Phlegm in the throat
Sputum is a secretion in the form of mucus formed in the cells of the epithelium (mucous membrane) of the bronchi. Fragments of bacteria, desquamated epithelial cells and other components may be mixed with this mucus. Mucus moves through the bronchi, mixes with saliva and nasal discharge. Normally, sputum should be transparent and released in small quantities, without causing any discomfort. Smokers and those who work in dusty environments may produce sputum in large quantities. Sputum usually forms in the lower parts of the respiratory tract (trachea, bronchi, bronchioles) and, accumulating, irritates the receptors, causes a cough reflex and comes out through the mouth.
Some patients call phlegm nasal discharge that flows down the back wall of the nasopharynx, as well as discharge from chronic pathologies of the oropharynx and larynx.
That is why sputum production can be associated with various pathological processes. In case of such complaints, it is necessary to conduct a full examination of the patient, find out the details of the medical history and conduct a series of tests.
Condition Characteristics
From the moment the virus enters the body until the clinical symptoms of enteric coronavirus appear, 2 to 5 days pass. This condition does not occur in an asymptomatic form. Unlike the respiratory form, after a person has had an intestinal form of coronavirus, their body develops unstable immunity. The clinical picture of this condition is largely reminiscent of gastroenteritis.
In patients with chronic diseases of the gastrointestinal tract, the clinical symptoms of intestinal coronavirus are more pronounced.
Causes
Diarrhea due to coronavirus infection can be either primary or secondary. The primary variant of the disease develops from the direct effect of the virus on the body. When the virus is transmitted by the fecal-oral route, in the intestinal lumen the pathogenic microorganism attaches to the epithelial cells of the organ mucosa and provokes the development of the inflammatory process.
The secondary variant of the intestinal form of coronavirus is a complication that occurs after complex treatment of Covid-19. In 90% of cases, complex therapy for this infectious disease includes taking antibiotics, as this helps prevent the addition of a secondary bacterial infection. Antibiotics, in turn, have a detrimental effect not only on pathogens, but also on beneficial intestinal microflora. A person is faced with a phenomenon called dysbiosis.
Sputum with cough
A cough with sputum or a wet, productive cough may indicate various diseases of the respiratory system, from ARVI to allergies. There are a number of diseases and conditions that are characterized by coughing with sputum:
- Smoking. A larger amount of mucus forms in the lungs of a smoker, which the body tries to get rid of, causing a cough;
Infections of the upper and lower respiratory tract. Viral, fungal, or bacterial infections also cause coughing. Quite often, a common cold can cause complications in the form of tracheitis, bronchitis and other more severe diseases, accompanied by a wet cough;
Bronchial asthma. With this disease of an infectious-allergic nature, the secretory function of the lung mucosa also increases, as a result of which sputum is released;
Abscess (purulent focus) of the lung or bronchiectasis. If there is an abscess in the lung, it is possible to separate its purulent contents, requiring separation by coughing;
Tuberculosis. This disease is characterized by the presence of blood in the sputum;
- Entry of a foreign body into the respiratory tract. Foreign particles in the respiratory tract cause irritation and, as a result, cough.
Principles of treatment of cough with sputum
If a person is suffering from a cough with sputum, it is recommended to provide plenty of fluids; it is possible to use drugs or herbal remedies that have an expectorant, anti-inflammatory, enveloping and bronchodilator effect. There are several groups of medications that are prescribed to relieve the symptoms of wet cough:
- expectorants . They are prescribed for viscous sputum to facilitate the process of its removal from the respiratory tract. A similar effect is achieved through reflex stimulation of the glands located in the bronchial mucosa. When using these drugs, the amount of mucus may increase due to the dilution of sputum;
- mucoregulating agents. They help reduce the secretion of sputum and, like expectorants, allow it to be removed from the body. In case of exacerbation of bronchial asthma, the use of these drugs is contraindicated, therefore, before taking, you should consult with your doctor;
- mucolytic agents. They improve the removal of sputum by stabilizing the release of bronchial secretions. These drugs are usually prescribed for tracheitis, bronchitis, pneumonia and other diseases;
- antihistamines. They are prescribed if the cough is a consequence of allergies. They help alleviate the consequences of the body's reaction to certain irritants. If you are bothered by a sore throat, sputum of unusual color and consistency, cough, fever and other unpleasant symptoms, you should consult a doctor. Such manifestations are a consequence of a number of diseases, so consultation with a specialist is necessary to make a diagnosis and select therapy. This will help avoid complications and start treatment in a timely manner.
Sputum without cough
Sometimes the accumulation of phlegm is not accompanied by a cough. The method of treatment will depend on the cause of the symptom.
The reasons for the accumulation of phlegm in the throat without a cough can be both physiological processes and diseases. In this case, patients complain of a feeling of a lump in the throat, which they want to cough up, but there is no cough. The accumulated mucus is difficult to excrete, and the person suffers from soreness and itching in the throat.
Additional symptoms accompanying this condition may include fever, severe runny nose, etc. Phlegm in the throat without a cough can be a manifestation of various diseases, so it is impossible to make a diagnosis based on this symptom alone. Additional diagnostics are required.
Diseases that may be accompanied by phlegm in the throat include:
Rhinosinusitis of various etiologies (allergic, viral, bacterial, fungal);
Latent forms of tuberculosis;
Smoking can also cause the formation of sputum that is difficult to cough up. Particles of tobacco smoke settle on the mucous membrane of the nose, throat, and nasopharynx and form thick, difficult-to-remove mucus.
Why does phlegm accumulate?
Accumulation of sputum is rarely the only manifestation of the disease. It is usually accompanied by other symptoms, such as fever, cough, runny nose, etc.
The main reasons for the accumulation of sputum include:
- A runny nose or rhinosusitis of any origin (viral, bacterial, fungal) can cause the appearance of sputum. Mucus and pus formed as a result of the inflammatory process in the nasal cavity and pharynx do not exit through the nose as a result of swelling and flow down the back wall of the larynx;
Acute viral diseases are the main cause of sputum formation. Usually, at the beginning, the patient’s temperature rises, the throat begins to hurt, when the inflammatory process spreads lower to the trachea and bronchi, a cough with thick sputum appears;
Gastro-esophageal reflux, gastritis and esophagitis. In these diseases, the contents of the stomach and esophagus are thrown back into the throat, irritating the mucous membrane, which causes chronic inflammation of the larynx and throat with mucus secretion.
Bronchial asthma is characterized by the reaction of the bronchi to various allergens. In addition to the formation of sputum, symptoms of this disease also include suffocation, wheezing in the chest, and coughing with difficult-to-clear sputum.
Pneumonia and pleurisy. Inflammation of the lung tissue and pleurisy is always accompanied by the formation of thick foamy sputum, high fever, and chest pain.
Causes of foul-smelling sputum
Lung abscess
In the acute course of the pathology, large quantities of purulent sputum with a foul odor are expectorated.
The unpleasant odor is caused by the breakdown of protein compounds as a result of prolonged stagnation of exudate in the abscess cavity. Sputum begins to be coughed up suddenly, “mouth full”, its amount reaches 1 liter. The stench when an abscess breaks into the bronchus is so strong that it can be felt several meters from the patient. With chronic pulmonary abscess, there is periodic coughing up of fetid pus and mucus in small quantities. During an exacerbation, the volume of foul-smelling sputum increases to 300-500 ml per day. Febrile fever, weakness, and chills occur. Patients complain of pain in one half of the chest, shortness of breath on exertion, and night sweats.
Lung gangrene
With extensive destruction of lung tissue, dirty gray putrid sputum appears. It has a pungent odor and coughs up large volumes - 500-1000 ml per day. If the blood vessels are damaged, the expectorated secretion contains blood impurities. Pulmonary gangrene is characterized by the release of foul-smelling sputum in a mouthful after a coughing attack. Symptoms include dull chest pain, hectic fever, and disturbances of consciousness.
Aspiration pneumonia
The disease, as a rule, proceeds hidden. Initially, when you cough, a scanty amount of mucus mixed with pus is released, which smells unpleasant. As aspiration pneumonia progresses, the amount of discharge increases. The sputum gradually acquires a putrid character, its smell becomes even more fetid and pungent. Hemoptysis often begins, and when large vessels are destroyed, pulmonary hemorrhage occurs. Patients experience chest pain, febrile fever, and chills.
Foul-smelling sputum
Friedlander's pneumonia
For this type of pneumonia, the appearance of brown, foul-smelling sputum with scarlet blood streaks is pathognomonic. Gradually, the amount of pus in the discharge increases. With Friedlander pneumonia, the sputum acquires a characteristic smell of burnt meat, which distinguishes the pathology from other types of lung damage. Patients are exhausted by a painful paroxysmal cough, difficulty breathing, and interruptions in the functioning of the heart.
Bronchiectasis
If the disease is complicated by infection with anaerobic flora, typical purulent sputum is replaced by putrefactive sputum, and the stench becomes more noticeable. Patients after a cough paroxysm cough up large amounts of grayish-green pus. Foul-smelling sputum is secreted intensely in the morning after waking up. The clinical picture of bronchiectasis is complemented by shortness of breath and pain in the chest area.
Empyema of the pleura
Foul-smelling sputum is expectorated when the inflammatory process is complicated by a bronchial fistula. In this case, the purulent exudate accumulated in the pleural cavity is drained through the respiratory tract when coughing. Expectorated sputum has a foul odor and is dirty green in color. When coughing, patients experience severe pain in the affected part of the chest. With pleural empyema, a forced position is typical: half-sitting with emphasis on the arms placed behind the body.
Lung cancer
When a malignant tumor disintegrates, a painful cough occurs with expectoration of foul-smelling brown, dirty green or gray sputum. The discharge has a heterogeneous structure, sometimes reddish particles of destroyed lung tissue are visible in it. Symptoms are more typical for peripheral lung cancer, while with a central location of the tumor, bleeding often occurs and atelectasis of the affected lobe or segment develops.
Ozena
With fetid atrophic rhinitis, thick, bloody-purulent nasal discharge is formed, but it can flow down the back of the throat, causing a cough with sputum. The patient constantly emits a noticeable putrid odor, which is not associated with a coughing attack or blowing his nose. During ozena, the olfactory receptors are usually damaged, so the patient himself does not feel the stench. Patients are concerned about dryness and painful itching in the nose, and disturbances in nasal breathing.
What is sputum - causes and types of secretions
Most diseases of the respiratory system are characterized by fever, redness of the throat and severe cough. Doctors say that the best option is when spasms of the chest muscles are accompanied by sputum production. What is the secretion of the tracheobronchial tree and should we be wary of such a symptom of pathology? Let's deal with this issue together.
Clinical symptoms
In 50% of patients diagnosed with Covid-19, intestinal symptoms of coronavirus infection initially appear. Respiratory symptoms such as shortness of breath, dry cough, sore throat, and fever may develop later. The most likely symptoms of intestinal coronavirus include:
- partial or complete loss of appetite;
- bowel disorders in the form of diarrhea;
- nausea and vomiting;
- cutting pain in the abdomen.
Additionally, the clinical picture of the intestinal form of coronavirus can be supplemented by headache, dizziness, fever, general weakness, increased sweating and muscle pain.
The duration of the so-called acute phase of an infectious lesion of the gastrointestinal tract is individual. On average, this period ranges from 4 to 10 days. Compared to the respiratory form of coronavirus, the intestinal form of the disease is more severe and its symptoms are more pronounced.
Stool disorders due to intestinal coronavirus in humans persist for 2-5 days. Vomiting may persist for 2-4 days.
What is phlegm used for?
Sputum is a mixture of secretions from the paranasal sinuses, nasal mucosa, saliva and waste products of pathogenic microorganisms that cause inflammation in the lungs and bronchi. Mucus is necessary to “filter” any foreign substances that enter the respiratory system from the outside. In most cases, phlegm is beneficial. The exception is the abnormal release of formations that interfere with normal breathing.
Many patients at an appointment with a therapist or pulmonologist ask where does sputum come from? In fact, this question is not correct. Mucus is produced throughout life. If the ciliated epithelium stops transporting phlegm to the upper respiratory tract, then the risk of infectious infection of the lungs increases significantly.
Types and color of sputum
A healthy person daily gets rid of 50-100 ml of mucus, consisting of dust and other substances foreign to the body. During illness, the amount of phlegm produced can increase 10-15 times (1500 ml). Therefore, there is no need to worry too much when detecting mucus when coughing. This is believed to be a normal occurrence during treatment of viral and bacterial lesions.
It is necessary to seek help from a medical institution if the composition and color of sputum changes. A severe inflammatory process may be accompanied by the discharge of serous, purulent, bloody or glassy phlegm. Such symptoms often indicate the development of dangerous diseases of the respiratory system (tuberculosis, bronchitis, pneumonia, cancer).
Many doctors make an initial diagnosis based on the color of the sputum:
- clear discharge should not frighten the patient, since the absence of impurities indicates a gradual extinction of inflammation;
- glassy mucus should be a reason to check the body for the presence of bronchial stenosis;
- yellow sputum is considered an indicator of an increased fight by the immune system against infection (pneumonia, asthma, bronchitis);
- green discharge is usually viscous and difficult to expectorate due to an increased concentration of neutrophils, epithelium and dead pathogenic agents (staphylococcus, streptococcus);
- brown phlegm indicates spread of the disease to the lower respiratory tract or internal bleeding (ruptured capillaries).
Sputum with blood must be removed into a separate group. This symptom occurs when the lung tissue is severely damaged. Usually, patients with similar signs of the disease are immediately hospitalized.
The danger of intestinal coronavirus
This condition is dangerous not only because an inflammatory reaction develops, but also because during vomiting and diarrhea, the human body loses a large amount of fluid, which can result in dehydration (dehydration). Elderly people with additional chronic diseases are at particular risk. For them, this condition poses a threat not only to health, but also to life.
Diagnostics
By analogy with the respiratory form of coronavirus, diagnosis of the intestinal form of the disease is carried out using a laboratory PCR test. The nature of the patient's complaints is taken into account.
Other reasons for the formation and discharge of mucus when coughing
During the examination, the doctor will definitely ask a question about the time when the unpleasant symptom appeared. If sputum production is observed in the morning, then first of all it is necessary to exclude natural sources of phlegm. Often the cause of excessive discharge during coughing is an allergic reaction to external irritants (dust, dry air, animal hair). The possibility of poisoning from chemicals (fumes from household chemicals) cannot be ruled out.
Mucous, viscous sputum may form in smokers. With cigarette smoke, soot, soot and other toxic elements enter the lungs.
The negative effect on the bronchi causes a decrease in the respiratory lumen and a weakening of the functions of epithelial cells. The phlegm accumulated overnight comes out in the morning with a dry, paroxysmal cough.
Diseases characterized by sputum production
Many respiratory tract diseases are accompanied by the formation of large amounts of secretion. Respiratory pathologies almost always provoke the body to produce phlegm. What pathologies need to be excluded first?
- Tuberculosis is a persistent infection caused by Koch bacilli. This disease is characterized by abnormal sweating, loss of appetite, and low-grade fever (37°C). A distinctive feature of the disease is white (initial stages), greenish or bloody sputum when coughing.
- Pneumonia develops due to infection of the lung tissue by bacteria, fungi or viruses. The main manifestations are a sharp jump in body temperature, a dry, unproductive cough with wheezing, chest pain, and shortness of breath. The secret is yellow or green.
- Bronchitis is characterized by swelling of the mucous membrane and accelerated production of immunoglobulin. Such processes cause blockage of the bronchi and complicated sputum production. Symptoms of the disease resemble the classic cold with the appearance of white, yellow or green phlegm.
Self-diagnosis is not allowed. Treatment should be prescribed by a specialist (therapist, infectious disease specialist, immunologist or pulmonologist).
Indications for sputum analysis
It is necessary to seek help from a medical facility if the cough continues for more than 2 weeks, there is a suspicion of pneumonia, tuberculosis or other dangerous diseases, or there are impurities in the sputum (pink, green, yellow or glassy mucus).
Phlegm analysis allows:
- accurately determine the cause of increased mucus production;
- exclude oncology (lung cancer);
- check discharge for allergy markers.
When the bacterial nature of sputum is identified, the laboratory conducts studies on the resistance of pathogenic microflora to various types of antibiotics.
How to alleviate the patient's condition
Normal sputum production is considered a good sign. The release of a clear secretion of normal viscosity shows that the treatment of the root cause of cough is moving in the right direction. Additional stimulation of mucus expectoration is needed in case of stagnation of secretions.
Preparations for removing phlegm:
- mucolytics are necessary to increase the volume of mucus with a dry, unproductive cough (“Mukaltin”, “ACC”, “Ambroxol”);
- expectorants are prescribed to facilitate the removal of secretions from the bronchi (“Lazolvan”, “Stoptussin”, “Doctor Mom”);
- natural syrups and mixtures increase immunity and relieve irritation of the mucous membrane (Gedelix, Gerbion, Althea Root).
It is better to start treating a child with relatively safe methods of traditional medicine. If the sputum is viscous, but without impurities (purulent, pink, serous), then you should use decoctions of sage, oregano, calendula, and licorice. Inhalation therapy and the use of compresses show good results.
What is phlegm and why can it change color?
A productive (wet) cough indicates the activation of mechanisms that help cleanse the lungs and bronchi from pathogenic microorganisms, toxins or particles of polluted air (tobacco smoke, dust). The body ensures the removal of infection and toxic substances from the respiratory system by increasing the secretion of mucus (sputum, phlegm) secreted by the glands of the bronchi and trachea, and by activating the cough reflex.
The sputum takes on a yellow or yellowish-green tint if it contains impurities of pus, which indicates the development of inflammation, which is caused by a bacterial infection. The bright yellow (canary) color of phlegm is due to an increased content of eosinophils and is observed with eosinophilic infiltrative processes in the lungs or bronchial asthma.
The discharge of yellow mucus may also be due to subjective reasons. Tobacco and nicotine tars give the mucous exudate a yellow-rusty hue. Eating large amounts of carrots or citrus fruits can also cause the formation of large amounts of yellow exudate.
Signs of physiological and pathological cough
Coughing is an unconditioned reflex that helps clear the respiratory tract of accumulated mucus or foreign particles caught in the flow of inhaled air. Normally, a person can cough up to 20 times during the day. The main signs of a physiological cough are the absence of:
- prolonged attacks;
- wheezing, suffocation;
- systematicity;
- symptoms of the disease.
A cough that appears in the morning is most likely caused by the accumulation of phlegm in the respiratory tract during sleep.
A pathological cough appears with the development of foci of inflammation localized in the respiratory system. In this case, symptoms characteristic of a particular disease are observed, which make it possible to diagnose the disease.
Main characteristics of pathological cough:
- strength (from coughing to hysterical cough);
- duration (acute, protracted, chronic);
- timbre (short, barking, ringing, hoarse, silent);
- presence of discharge (productive, unproductive);
- characteristics of phlegm (the shade of sputum, its viscosity, whether there are blood clots or pus in it).
When diagnosing a pathological cough, the time of day and season are taken into account:
- morning cough is typical for both smokers and tuberculosis patients;
- evening cough occurs with chronic bronchitis or pneumonia;
- a night cough may be a symptom of acute bronchitis, an allergic reaction to dust or posterior rhinitis;
- the spring and autumn seasons are characterized by allergies (cough, runny nose, lacrimation) to flowering plants;
- In winter, cough syndrome is observed with acute respiratory infections and is accompanied by fever, joint pain and rhinitis.
Diagnosis of cough with yellow sputum
Coughing with yellow mucus is a symptom of many diseases of the respiratory system. For a more accurate diagnosis, the doctor must examine the patient, conduct auscultation using a stethoscope or phonendoscope, and obtain the results of blood, urine, and sputum tests. If necessary, a chest x-ray, spirometry, bronchoscopy or computed tomography may be prescribed. If you suspect bronchial asthma (including hereditary), your doctor may recommend skin testing to identify allergens.
When making a diagnosis, the specialist notes all the symptoms, since the appearance of yellow phlegm accompanies various diseases of the respiratory tract. Only by a combination of signs, by identifying the pathogen and determining the localization of the inflammatory or degenerative process, will the doctor be able to accurately diagnose the disease and prescribe appropriate treatment.
A cough with yellow sputum appears with pneumonia (pneumonia). In this case, an increase in temperature is observed, it remains stable for 3 to 5 days, after which a period of “imaginary well-being” begins, followed by an exacerbation of the disease. The causative agents of the inflammatory process localized in the lung segments are the following pathogenic microorganisms:
- Klebsiella;
- Staphylococcus aureus;
- hemolytic and viridans streptococci, etc.
When you cough, thick sputum comes out, the yellow color of which is due to the presence of pus in it, consisting of:
- serous fluid;
- mucus;
- dead white blood cells;
- infectious agents.
Unlike pneumonia, with bronchitis the inflammatory process is localized exclusively in the bronchi.
In tuberculosis, the causative agent of which is tuberculous mycobacteria (Koch bacilli), the sputum acquires a yellow tint only at some stages of the disease. The early stages are characterized by white or light yellow pigmentation of the exudate, and with the development of cavernous forms, hemoptysis appears. The doctor may prescribe additional tests aimed at identifying the causative agent of inflammation or pathological changes in lung tissue, with a cough without fever that lasts more than 3 weeks, as well as other symptoms of tuberculosis:
- increased sweating;
- loss of appetite;
- sleep disorders;
- sudden weight loss, etc.
Bronchiectasis also causes yellow mucus to be coughed up. This disease is characterized by the appearance of hollow formations in the bronchial alveolar structures that are filled with pus. The sputum released with a cough is a multi-layered structure of yellow color interspersed with blood. To accurately diagnose the disease, it is necessary to conduct a number of studies to exclude pneumonia or emphysema.
Sinusitis is also characterized by the appearance of a cough with yellowish sputum, which contains purulent discharge from the inflamed sinuses.
Lung abscess is a papular formation that is localized in the tissues of the bronchi or lungs. When the papule is opened, suppuration or purulent melting of the lungs may develop, accompanied by the release of large volumes of yellow exudate mixed with fresh blood. This condition leads to respiratory failure and a high risk of death.
Sputum with a yellow tint can be observed with the development of a cancerous tumor located in the central segments of the lungs. The color of the exudate is due to the presence of pus and blood in it.
Diagnosis of a disease accompanied by a cough with yellow sputum should be carried out by a pulmonologist. After comparing the results of studies, tests and examination, the doctor will make a diagnosis and determine the direction of treatment.
Self-medication can lead to complications of the current disease and cause exacerbations of chronic diseases. If your child has a cough, you should consult a pediatrician.
Diagnostics
If you complain of foul-smelling sputum, an examination by a pulmonologist is indicated. During a physical examination, a specialist assesses the nature and frequency of breathing, performs percussion and auscultation of the lungs to make a preliminary diagnosis. If destructive processes in the lungs are suspected, consultation with a surgeon is required. The diagnosis plan for diseases manifested by sputum with an unpleasant odor includes the following methods:
- X-ray imaging.
X-ray examination of the OGK is recommended in 2 projections, which shows rounded shadows with a horizontal level of liquid, areas of infiltration or decay, and the contours of space-occupying formations. To clarify the diagnosis, MSCT is prescribed, which allows detailed visualization of pathological changes. - Bronchoscopy.
When examining the bronchi with an endoscope, signs of diffuse purulent endobronchitis are mainly detected. If the foul-smelling sputum is caused by an oncological process, during bronchoscopy the doctor sees a disintegrating tumor that is blocking the bronchus. During the study, biopsies are taken from suspicious areas. - Sputum analysis.
When the biomaterial settles, a division into 3 layers is found (purulent, mucous and foamy). Upon visual examination, you can see particles of pulmonary parenchyma, foreign bodies, and pathogenic fungi. A culture of foul-smelling sputum is performed to isolate the infectious pathogen and perform an antibiotic sensitivity test. - Additional laboratory tests
. Changes specific to inflammation are detected in the hemogram: increased ESR, neutrophilic leukocytosis. A biochemical blood test reveals dysproteinemia and an increase in acute phase parameters. To assess respiratory failure, blood gases are analyzed.
If symptoms of pleurisy are detected, a therapeutic and diagnostic puncture of the pleural cavity and collection of exudate for bacteriological examination are necessary. For patients with chronic bronchopulmonary diseases, ECG and echocardiography are performed to study the functioning of the heart, since such pathologies are often combined with hemodynamic disorders. In difficult cases, they resort to angiopulmonography and diagnostic thoracoscopy.
Lung abscess - cause of foul-smelling sputum
How to cure a cough with yellow phlegm
For ARVI or bronchitis, the doctor may prescribe drugs that have mucolytic or expectorant properties. Medicines belonging to such pharmacological groups can be of either synthetic or plant origin.
Similar medications for productive cough are prescribed as follows:
- expectorants are recommended for the separation of thin or not too thick sputum;
- Mucolytic agents are prescribed if the sputum is thick and viscous, and its separation is difficult.
Medicines with expectorant properties may have different mechanisms of action:
- resorptive - irritate the bronchial mucosa to increase sputum production;
- reflex - irritate the gastric mucosa, stimulating the vomiting center and increasing the secretion of mucus in the respiratory tract and the peristalsis of the bronchial muscles.
Mucolytic drugs are divided into:
- diluting bronchial secretions and increasing the elasticity of sputum (for example, ACC);
- accelerating the release of exudate from the bronchi (Ambroxol and Bromhexine);
- reducing sputum formation (M-anticholinergics and glucocorticoids).
If a drug is effective in relieving cough in an adult, this does not mean that this drug can be used in pediatrics. When choosing medications for treating children, you need to consult a pediatrician, since reflex expectorants can cause vomiting and depression of respiratory function in a child.
Causes of white sputum when coughing
The causes of the appearance of white sputum can be various diseases, both not very serious, for example, a viral infection, and infections that require timely detection and appropriate treatment, such as pulmonary tuberculosis.
Depending on the etiology, the nature of the white cough discharge may vary, namely:
- fungal infection: with long-term use of antibacterial drugs, a significant decrease in the protective forces of the immune system, representatives of pathogenic or conditionally pathogenic fungi, for example, candidiasis, can begin to multiply on the mucous membrane of the tracheobronchial tree, which will lead to changes in mucous secretion. It will be a copious white, curd-like discharge;
— pulmonary tuberculosis: the nature of the sputum, its color, consistency and other parameters in tuberculosis can be different, however, sometimes the sputum acquires, just like in fungal infections, a curdled consistency and a white tint. However, with tuberculosis, there is a paucity of sputum discharge;
Important! If you experience a prolonged cough with curdled white sputum, you should definitely consult a doctor so that he can make a differential diagnosis between a fungal infection and pulmonary tuberculosis and prescribe the necessary appropriate treatment.
— viral infection of the respiratory tract: with this pathology, the sputum has a watery consistency, white, and slightly transparent;
— allergic reactions: this type of changes in the body is caused by individual intolerance to various substances. Cough with sputum production is usually caused by aerosol allergens, such as dust, gaseous chemicals, volatile liquids, etc. In this case, thick or slightly watery white mucus is released when coughing;
- bronchitis: at some stages of bronchitis, coughing up a whitish, transparent secretion may be observed, which indicates the onset of the inflammatory process;
- oncological pathology: in the initial stages of lung cancer, the separation of transparent sputum with a white tint may be observed, but the separation of pure white sputum is quite rarely observed; white sputum with blood streaks is more common, which indicates the presence of a complication;
- smoking: smoking abuse can lead to hypersecretion of the glands of the bronchi and trachea, which manifests itself in the form of a constant productive cough with the release of first white, then white with a grayish sputum. Later, an unpleasant odor may appear.
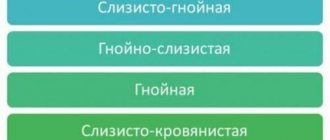
Types of sputum
Depending on the causes, the cough can be dry or wet. Of course, the latter type is easier for humans to tolerate and responds better to treatment. Thanks to the release of mucus from the respiratory tract, recovery occurs faster. But in this case, it is necessary to carefully monitor the characteristics of the sputum, its color and consistency, in order to detect the pathological process in time and begin appropriate therapy. Otherwise, seemingly harmless symptoms can lead to serious consequences. The following types of sputum are distinguished:
- mucous membrane (whitish or colorless);
- serous;
- purulent (yellow-green);
- mucopurulent;
- bloody (yellowish-transparent with blood impurities).
Of the listed types, only mucous sputum does not pose any particular danger. It occurs in diseases of the respiratory tract accompanied by catarrhal inflammation (initial manifestations of an acute inflammatory process or a chronic inflammatory process in remission). The greatest risk to the patient’s health is indicated by purulent and mucopurulent sputum, which is formed in such serious diseases as bronchitis, pneumonia, bronchiectasis, tuberculosis, abscess and gangrene of the lung. Only a doctor can determine the cause of a particular symptom, so you should not self-medicate and cause the disease to worsen. In addition, the color of sputum largely depends on a person’s lifestyle. For example, heavy smokers may produce sputum of different colors: from white to brown. This phenomenon indicates the need to take care of lung health.
Principles and basic methods of treating a patient with white sputum separation
Treatment of the symptom of sputum itself will not give any results, since the appearance of pathological discharge from the tracheobronchial tree occurs against the background of some reason, a disease that led to the appearance of a productive cough.
You should definitely consult a doctor who can correctly determine the cause of the appearance of white sputum when coughing. Depending on the etiology, the necessary treatment is prescribed.
For example, when a fungal etiology is identified, antifungal drugs are prescribed, and it is also necessary to normalize the microflora of the respiratory tract, since the proliferation of opportunistic fungi usually occurs after long-term use of antibacterial drugs, which leads to disruption of the natural biocenosis.
When a diagnosis of pulmonary tuberculosis is made, the patient is sent to a specialized anti-tuberculosis institution, where he is prescribed antimycobacterial therapy that corresponds to the sensitivity of mycobacteria to drugs.
In case of a viral infection, bed rest with minimal physical activity, plenty of warm fluids, antiviral drugs are indicated; in case of a bacterial infection, antibiotics are indicated.
Treatment
Help before diagnosis
Cough with foul-smelling sputum occurs with severe lesions of the bronchopulmonary system, which cannot be treated at home. If you have such a symptom, you should consult a doctor as soon as possible. If the symptom is accompanied by impaired consciousness, hemoptysis or pulmonary hemorrhage, hectic fever, the patient needs emergency medical attention.
Conservative therapy
Most diseases that cause foul-smelling sputum are caused by bacterial infections. Therefore, etiotropic antimicrobial therapy is selected with the inclusion of drugs in the therapeutic regimen based on the results of the antibiogram. Combinations of 2-3 drugs are recommended, which are administered parenterally or locally (into the pleural cavity). Long-term antibiotic therapy is required - at least 10-14 days.
To improve sputum discharge, inhalations with brocholytics and proteolytic enzymes are used. To remove toxic products from the blood, detoxification methods are indicated: administration of electrolyte solutions in combination with diuretics, plasmapheresis, and the use of desensitizing agents. To improve the rheological properties of blood, anticoagulants and antiplatelet agents are prescribed.
If the patient’s condition is satisfactory and moderate, it is possible to perform percussion or vibration massage of the chest, which enhances the drainage function of the bronchi and stimulates expectoration of foul-smelling sputum. After the acute process subsides, physiotherapy is effective: ultrasound, speleotherapy, magnetic therapy. Patients are given complexes of breathing exercises and exercise therapy.