- Acute herpetic stomatitis
- Traumatic stomatitis
- Chronic aphthous stomatitis
- Candidal stomatitis
Stomatitis is an inflammation of the mucous membrane in the oral cavity. It is believed that children are most vulnerable to stomatitis. In adults, stomatitis does not occur as often. The instability of children to stomatitis is explained by the fact that they have a more delicate mucous membrane; children tend to constantly put something in their mouth and taste it, which contributes to the entry of microbes and accidental injuries. In addition, children's immunity is at the stage of formation, and therefore they are becoming acquainted with many bacteria and viruses for the first time. The first encounter with bacteria or, for example, with the herpes virus can be accompanied by a fairly violent reaction from the body.
Causes of childhood stomatitis
The immediate causes of stomatitis are bacteria, viruses and fungi. These microorganisms may be present in small quantities in a healthy child, but they begin to multiply and cause disease in the presence of certain factors.
Factors contributing to the occurrence of stomatitis
- Failure to comply with hygiene rules (the child may touch the mouth with dirty hands), hard plaque on the teeth;
- Weakened immunity;
- Long-term use of medications (especially antibiotics). Antibiotics disrupt the natural microflora, promoting the growth of fungus and the occurrence of fungal stomatitis.
Diagnosis of pathology
The pediatric dentist prescribes diagnostic and therapeutic measures for stomatitis in children. To determine the main cause of stomatitis associated with internal diseases, it is necessary to undergo examination by a gastroenterologist, immunologist, allergist, virologist, endocrinologist or infectious disease specialist.
To make an accurate diagnosis you need:
- obtaining a clinical picture of the disease (collection of complaints and anamnesis);
- laboratory examination: blood test, smear and scraping materials;
- in case of frequent candidal stomatitis, a blood test for a glycemic curve is necessary;
- in case of aphthous stomatitis, stool sampling for ovitis and ultrasound examination of the internal organs of the abdomen are required.
Childhood stomatitis can be a consequence of many diseases, so it is important to undergo a full diagnosis to identify the cause. In cases where stomatitis is caused by a system-wide disease, additional examination is required.
Types of stomatitis in children
Modern medicine knows a huge number of varieties of stomatitis. They can have an acute course, that is, be accompanied by pain, discomfort, and a disturbance in the general condition, or they can have a chronic course. Chronic stomatitis passes almost unnoticed for a person, pain is not expressed, general health does not suffer.
Let's look at the most common types of stomatitis in children, which dentistry in Belarus .
Acute herpetic stomatitis
Acute herpetic stomatitis is caused by the herpes virus. There are several types of herpes virus. The disease that appears on the lips and in the oral cavity is caused by the first two types of the virus. Adults remember herpes when blisters appear on the lips due to stress or hypothermia, and in children it manifests itself in the form of ulcers in the mouth and even a rise in temperature. As a rule, the disease begins with inflammation of the gums and enlarged lymph nodes. If a child looks into the mouth, you will notice several bubbles on the mucous membrane of the lip, gums, and cheeks. Over time, the membrane of the vesicles bursts and ulcers form. These ulcers are painful and the child refuses to eat. This stomatitis occurs when the baby first encounters the virus.
It is most often transmitted from parents through kissing and sharing cutlery. 98% of the world's population is infected with this virus, so it is useless to protect yourself from it. Infection with the herpes virus does not always occur with manifestations of stomatitis, and is often completely unnoticeable. But, if the latter does appear, the parents’ task is to provide proper care and alleviate the symptoms.
Traumatic stomatitis
Traumatic stomatitis is associated with mechanical damage to the mucous membrane. Children often put toys and cutlery in their mouths and can injure themselves and cause stomatitis. Stomatitis can form at the point of contact between the edges of a decayed tooth and the cheek. A bacterial infection sometimes attaches to the wound, resulting in an inflammatory process that lasts several weeks.
Chronic aphthous stomatitis
Chronic aphthous stomatitis manifests itself in the form of white spots (aphthous) on the mucous membrane of the lips, cheeks and sometimes gums. In the first days, the spot is surrounded by a red rim. Then a small ulcer forms at the site of the spot. After 7-10 days, the ulcer heals. The causes have not been fully elucidated, but it is believed that it often occurs in children with allergies, intestinal diseases and weakened immune systems.
Candidal stomatitis
Candidal stomatitis is caused by the fungus Candida Albicans. You can see red spots and ulcers in the child’s mouth. A cheesy white coating can be seen on the cheeks and tongue. Often this stomatitis appears after prolonged use of antibiotics. Children complain of pain and refuse to eat.
Causes
The most common reasons:
- Presence of infectious diseases.
- Genetic predisposition.
- Increased sensitivity of the mucous membrane.
- Weak immunity.
- Lack of zinc or iron.
- Lack of vitamins.
- Injuries to the oral mucosa.
- Diseases of the gastrointestinal tract.
- Burn of the mucous membrane.
- Allergy to any food product or hygiene product.
- Caries.
- Dry mouth.
- Using the wrong toothbrush.
- Pulpitis.
- Nervous exhaustion.
- Malocclusion.
Treatment
Each type of stomatitis is treated differently depending on the cause that caused it. You should not prescribe medications yourself. Taking antibiotics for herpetic stomatitis caused by a virus will not help. But there will be wonderful prerequisites for the development of fungal stomatitis. Rinsing with antibacterial solutions for fungal stomatitis will only worsen its course. The fungus must be treated with antifungal drugs. To prescribe effective treatment, it is best to consult a specialist . Dentists in Minsk will be able to correctly diagnose and prescribe effective treatment.
At home, before going to the doctor, you can alleviate the condition by following these recommendations:
- Gently brush your teeth with a soft-bristled brush;
- exclusion from the diet of hot, sour and salty foods;
- if health worsens and the temperature rises, the child should be given plenty of water and, if necessary, given an antipyretic (in this case, a visit to the doctor should take place as soon as possible).
As a rule, doctors recommend special ointments and solutions for children, as well as medications to reduce fever or relieve pain. After each meal, be sure to rinse your mouth with water. It is important to treat children's teeth promptly.
You should not rely on folk remedies: remember, some herbal infusions and decoctions can cause a negative effect and also contribute to the development of an allergic reaction in children. Do not aggravate the situation, seek help from your dentist.
Stomatitis. What do they eat them with?
Authors : Solovyov D.V.
What is good about medicine (for a doctor ) is that it uses a specific language that is not very familiar to most patients. As a result, the doctor can talk about basically nothing, but in such a way that you will be confident in his intelligence and irresistibility. For example, when I hear that a doctor has diagnosed stomatitis, I already want to kill this pediatrician/therapist. Let me explain. First, let’s imagine a situation: a person has some kind of swelling in his mouth, he goes to the doctor, who confidently says: “Yes, you have stomatitis, father.” What are you saying, doctor, it can’t be! “Yeah, yeah, he is it, darling.
) is that it uses a specific language that is not very familiar to most patients. As a result, the doctor can talk about basically nothing, but in such a way that you will be confident in his intelligence and irresistibility. For example, when I hear that a doctor has diagnosed stomatitis, I already want to kill this pediatrician/therapist. Let me explain. First, let’s imagine a situation: a person has some kind of swelling in his mouth, he goes to the doctor, who confidently says: “Yes, you have stomatitis, father.” What are you saying, doctor, it can’t be! “Yeah, yeah, he is it, darling.
Common situation? Apparently the doctor did not make a mistake, he was able to recognize the trouble, and at the same time added to his authority. Now let's make a small insert. The fact is that the term “stomatitis” itself simply means “inflammation in the mouth.” And let’s now replace one thing with another in that very dialogue: - Yes, you have inflammation in your mouth, father. - ...
Now the conversation sounds bad, because the patient’s next phrase will most likely be completely different: “My dear, I can see for myself that there’s inflammation, what did you tell me that’s new?”
Do you feel the difference? Would you like it if, when you have a stomach ache, a doctor in a hospital happily said, “You have a stomach ache!”? We know this without you, that pain, you don’t need a doctor for that. Therefore, now remember one of the basic knowledge about stomatitis: there is no single diagnosis of “stomatitis”, there are a lot of different stomatitis. Therefore, when the doctor says that “there is stomatitis here,” this means that he is saying practically nothing, i.e. What kind of stomatitis this is, he still hasn’t figured out. True, in fairness, it must be said that many of the stomatitis are treated in the same way, but still not all, besides, knowing which one has decided to visit you is necessary not only for treatment. For example, this is necessary because some of them can be prevented or at least greatly alleviated at the very beginning.
So, the main points you need to know. The most common stomatitis is the so-called HRAS (chronic recurrent aphthous stomatitis), herpetic stomatitis and seizures.
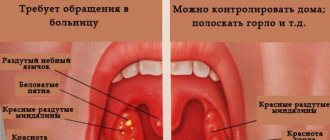
Chronic recurrent aphthous stomatitis. This stomatitis is called recurrent (i.e. recurring) because it repeats during life approximately once or twice a year (more often in children), and aphthous - because it has very characteristic ulcers - aphthae, which look something like this:
This disease occurs in approximately 20% of people (i.e., it is quite common), and has been known since ancient times. Aphthae are most often single, appearing on the lips, cheeks, in the front of the mouth, on the palatine arches, tongue, and soft palate. The lesion is surrounded by a clear stripe of redness, it is quite painful, and in children it may be accompanied by general symptoms - malaise and poor health. Most often it goes away without a trace within two weeks, and the exact cause, unfortunately, has not yet been established.
Herpetic stomatitis. Caused by the herpes virus. It begins quite abruptly, with malaise, headache and pain in the mouth, which is especially difficult for children. A characteristic sign is small bubbles filled with liquid, something like this:
I would like to draw special attention to the fact that sometimes the diagnosis “herpangina” has nothing to do with herpetic stomatitis! It's just a similar (and not very good) name.
Jams. Almost everyone knows what it is, so here, perhaps, you can do without pictures. The most common causes of its appearance are streptococcus, cadidosis or iron deficiency anemia . Or rather, in children it is anemia that needs to be put in first place. Therefore, if you see that your child is visiting, don’t be lazy and take a blood test for iron. At the same time, I would like to draw special attention to the fact that it is impossible to eliminate anemia only by taking foods containing iron! There is no need to believe the recommendations that you just need to start eating pomegranates or meat in larger quantities and the anemia will disappear. It won't disappear. Products can maintain normal iron levels only when they were normal before. Anemia has appeared - it is necessary to take iron in the form of medications. There are also other stomatitis, but they are much less common.
Basic principles of treatment. I present only those things that are common to all types of stomatitis and that everyone can and should do, and at home. Some stomatitis also has its own specific treatment, which your doctor will prescribe for you.
- Pain is the leading sign of almost any stomatitis, so immediately eliminate any irritating (spicy, sour, salty) food from your diet.
- Your main task is pain relief. The easiest way to relieve pain is to pour a solution of 2% lidocaine from an ampoule into a spoon and either rinse with it for a couple of minutes (if this is an adult or child who can rinse without swallowing), or lubricate the sore spot with a cotton swab. There are also ready-made ointments with pain relief (for example, Kamistad for adults or Kalgel for children).
- Alternatively, you can freeze an ice cube in the refrigerator and suck on it (do not give to small children!).
- I was surprised to learn that it turns out that there are chewable tablets approved by the Ministry of Health that are recommended for children with teething and stomatitis. So remember: no chewable tablets should be given to infants! The reason is that small objects (including pills) easily end up in the respiratory tract of such children.
- If it is herpes, from the very first hours start taking an antiherpes drug: (for example: Zovirax (acyclovir), famciclovir (Famvir), valacyclovir (Valtrex), etc.). Remember that the sooner treatment is started, the easier you will get off.
- If iron deficiency anemia is detected, then salvation is taking iron. However, in this case, do not expect quick results. Everything here is aimed not so much at treating existing stomatitis, but at preventing its occurrence in the future.
- In addition to painkillers, you can use drugs that speed up healing. For example, this is aekol, vitamin A (naturally, in the absence of allergies).
- It may also be easier with simple rinsing. How? Even with ordinary water. The point is to wash away food residues from the painful mucous membrane, because what exactly you will do is the tenth thing.
Some additional information.
- Many stomatitis still have an unknown cause, so it is often simply impossible to establish it for sure.
- Naturally, when there is pain, it is quite difficult to brush your teeth (especially for a child). Overcome yourself, because uncleaning can lead to the addition of bacterial inflammation of the gums, which can be very difficult to cope with.
- If you see putrefactive processes on the edge of the gums in yourself or your child (this is a grayish or greenish coating), there is a further increase in temperature or a general deterioration in the condition, immediately consult a doctor!
- If stomatitis is of a traumatic nature (i.e., it appeared from constant trauma with a prosthesis or a sharp edge of a tooth), immediately get rid of the traumatic cause, because such stomatitis more often than others degenerates into cancer.
- Quite often, stomatitis is accompanied by diseases such as influenza, scarlet fever, measles, etc. Therefore, you should not leave such things to chance, even if you feel normal. If you see something unusual, especially in a child, it is better to ask a doctor.
- If you know that you are prone to developing a “fever” (herpes), you do not need to wait until the process is in full swing. As a rule, you already know exactly a certain sensation before the bubbles appear (usually it’s something like itching), so if you feel it, immediately apply the medicine. The faster you do this, the better the effect will be (it’s not the days that are important, but the hours). Remember that 95% of the world's population are carriers of the herpes virus; science cannot yet get rid of the virus once it has entered the body.
- The appearance of stomatitis of an allergic nature at least once is a reason to forever (or at least before the course of so-called desensitization) abandon the allergen that caused such stomatitis. Don't joke with allergies, these are deadly jokes.
- If any stomatitis lasts more than two weeks, this is a clear reason to visit the doctor again.
How to prevent stomatitis? Since stomatitis is different and has a completely different nature, there cannot be uniform recommendations. Sometimes stomatitis is contagious, sometimes it is not, so just in case, until the doctor expresses his opinion, you do not need to kiss the patient, or use shared utensils and towels. And also, in any case, do not forget about hygiene and, in particular, hand washing.
What not to do and what not to use.
- There is no need to use lidocaine 10% in aerosol. It anesthetizes well, but is not suitable for repeated use, because there remains a very unpleasant sensation of burning and tightening of the mucous membrane. (Also, do not forget that small children should not be sprayed with aerosols in their mouths in principle!)
- Never apply cauterizing drugs to your mouth! Firstly, with stomatitis it is wildly painful (for some reason parents especially like to do this, not for themselves, but for the child), and secondly, it can lead to the degeneration of the ulcer into all sorts of bad things.
- There is no need to use dyes (such as blue). They do not speed up healing in any way, but they do an excellent job of hiding everything, as a result of which the doctor may miss important points.
- Maraslavin at home: is still a very popular drug, although for some reason patients most often forget to inform that, firstly, it causes an increase in temperature (which is very undesirable, especially in children), and secondly, it causes loosening of the gums, making it impossible to brush your teeth at home (a visit to the doctor is required).
I will also draw attention to such a popular medicine as Cholisal. It has a very specific taste and especially smell. Therefore, before using it in children, try it in a very small dose. If the child takes it normally, use it; if not, it’s better not to force it.
Geographic tongue (desquamative glossitis). Let's take a special look at this state. It appears as whitish or “bald” spots, constantly changing their shape, size and position. One often gets the impression that the language seems to have a constantly changing picture, a “geographical map”:
Apart from appearance, there are usually no complaints; sometimes a slight tingling sensation may appear. This condition is a normal variant and does not require any treatment at all!
I hope that now you have received at least the most general knowledge of what stomatitis is and what you should eat it with. 
And the choice, as always, is yours. 
Consultations by Dmitry Solovyov at ClubCom
published 25/11/2013 13:32 updated 15/02/2018 — Diseases of the teeth and oral cavity, Dentistry
Questions and answers
— Which doctor treats stomatitis in children?
— For diagnosis and therapeutic prescriptions, you must contact a pediatric dentist. In some cases, consultation with an allergist, immunologist, gastroenterologist, or infectious disease specialist may be required.
— Is stomatitis contagious in children?
— The contagiousness of stomatitis is determined by its etiology. Thus, viral, bacterial, and fungal stomatitis are definitely contagious, since they have a causative agent of pathogenic microflora. Traumatic or allergic stomatitis is not contagious. However, the etiology of the disease can only be determined by a pediatric dentist, and until the causes of the disease are determined, contact with the sick child should be limited: avoid sharing dishes, limit kissing, and adhere to the rules of general hygiene.
— How long does stomatitis last in children?
— The duration of the disease depends on many factors: etiology, degree of damage and severity of the disease. In mild cases, complete disappearance of stomatitis can occur within a few days; in severe cases, treatment takes several weeks.
Prevention
Preventive measures include education on general hygiene and precautions. The following preventive measures are highlighted:
- timely treatment of concomitant diseases;
- cleansing the skin of the breast before feeding the baby;
- disinfection of toys, pacifiers, bottles with chlorhexidine;
- prevention of injuries to the oral mucosa (mechanical, thermal, chemical);
- avoiding contact with other people's saliva;
- examination by a dentist at least twice a year;
- the use of special pastes that increase the protective functions of the mucous membrane;
- Teaching children oral hygiene is of great importance in the prevention of stomatitis;
- general strengthening of the immune system: healthy sleep, proper nutrition, outdoor games, physical education.
By following these preventive measures, you can reduce the risk of pathology and its recurrence.