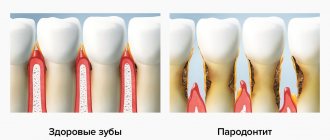
Generalized periodontitis is a type of oral disease that belongs to the group of inflammatory diseases and affects periodontal tissue. Its course is accompanied by bleeding gums, swelling, and unbearable pain. The situation is aggravated by the occurrence of bad breath, the appearance of dental plaque, and the formation of periodontal pockets.
Only a competent periodontist can diagnose the disease by examining the oral cavity and performing a biopsy of the gum tissue. Treatment involves the use of medications and surgery. General and immunomodulatory therapy plays an important role.
Periodontitis is a condition in which diffuse disruption of the periodontal complex occurs. The disease affects several teeth at once, and in particularly serious cases, all teeth. This is one of the most difficult problems in dental practice. The generalized form of the disease is 5 or 6 times more likely than caries, leading to partial or complete adentia. And the prolonged development of infection in the oral cavity is the cause of the formation of rheumatoid arthritis, infective endocarditis, atherosclerosis, stroke, and heart attack.
What is periodontium, its features
In dental practice, the term “periodontium” is used. It includes a whole complex of tissues surrounding the teeth. They all have a common nerve origin and a single blood supply, therefore they are closely related to each other. The periodontium forms several constituent elements: gums, bone tissue, periodontium, cement of the root system of the teeth. Its functions include providing support, maintenance, and protection of the entire dental system. Pathologies associated with periodontal damage include conditions such as gingivitis, periodontal disease, tumors, and periodontitis.
Reasons for the development of generalized periodontitis
The precursors to the formation of the disease are some exogenous and endogenous factors. The first group is small; most of the diseases of this system are provoked precisely by the internal state of the body. All etiological factors are classified into local (plaque, tartar, problems with bite, abnormal position of teeth, strands of the mucous membrane) and general (diseases of the body - diabetes mellitus, goiter of toxic origin, excess weight, hypovitaminosis, hepatitis, gastritis, etc. ). All this one way or another affects the condition of the periodontium and leads to a deterioration in its functioning.
Microbiological studies have been able to prove the fact that the leading role in the development of this condition is given to microorganisms called Prevotella Intermedia, Bacteroides forsythus, Peptostreptococcus, etc. In order for the dental system to be protected from their influence, protection in the form of plaque is provided in the dental plaque , accumulated in the gingival sulcus, periodontal pockets, and tooth roots.
The life products of pathogenic organisms contribute to the activation of the secretion of certain substances (prostaglandins, cytokines, enzymes), which lead to the destruction of periodontal tissue structures. Factors that entail a decrease in local and general protection from the influence of pathogenic bacteria include:
- smoking,
- radiation damage,
- ignoring the rules of personal hygiene regarding the oral cavity.
The development of this condition is usually preceded by inflammation of the gingival margin, which entails disruption of the connection, destruction of the ligamentous apparatus, and resorption of the alveolar bone. These changes lead to pathological mobility of teeth, overload of their individual groups, and occlusion. In the absence of adequate therapy, this disease provokes tooth loss or removal, as well as problems with the functioning of the jaw system as a whole.
Classification and symptoms of generalized periodontitis
If you take into account the depth of the pockets and the severity of bone tissue destruction, the doctor can diagnose three forms of manifestation of the disease. They differ in symptoms and signs.
Mild periodontitis
This stage is characterized by a slight sensation of itching and burning. Bleeding periodically occurs during brushing your teeth and after eating (hard foods - meat, fresh fruits and vegetables). The depth of periodontal pockets reaches 3.5 mm, and a decrease in gum tissue is observed at approximately 1/3 of the height of the root. Pathology may not manifest itself for a long time. Therefore, at the first stage of the disease, patients are in no hurry to contact doctors, which provokes the transition of the disease to more severe forms.
Average degree of periodontitis
During its course, various pathological changes occur in the patient. In particular, the functions of the dental system change. The pocket reaches a depth of 5 mm, the teeth become mobile and slightly loose. Gaps appear between them. The tissue structure of the hole is reduced by half the root. There may be an unpleasant odor coming from your mouth.
Severe periodontitis
This disease is typical for adult patients. The depth of the periodontal pockets exceeds 5 mm, the loss in tissue is more than ½ the length of the tooth root. The gums are subject to severe inflammation and bleed. They come out with purulent discharge. Not only tissue elements are destroyed, but also bone parts. Sometimes the walls between the teeth completely dissolve, leading to severe tooth mobility. In this case, it is almost impossible to preserve them in their natural form.
The more advanced the disease, the more difficult it is to cope with it and choose adequate treatment. And the chances of a full recovery decrease with each step of its progression.
What is periodontitis
Periodontitis is one of the most common dental diseases. Symptoms of periodontitis can affect many people to varying degrees for a variety of reasons.
But, despite this, many people often do not pay special attention to the first signs of this disease, as a result of which periodontitis can worsen and develop into severe forms of the disease, which, in turn, most often leads to the loss of a tooth or even several teeth, and as well as other complications.
Periodontal tissue surrounds the root of the tooth and is designed to hold the teeth firmly in place. In other words, periodontal tissues include vessels, hard fibers and channels involved in the process of feeding hard tissues.
Periodontal pathology is an inflammation of its tissues, the cause of this inflammation is the penetration of infection into the periodontal tissue. Periodontitis often occurs as a result of a complication of gum disease such as gingivitis, or due to untreated caries.
Periodontitis in severe advanced form and in the acute phase is accompanied not only by bleeding gums, but also by purulent discharge and ulceration of the gums (formation of ulcers on the gums).
If periodontitis starts and treatment is not started on time, the inflamed gum tissue begins to peel off from the roots of the tooth, causing the teeth to become loose, and if treatment is not started, the teeth may begin to fall out.
Also, periodontitis can develop during pregnancy, since during pregnancy there is a temporary decrease in natural immunity, while the progression of the disease in the first stages is often characterized by a latent course.
In this case, as a treatment, dentists try, if possible, to limit themselves to the use of gentle medicinal treatment methods, and continue treatment after the woman is ready for more serious therapy.
Features of the chronic form of generalized periodontitis
Any other oral disease can be a provoking factor in the development of the disease. Gingivitis, neglect of personal hygiene rules, mechanical damage - all these are obvious reasons for the development of a chronic form of pathology. It occurs in two stages:
- exacerbation, accompanied by throbbing pain in the gums, excessive bleeding, pus discharge, abscesses, fever, inflammation of the lymph nodes (such symptoms often make themselves felt against the background of pneumonia, stressful situations, ARVI);
- remission, which occurs during therapeutic measures; during this time, symptoms do not appear, and nothing bothers the patient.
The further the pathology develops, the longer the exacerbation lasts, and the time of remission gradually decreases.
Classification and forms of periodontitis
Before starting treatment for periodontitis, the dentist conducts a diagnosis, the purpose of which is to determine the form and stage of the pathology. Based on the study of the characteristics of the course of the disease, the following types of periodontitis are distinguished:
Acute stage of periodontitis: this stage is characterized by the rapid development of foci of infection, which in a short period of time can lead to serious complications. The gums begin to bleed heavily, and acute painful sensations appear when pressing on areas of inflammation, brushing teeth, or eating hard foods.
Within a very short time (several days), periodontitis can lead to the rapid formation of significant abscesses and the subsequent formation of fistulas.
Chronic form of periodontitis: when periodontitis is chronic, the pathology usually does not manifest itself with such pronounced symptoms as in acute cases. The patient may not experience any discomfort or experience minor discomfort, but this fact does not mean that the inflammatory process does not occur and does not develop.
Treatment methods for periodontitis
Treatment of chronic generalized periodontitis is complex and depends on the severity of the manifestation. In general, medical and preventive measures are aimed at solving a number of problems.
- Elimination of symptoms that cause discomfort.
- Relieving inflammation in the oral cavity.
- Strengthening the protective properties of periodontium.
- Prevention of the appearance of dental deposits in the form of stone and plaque.
- Prevention of relapses and exacerbations.
This is the general treatment plan. There are private sets of measures, depending on the stage of progression of the pathology.
How does periodontitis occur?
As a result of several scientific studies, statistics were collected that showed that people between the ages of 30 and 40 most often experience periodontitis.
At the same time, these data do not allow us to assert that the occurrence of periodontal pathologies is directly dependent on a person’s age.
How to reduce the risk of periodontitis
To minimize the possible occurrence of periodontitis, you need to undergo preventive examinations with a dentist every six months, lead a healthy lifestyle, eat right and carefully observe oral hygiene.
Directions of therapy for mild periodontitis
The chronic form of mild periodontitis is treated in stages, here is an approximate diagram.
- First, plaque and deposits formed on the tooth enamel are removed.
- Subsequently, the doctor prescribes topical antibacterial agents. They need to be applied in the form of applications to the affected areas. An important role is played by rinsing the mouth with solutions containing antiseptic components.
- The key to successful therapy is compliance with hygiene procedures (purchase and use of special healing pastes, professional toothbrushes, dental floss).
By providing thorough daily oral care and learning to visit the dentist regularly, you can avoid this sore and prevent worsening if it progresses.
Treatment of moderate periodontitis: possible options
If the disease is of moderate severity, therapy will take longer. In addition to these procedures, the complex should include the removal of decayed teeth and the use of steroidal and non-steroidal anti-inflammatory compounds. Also, to improve the general condition, doctors prescribe physiotherapy procedures:
- exposure to affected areas through short-wave ultraviolet radiation;
- carrying out a special massage of the gums, which can be vacuum, vibration, etc.;
- darsonvalization procedures;
- local hypothermia;
- electrophoresis.
Upon completion of treatment, it is necessary to make a follow-up visit to the doctor so that he can assess the general condition and make a prognosis.
What are the treatment options for periodontitis?
First of all, it should be noted that self-treatment of periodontitis at home without consulting a dentist often leads to neglect of the disease, complications and dangerous consequences. The treatment of periodontitis should only be carried out by a dentist, preferably a specialized specialist - a periodontist.
Treatment methods for generalized severe periodontitis
Chronic periodontitis, the course of which has moved to the last, most dangerous stage, requires not only careful conservative therapy, but also surgical intervention. Indeed, at this stage, tissue destruction is pronounced, and conventional antibiotics are not enough. You will need to undergo a number of procedures aimed at restoring the affected areas and replacing teeth. Depending on the overall picture, the following types of surgical interventions are prescribed:
- removal of teeth with a high degree of mobility;
- vertical dissection of the gum wall in order to scrape tissue that has undergone pathological changes;
- horizontal excision of the pocket wall together with the affected gum (if the depth of the periodontal pockets is more than 4 mm);
- flap surgery (coronal displacement, lateral, therapy, transplantation, etc.);
- abscess incisions;
- plastic surgery in the frenulum of the tongue, lips.
An important role in the treatment of this form of the disease is played by the use of anti-inflammatory drugs, vitamin compounds, and drugs that strengthen immune function. The prognosis of the disease at this stage is unfavorable, since exacerbation does not entail remission and lasts almost constantly. In addition to tooth loss and gum decay, there is the possibility of systemic complications.
What to do to avoid complications
To avoid complications, it is necessary to recognize the disease in the early stages and take measures for adequate treatment. All this will allow you to achieve stable and long-term remission and preserve the functions of your teeth and gums. In order for the dental system to be healthy, it is necessary not only to observe the rules of personal hygiene, carrying out regular care procedures, but also to periodically visit a specialist who will perform professional cleaning in order to remove minor dental deposits.
General symptoms of the disease
In the initial stages, the patient suffers from severe bleeding gums. They become loose and swollen. The patient feels itching, throbbing, severe burning, pain when he chews food. An unpleasant odor begins to emanate from the mouth. Dental pockets at this stage are shallow, they are located mainly in the interdental spaces. At the initial stages, the teeth are motionless and not displaced anywhere. The patient's general condition is normal.
The clinical picture of the developing disease is somewhat different. In addition to the above symptoms, the patient may experience:
- displacement of teeth and their loosening;
- high sensitivity of teeth to external irritants (temperature fluctuations);
- problems chewing food;
- disturbance of general well-being (typical of severe forms of pathology), accompanied by weakness, malaise, and increased body temperature;
- an increase in the size of regional lymph nodes, which in addition become painful;
- during a dental examination, the doctor observes signs of diffuse gingivitis;
- Plaque and deposits accumulate abundantly on the teeth;
- tooth loss, fistula, abscesses (signs are characteristic of advanced stages of the disease).
In the case of a chronic form of the disease, the gums have a pale pink tint. There are no dental deposits, manifestations of pus or blood. There is a possibility of exposure of the roots of the teeth. X-ray does not show signs of bone resorption.
Periodontitis
Periodontitis is an inflammation of periodontal tissues with progressive destruction of these tissues and the bone of the alveolar process. Unlike gingivitis, periodontitis is characterized by the presence of a gingival or periodontal pocket, destruction of the tissues of the interdental septa of varying severity, which is determined on an x-ray.
There are localized (local) and generalized (general) periodontitis.
With localized periodontitis, one tooth is affected. Localized periodontitis develops under the influence of local causes: the entry of filling material into the interdental space, injury from the overhanging edges of the filling, or parts of orthopedic structures (dentures). It is characterized by food getting stuck in the interdental spaces, pain, hyperemia and swelling of the gums, and tooth mobility. Treatment of periodontitis is aimed at eliminating periodontal pockets and factors that damage the gingival margin.
Generalized periodontitis is a much more serious disease. It always begins with catarrhal gingivitis. With generalized periodontitis, the integrity of the dentogingival junction is disrupted, the ligamentous apparatus of the tooth is destroyed, bone tissue is resorbed, periodontal pockets with purulent discharge and extensive dental deposits are formed. Periodic exacerbations are accompanied by the occurrence of periodontal abscesses. The occurrence of generalized periodontitis is based on a violation of the protective barrier function of the periodontium, a decrease in immunity, as a result of which the process spreads from the gums to the underlying tissues. Treatment is complex, including curettage, surgical removal of periodontal pockets, antibiotics, metronidazole, and immunomodulatory drugs.
Acute periodontitis is rare and is characterized by aching pain in the gums, hyperemia of the gum edge, bleeding of the gums when touched and a violation of the integrity of the periodontal junction. No changes in bone tissue are detected. The cause of acute periodontitis is always associated with mechanical irritation (fillings, crowns, orthopedic devices, etc.). Treatment is aimed at eliminating these mechanical irritants, followed by applications of anti-inflammatory drugs.
Chronic periodontitis has several degrees of severity.
Mild chronic periodontitis has the following symptoms: bleeding gums when biting hard food and when brushing teeth; itching, numbness and tingling in the gum mucosa; swelling of the interdental papillae; hyperemia of the gums with symptoms of cyanosis (bluish coloration); a large amount of subgingival stone; the appearance of gum pockets up to 2 mm deep without discharge; The x-ray shows signs of osteoporosis of the interalveolar septa, with the apexes of the septa having the appearance of a truncated cone.
Chronic periodontitis of moderate severity has the following symptoms: bleeding gums; pain in the gums; bad breath; tooth mobility; the occurrence of pathological periodontal pockets more than 5-6 mm deep with purulent discharge; the necks and partially the roots of the teeth are exposed; the gingival margin is thickened like a roller; interdental papillae are swollen; the gums are hyperemic, loose, and bluish in color; The radiograph reveals resorption (absorption) of bone tissue up to 1/3 of the root length.
Severe chronic periodontitis is characterized by the following symptoms: pain when biting, sometimes the spontaneous appearance of tearing, pulsating pain; significant mobility and discrepancy of teeth; there are pathological periodontal and bone pockets up to 10 mm deep with copious purulent discharge; the necks and roots of the teeth are exposed; there are significant supragingival and subgingival dental deposits; the gums are strongly and unevenly thickened in a roller-like manner and easily peel off from the teeth, hyperemic, and have a bluish tint; The radiograph reveals bone resorption exceeding 1/3-1/2 the length of the tooth root; abscesses appear in certain areas; The patient's general condition is characterized by headache, increased body temperature to 37.5-38°C, and malaise.
Request a consultation
Diagnosis of generalized periodontitis
In identifying the disease, a special role is played by the clinical picture and the “age” of the disease. If there are concomitant diseases, the doctor can refer the patient for examination to other doctors - an endocrinologist, therapist, gastroenterologist, immunologist, rheumatologist, etc. When analyzing dental status, the doctor should pay attention to the following criteria:
- the amount of deposits on the teeth;
- their character;
- general condition of the gums;
- depth of the vestibule of the oral cavity;
- features of bite;
- condition of the bridles;
- degree of tooth mobility;
- formation of periodontal pockets.
As part of the initial examination, a Schiller-Pisarev test is taken and the periodontal hygiene index is determined. The doctor also examines scrapings from the gum pocket using PCR diagnostics and saliva chemiluminescence. Among additional diagnostic methods, it is recommended to conduct a biochemical analysis of blood fluid for glucose and CRP. Of no small importance is the determination of IgA, IgM, IgG indicators.
To identify the stage of development of the disease, the following is used:
- orthopantomography,
- x-ray of the intraoral cavity,
- biopsy of gum tissue.
Doctors pay special attention to differential diagnosis with pathologies such as gingivitis, periodontal disease, periostitis, and osteomyelitis. Like therapy, diagnosis must be comprehensive and include several examinations to make the most accurate diagnosis.
Periodontal measures for moderate disease
If the disease has become moderately severe, selective therapy is added to the above measures. It is aimed at grinding the surface of teeth that have undergone occlusion, removing deposits under the gums, applying therapeutic dressings and compresses. Along with this, questions are being resolved about whether it makes sense to remove roots or individual teeth, and whether it is worth carrying out splinting and orthopedic therapy. Local anti-inflammatory procedures are usually complemented by general therapy.
Stages of development of periodontitis. Localization of infection in periodontitis
Localized form of periodontitis: The onset of this type of periodontitis is usually caused by minor trauma to the mucosa. The localized form, in the absence of dental care, can progress to the next stage of the disease.
Generalized form of periodontitis: inflammation in the generalized form of the disease, inflammation develops along the entire length of the alveolar ridge. Experts in the field of periodontology argue that this form can quickly develop and become more complicated due to weakened immunity, for example, with a cold, hypothermia, infection with another infection, or self-medication with antibiotics.
Forms of periodontitis
According to the severity of periodontitis, there are: mild form, moderate form, severe form. At the beginning of the pathological process, slight bleeding, slight pain, and the formation of small periodontal pockets are observed. In the moderate form of the disease, large gaps appear in the periodontal pockets, and the teeth become mobile and loose. With the development of severe periodontitis, deformation of the interdental septa, decay of collagen fibers and root tissues are observed. Periodontal pockets become large, they contain purulent contents, and teeth fall out.
Is it possible to cure chronic generalized periodontitis?
In the process of getting rid of generalized forms of severe periodontitis, surgical manipulations are added to the listed methods. As part of these procedures, teeth with 3-4 degrees of mobility are removed, patch surgery is performed, abscesses are opened, etc. Based on the available indications, plastic surgery of the vestibule of the oral cavity and frenulum is performed. If the disease is accompanied by a particularly severe course, systemic anti-inflammatory therapy, immunomodulatory treatment, and vitamin intake are mandatory measures.
Physiotherapy takes part in complex therapy. In particular, the doctor prescribes electrophoresis, darsonvalization, laser treatment, hirudotherapy, herbal medicine, and apitherapy. Activities must be carried out under the supervision of a treating specialist in compliance with all his instructions. Violation of the treatment regimen is fraught not only with a lack of effect, but also with a complication of the general condition.
Forecast and preventive measures
If treatment is started in the early stages of the pathology, this leads to remission and the possibility of its extension. In restoration measures and in the process of preserving tissue functions, compliance with recommendations related to the implementation of preventive measures plays an important role. If the disease is advanced, the prognosis is unfavorable. This may be due not only to the loss of almost all teeth, but also to the fact that severe systemic complications will begin to develop, especially in the cardiovascular system.
The preventive complex involves compliance with a number of care and hygiene measures:
- timely brushing of teeth;
- a competent choice of cleaning products and tools - toothpastes, powders, brushes, threads;
- regular implementation of professional hygiene;
- timely treatment of emerging diseases;
- removal of deposits from the teeth;
- carrying out treatment of concomitant pathologies.
With these simple measures you can prevent illness and feel great.
Thus, generalized periodontitis is a serious disease that tends to constantly develop and progress. In this regard, it is necessary to diagnose it in a timely manner and take therapeutic measures. This approach will prevent complications and keep all teeth normal, eliminating unpleasant symptoms and improving the patient’s well-being.
Laser gingivectomy in the area of one tooth
Treatment of generalized moderate and severe periodontitis
Catarrhal and hypertrophic gingivitis symptoms and treatment in adults
Splinting teeth for periodontitis with fiberglass and tape
The roots of the teeth are exposed - what to do and how to treat them
Laser gingivotomy - surgical treatment of complex forms of periodontitis
Advanced periodontitis
Advanced periodontitis in the absence of timely initiation of treatment leads to the appearance of typical complications that have a detrimental effect on the condition of the body as a whole - the patient’s body temperature rises, headaches occur, general weakness appears, appetite and mood decrease.
Causes of periodontitis development
Periodontitis can occur for many reasons, the main ones being:
- untreated caries;
- advanced gingivitis;
- improper oral hygiene;
- lack of daily oral hygiene;
- using a toothbrush that is too hard, which injures the gums;
- incorrect, incorrectly and poorly installed fillings;
- the presence of subgingival deposits;
- improperly manufactured dentures that injure the mucous membrane;
- improper hygiene of dentures or lack of such hygiene;
- congenital prerequisites;
- complications after treatment of jaw fractures;
- jaw injuries;
- some types of malocclusions.
Also, the development of periodontitis can be caused by the presence of common general somatic diseases, such as:
- diseases of the cardiovascular system;
- disruptions in the digestive system;
- insufficient function of the salivary glands;
- vitamin deficiencies;
- disruption of the normal functioning of the hormonal system;
- severe stress;
- uncontrolled use of antibiotics;
- temporary drop in general immunity.
For what other reasons can periodontitis develop?
However, it is worth noting that with all the variety of possible causes for the development of periodontitis, according to statistical data obtained as a result of many studies conducted around the world, the main cause of periodontitis is the lack of oral hygiene or its poor or improper implementation. And, as a consequence, lack of oral hygiene leads to the formation of plaque, and then the formation of hard dental deposits (tartar). Everything else is just provoking factors.