Stomatitis is an inflammatory process of the oral mucosa, often of infectious or allergic origin. Stomatitis is one of the most common oral diseases in children of all ages, from infants to school-age children, although it can sometimes occur in adults. The special predisposition of children to this disease is explained by the fact that at a young age the mucous membrane of the oral cavity is more tender and thinner than in adults.
Types of stomatitis and causes of occurrence in children
The causes of stomatitis in children can be different, and they are directly related to the type of disease. In this section, we will look at the main types of stomatitis and their causes in children.
Herpetic viral stomatitis
This type of stomatitis is the most common and common. Sometimes this type of disease is simply called herpetic stomatitis or viral . Typically occurs in children aged 1 to 4 years.
Often infection occurs through airborne droplets. Infection with herpetic viral stomatitis is also possible through children's toys, dishes and other objects. Against the background of weak immunity, the virus enters the body and settles in the most damaged areas of the mucous membrane. Such places can serve, for example, as small wounds that appear after a child bites his lips.
Aphthous (allergic) stomatitis
This type of stomatitis is often also called drug stomatitis , since the main reason for the appearance of this type of disease is allergic reactions to various medications. It is impossible to say exactly which drugs can cause stomatitis; this is an individual predisposition, and can only be accurately determined by visiting a pediatric dentist after all the necessary diagnostics have been carried out. This type of disease occurs infrequently and, most often, in preschool children.
Traumatic stomatitis
As the name implies, this type of disease occurs after mechanical trauma to the child’s oral cavity and the entry of dirt and bacteria into these places.
Injuries can be of a completely different nature. This could be purely a dental problem. For example, due to an incorrect bite, a child may constantly bite his tongue or lips. Other types of mechanical damage to the mucous membrane include burns, for example, from food that is too hot, a pacifier that is too hard, various bad habits (pulling toys into the mouth, chewing a pencil, etc.).
Candidal (fungal) stomatitis
The main cause of candidal stomatitis is Candida fungi. Basically, this type of disease is typical for children under 1 year of age who are breastfed. Particles of mother's milk remaining in the baby's mouth after feeding provide an excellent environment for the development of this type of fungus. For this reason, sometimes this type of stomatitis is called thrush .
Infectious (microbial) stomatitis
The main reason for the appearance of infectious stomatitis in children is a decrease in immunity against the background of diseases such as tonsillitis, sinusitis, pneumonia and other diseases of the nasopharynx. This type of disease occurs in children of both school and preschool age. Infectious stomatitis develops especially often in the autumn-winter period, when the child’s immunity is weakened.
How to treat stomatitis in a child?
Stomatitis in children
Canker sores are inflammations in a child's mouth that can cause sores on the tongue, gums, cheeks, and throat. This situation is more common in children under 3 years of age, but can also occur in adolescence. In most cases, stomatitis is caused by the herpes virus, and in this case is called herpetic gingivostomatitis.
Treatment is carried out as prescribed by the pediatrician, who recommends keeping the child's mouth clean at all times, as well as using medications to relieve symptoms and, in some cases, relieve discomfort.
What can cause stomatitis in children?
Stomatitis can occur for several reasons, but the most common causes are:
- decreased immune system defenses,
- habit of putting dirty hands and objects (toys) in the mouth,
- as a result of infection with influenza viruses, herpes simplex or chickenpox, Coxsackie viruses, enteroviruses,
- candidiasis (thrush).
Other pathogens include bacteria and fungi. Temperature or mechanical trauma to the oral cavity and allergic reactions may also be the cause. Vitamin B or C deficiency plays a role.
Main symptoms
Pediatric stomatitis usually presents with symptoms such as irritability and poor appetite because when food gets into the wound, it causes pain. Other symptoms that may occur with stomatitis:
- Mouth ulcers or gum inflammation;
- Pain in the mouth and throat when swallowing;
- There may be a temperature above 38°C;
- Sores on the lips;
- Bad breath.
These symptoms can appear at the same time, but most often only the ulcers appear. In addition to stomatitis, there are other diseases that can cause mouth ulcers, such as Coxsackievirus, which causes foot-and-mouth disease. Therefore, it is important for the pediatrician to timely assess the symptoms and do tests in order to make a correct diagnosis.
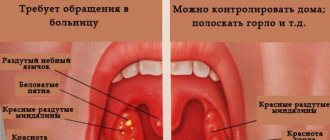
What is observed in a child’s mouth with stomatitis?
Upon examination, painful erosions, ulcers and blisters may be observed on the mucous membrane of the inner surface of the cheeks, gums, lips, tongue and, less commonly, in the back of the throat. Enlarged lymph nodes in the neck and under the jaw are also common.
The gums may be slightly swollen, red, ulcerated, and bleed easily.
When the cause of the disease is viral, oral lesions may last 7 to 10 days, although general symptoms disappear sooner.
Is it possible to easily diagnose the pathogen?
Microbiological testing can be done, but the methods used are not simple.
Samples must be transported and cultured in a suitable environment. Results will be received in approximately 15 days. Rapid diagnostic methods are also available, such as direct staining of vesicle contents with fluorescent antibodies.
Is there any specific treatment?
Treatment of stomatitis should be prescribed by a pediatrician or dentist and last about 2 weeks. However, it is important to be careful with the food your child eats and maintain proper oral hygiene to avoid the growth of microorganisms in the ulcer.
Most often, gingivostomatitis resolves spontaneously and requires only symptomatic pain treatment or antiseptics to promote local healing. In children, special attention should be paid to their hydration by offering liquids in divided form, cold or at room temperature. Sour, salty or spice-rich foods should be avoided.
Discomfort can be reduced with paracetamol or ibuprofen taken by mouth. If a yeast infection is suspected, topical application or antifungal rinses are usually effective. In some cases, the use of antiviral drugs such as acyclovir may be recommended for gingivostomatitis caused by herpes viruses. This medication helps heal sores in the mouth, but should only be used with a prescription from your pediatrician. Treatment of herpes infection with acyclovir is not required for mild infections in children with sufficiently strong immunity.
How to feed a baby or child with stomatitis?
It is important that the child’s feeding is not interrupted if there is an illness. However, it is important to be careful to avoid aggravating symptoms:
- Avoid acidic foods such as orange, kiwi or pineapple;
- Offer cold liquids such as fruit juices or smoothies;
- Eating pureed or liquid foods, such as soups;
- Choose cold foods such as yogurt, fruit compotes and gelatin.
How can you prevent stomatitis?
Infections caused by the herpes simplex virus often occur in schoolchildren. Most of these infections are asymptomatic; the virus is excreted in saliva in the absence of clinical manifestations of the disease. Children with this condition should remain at home until the end of treatment. The best form of prevention is strict hand-washing, avoiding direct skin-to-skin contact with others, and not sharing glasses or utensils.
Symptoms of stomatitis in children
Just like the causes of stomatitis in children, its symptoms are broad and also depend on the type of disease. In this section we will group the characteristic symptoms for each form of stomatitis in children.
Symptoms of viral stomatitis in children
The main symptom of viral (herpetic) stomatitis is the appearance of bubbles on the oral mucosa, which, after opening, form small erosions covered with plaque. Such erosions can be multiple in nature and located either at a distance from each other or merge together, forming large affected areas of the oral mucosa. They can be located on the lips, larynx, cheeks, tongue or roof of the mouth and are usually very painful and react strongly to touch, hot or cold food and other stimuli.
Symptoms of candidal stomatitis in children
Usually, before the onset of candidal stomatitis, the child experiences dryness of the oral mucosa, a burning sensation, an unpleasant taste and bad breath. Based on the baby's behavior, one can suspect the onset of the disease. As a rule, during this period, children are capricious while eating, behave restlessly, and sleep poorly. Further, as the disease develops, many small white dots appear, which form the affected area, covered with a white cheesy coating. In advanced forms of the disease, the plaque may turn gray. This indicates the transition of the disease to a severe form. In severe forms of candidal stomatitis, it is difficult to cleanse the mucous membrane of plaque and, at the slightest touch to the damaged area, it results in severe pain and bleeding.
Symptoms of bacterial (infectious) stomatitis in children
- The mucous membrane turns dark red; - The formation of yellow crusts occurs, which seem to stick together the lips; — The child experiences increased salivation; - Bad breath appears.
Also, depending on the infection that caused stomatitis, the following symptoms may be observed: the formation of fibrinous films, bleeding of damaged areas, severe plaque on the tongue.
Symptoms of aphthous stomatitis in children
With aphthous stomatitis, ulcers and aphthae form on the oral mucosa. Aphtha is a painful, round-shaped area of mucous membrane covered with fibrinous plaque. With aphthous stomatitis, children become lethargic, irritable, moody and complain of pain in the oral cavity. As a rule, aphthous stomatitis is chronic and can worsen 1–2 times a year.
What it is
Damage to the oral mucosa can be caused in a variety of ways. In a healthy person, minor injuries disappear quite quickly and without leaving a trace. In the presence of chronic diseases that reduce the level of immunity, any infection or dirt that gets into the wound provokes the development of inflammation.
Traumatic stomatitis is the result of a single or long-term impact on soft tissues, as a result of which painful formations appear in places of damage that are not characteristic of the normal state of the mucous membrane. These may be small blisters, ulcers, erosions, ulcers or wounds covered with a grayish or white coating.
Most often, with a single exposure and the absence of infectious contamination, such consequences of injury disappear quickly and without drug treatment. If soft tissue injury occurs over a long period of time (by braces, a sharp tooth fragment, tartar, dentures, etc.), gum inflammation and stomatitis can develop into a chronic form.
Treatment of stomatitis in children
There is no single correct treatment for stomatitis in children. Treatment is selected individually for each child after visiting a pediatric dentist and greatly depends on the form of stomatitis. Depending on the type of disease, treatment may include both local and general therapy methods.
Despite the impossibility of selecting treatment for all types of stomatitis, there are a number of recommendations that should be followed for any form of the disease. During the course of the disease, it is recommended to adhere to a strict diet that excludes eating hot or too cold foods, as well as avoiding other foods that irritate the oral cavity. Particular attention must be paid to oral hygiene. After every meal, it is recommended to rinse your mouth. For rinsing, you can use special herbs or antiseptics.
When treating the viral form of stomatitis in children, various anesthetics and antiviral drugs, anti-inflammatory ointments and gels, and immunomodulating drugs are used topically.
To treat candidal stomatitis, it is necessary to create a certain alkaline environment in the oral cavity. This is achieved by lubricating the baby’s mouth with a solution of soda or boric acid. Pharmacies also have special antifungal solutions, such as Candide. It is recommended to lubricate after every meal.
In the treatment of bacterial stomatitis, as in the treatment of other infections, antibiotics are used. Self-administration of antibiotics is strictly prohibited. Antibiotics should be selected correctly and prescribed only by the pediatric dentist, based on the sensitivity of microorganisms to certain drugs.
When treating aphthous stomatitis, oral anesthesia is used with the help of anesthetic gels, and the mucous membrane is treated with antiseptic drugs. Phototherapy using ultraviolet rays is also used. At the same time, it is recommended to carry out general immunostimulating therapy with the help of special drugs and vitamins.
Return to list of services
Causes
The causes of traumatic stomatitis may be the following:
- In children, this phenomenon is most often associated with active games and damage to the tooth or soft tissue as a result of a blow (for example, with a ball) or an unsuccessful landing on a hard object. However, this disease can also occur in infants as a result of injury to the gums by a protruding tooth.
- In the everyday life of an adult, the main cause of the onset of stomatitis can be a simple burn from hot tea. And if a person consumes very hot food and drinks systematically, such a burn and, accordingly, stomatitis, become chronic. By the way, you can get burned not only by hot food, but also by chemicals and medications used not according to instructions, acids, alkalis, and even electric shock and fire. In addition to a burn, stomatitis can also be caused by frostbite.
- Constant friction against the sharp edge of a chipped or broken tooth, poorly ground metal of braces, or poorly fitting dentures can also cause traumatic stomatitis. It is for this reason that you should not endure discomfort and pain due to the problems described above. The only correct solution would be to contact a dentist to eliminate the interference.
Another reason for the occurrence of this disease is bad habits, as a result of which the mucous membrane is injured:
- biting lips and inner cheeks;
- frequent consumption of seeds, which injures the tongue;
- haste in eating with frequent biting of the cheeks and tongue;
- the habit of holding sharp objects in the mouth and much more.
All these mechanical effects lead not only to permanent injuries to soft tissues, but also to the formation of swelling, inflammation and even ulcers.
Treatment
Like any serious disease, traumatic stomatitis requires immediate treatment. First of all, the doctor will have to eliminate the source of injury:
- In the case of a broken or chipped tooth, it is necessary to cure or remove this tooth, depending on the depth of the damage.
- Braces and dentures are improved or remade from higher quality material.
- Tartar is removed and the sharp edge of the tooth is ground down.
- If there are minor injuries, wounds and cracks are washed with antiseptics (peroxide, furacillin, infusions of calendula or chamomile).
- More serious injuries are numbed and treated with anti-inflammatory drugs.
- For quick healing of wounds, ulcers and erosions, your doctor may recommend applications with rosehip or sea buckthorn oils, vitamin A oil solution and other keratoplasties.
- In cases of thermal burns or frostbite, applications of an anesthetic drug may be necessary, but in case of a chemical burn, you must first thoroughly rinse the damaged area with a neutralizer. For an acid burn, use an alkali solution, and for an alkaline burn, accordingly, use an acid solution. And only after eliminating the traumatic substance is further treatment with antiseptics and anesthetic rinses possible.