The crown should not stand out too much in color.
Maxillary premolars
The crown of the premolars on the upper dentition has a prismatic shape. The buccal and palatal bones often have a convex surface. The first and second premolars in the row also have their differences.
First premolar
The difference between the first premolar of the upper jaw is the predominance of the vestibular surface over the palatal surface. Its contact surfaces are rectangular in shape. The buccal tubercle has two distinct slopes. The root of such a tooth often has a bifurcation.
Second premolar
In such a tooth, the buccal surface usually predominates over the palatal surface, which is more rounded. In most cases, this premolar tooth has a single cone-shaped root. However, there are also cases when it has a split.