What is mandibular nerve injury?
By this concept, dentists mean injury to one of the nerves:
- chin;
- lingual;
- alveolar.
Types of injuries include sprain, compression, crushing and rupture - partial or complete. The cause of the stretching is the long-term retraction of the mucoperiosteal flap, which is created by an implant of greater length than necessary. Crush injuries and compression are caused by needle injuries during the administration of anesthesia. Rupture occurs in two cases: when cutting the mucosa or during preparation of the hole for the implant.
Pharmacological therapy in the acute phase (first 30 hours) and intermediate phase (up to 4-8 weeks)
Pharmacological treatment of acute nerve fiber injuries includes the use of corticosteroids and non-steroidal anti-inflammatory drugs.
- Glucocorticosteroids – adrenocorticotropic hormone has been shown to inhibit central axon sprouting, reduce ectopic discharges in damaged sensory axons, and prevent neuroma formation. Seo K. et al.: Efficacy of steroid treatment for sensory impairment after orthognathic surgery. J Oral Maxillofac Surg 2004;62:1193-1201. Drug of choice - Dexamethasone - 8-12 mg/day for one week - Dexamethasone not only minimizes neuropathy after nerve injury when administered in high doses for one week after injury, but is especially recommended due to its significant anti-inflammatory effect compared to other corticosteroids. The recommendation is to prescribe a decreasing dose of dexamethasone (from high to low) for 5-7 days after a trigeminal nerve injury. Galloway EB, Jensen RL, Dailey AT, Thompson BG, Shelton C. Role of topical steroids in reducing dysfunction after nerve injury. The Laryngoscope 2000;110(10):1907-10. Kraut RA, Chanal O. Management of patients with trigeminal nerve injuries after mandibular implant placement. J Am Dent Assoc 2002;133:1351-1354.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are the best inhibitors of prostaglandin synthesis from damaged peripheral nerve endings. Prostaglandins released as a result of peripheral nerve injury sensitize peripheral nociceptor fibers and central neurons. Muller HW, Stoll G. Nerve injury and regeneration: basic insights and therapeutic interventions. Cun Opin Neurol 1998;11:557-559. Thus, maintaining therapeutic levels of NSAIDs in the blood as an adjunct to corticosteroids for 1-3 weeks after injury is very useful during the acute and intermediate phase of trigeminal nerve repair. Because any change in sensation may be caused by an inflammatory response, postoperative treatment with steroids followed by high-dose nonsteroidal anti-inflammatory drugs is given as soon as possible after any nerve injury. The drug of choice is Ibuprofen - 600 - 800 mg three times a day for three weeks (after finishing dexamethasone!). If necessary, two to three weeks after the injury, based on a repeat neurosensory examination, the doctor may prescribe an additional three weeks of taking NSAIDs if there are no signs of gastrointestinal disorders.
- Additional pharmacological agents - antidepressants, anticonvulsants, antisympathomimetic drugs, etc. Caution should be exercised with these types of pharmacological treatments, as they must be prescribed and monitored by a doctor who is familiar with the side effects of these drugs and has experience in treating nerve damage.
- Supportive pharmacological agents: - Neurorubin-Forte Lactab - one tablet twice a day for 4 weeks - contains high doses of vitamins B1, B6, B12, which play an important role in ensuring optimal metabolism in nerve cells. In high doses - has a weak analgesic effect; - Nucleo CMF Forte - one tablet twice a day for 20 days - Cytidine 5-monophosphate takes part in the synthesis of a complex of lipids that form the sphingomyelin membrane as the main component of the myelin sheath; - myogymnastics.
Causes and prevention of mandibular nerve injuries
The only cause of such damage is considered to be medical errors. Since in preparation for implantation, X-rays of the jaw are taken, which the doctor must carefully study so that when choosing an implant and a place for it, he does not injure the nerve, the injuries are caused by his unprofessionalism or negligence.
Damage to the mandibular nerve most often occurs when:
- improper administration of anesthesia - needle injury;
- choosing an implant that is too long;
- damage by an instrument - when preparing the site for the implant.
The only way to avoid such an injury is for a doctor to responsibly approach the stage of preparation for surgery, carefully studying the condition and structure of his patient’s jaw. The only way of prevention for the patient is to choose a trusted clinic and a highly qualified doctor. Specialists at the Implantmaster clinic have been able to reduce the number of injuries of this kind to 2%, since they carefully study three-dimensional photographs of a person’s jaw before implantation, and can correctly assess the condition of the bone tissue, the location of nerves and blood vessels, and select the optimal size of the implant.
Causes
The main causes of damage to the NAS are:
- implantation (doctor’s errors, lack of a full preliminary examination);
- removal of dystopic “eights” on the lower jaw;
- errors when performing conduction anesthesia;
- exit of the filling material beyond the root apex into the nerve canal;
- infectious lesion of the periapical region of the lower row.
But the most common reason is the first reason - damage as a result of implant installation, usually in the chewing area.
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Clinical picture
The pathology is accompanied by acute pain in the subradicular region of the tongue or one tonsil. The pain can spread to the soft tissues of the palate, ear, pharynx and other organs. Neuralgia has a one-sided short-term course (no more than 3 minutes).
Symptoms intensify while moving the tongue. Against the background of intense pain, the quality of life deteriorates and insomnia appears.
Other characteristic features:
- dryness of the mucous membranes of the oral cavity;
- increased salivation after an attack.
A neurological disorder can enter a stage of exacerbation and remission. Over time, the frequency of attacks increases, and the pain intensifies. Some patients report loss of taste perception.
Symptoms and stages of damage
The symptoms by which this complication can be recognized are as follows:
- numbness of parts of the head - tongue, lips, chin, cheeks, etc.;
- biting lips and tongue;
- choking while eating or drinking;
- profuse salivation.
All this creates a number of inconveniences for the patient: it makes it difficult to eat and talk, disrupts facial expressions, and also prevents men from shaving and women from applying makeup. The severity of this injury is determined by its degree: a minor one goes away on its own or with the help of drug treatment, a severe one leads to irreversible processes of nerve degeneration and is not curable. Damage to the mandibular nerve, the symptoms of which the patient observes, requires immediate consultation with a doctor - only a specialist will be able to determine its extent and provide timely assistance.
Dentists distinguish the following stages of this implantation complication:
- minor - neuropraxia;
- more severe, but partial damage - axonotmesis;
- a serious injury that leads to complete loss of sensitivity - neurotmesis.
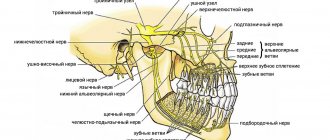
Anatomy of the trigeminal nerve
The trigeminal nerve (5th pair) is a large mixed (sensory-motor) nerve, consisting of three branches :
- Orbital (n. ophthalmicus).
- Maxillary (n. maxillaris).
- Mandibular (n. mandibularis).
The mandibular ( MF ) is the third branch of the trigeminal, innervating the skin, mucous membranes of the organs of the lower jaw, and the muscles of the lower part of the face. Its location and parameters in the human body are individual and determined by anatomical features. The nerve trunk consists of 30-80 fibers, thickness is in the range of 3.5-7.5 mm, length - 0.5-2.0 cm.
The roots of the mandibular nerve transmit information from the lower part of the face and oral cavity: teeth, gums, tongue, outer part of the ear. Motor - innervate the masticatory and part of the facial muscles.
At the exit from the skull, the LF is divided into two branches:
1. Sensitive ( anterior ) - innervating the mucous membranes and skin:
- cheeks, chin;
- floor of the mouth;
- lower teeth, jaw;
- lower lip, back of tongue;
- salivary glands (sublingual and submandibular);
- parts of the outer ear.
2. Motor ( posterior ) - ensuring coordinated work of muscles:
- chewable;
- maxillohyoid;
- suprahyoid;
- palatal-curtain;
- eardrum.
Recovery and treatment
In the first case, self-recovery takes approximately 1 month; the help of doctors is not needed, since there is no anatomical damage. Symptoms of the second appear after a while - usually 6-8 weeks, so recovery can be painful and incomplete: it will take more than 2 months. In the third stage of damage to the mandibular nerve, treatment gives results only at the beginning and is performed surgically, since we are talking about degeneration with a violation of integrity. Loss of sensitivity, which is observed in a patient for more than 3 months, indicates a high probability of losing it forever. Damage to the mandibular nerve, the consequences of which is the lack of sensitivity of the nerve for a year, leads to irreversible changes. Only the professionalism and responsibility of the doctor, which is guaranteed by the specialists of our Implantmaster clinic, can protect the patient from such unpleasant injuries.
Author:
Probability of occurrence
The mandibular nerve fascicle is a fragment of the trigeminal nerve. It provides sensitivity to intraoral and facial tissues, and is responsible for contraction of the facial muscles and dentofacial apparatus. The bundle consists of motor and sensory fibers and nuclei.
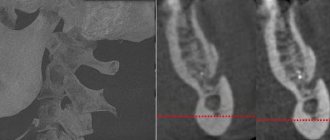
The inferior alveolar nerve (IAN) is located in the lower jaw and is one of the three endings of the trigeminal nerve. The NAN borders the root system of the mandibular arch. In this regard, there is a high risk of damage during dental treatment.
The statistics of nerve damage are especially high during the period when dental operations were performed without the use of modern technologies.
According to the latest data, the incidence of nerve damage during dental implantation does not exceed 3%. Of this number, only 1.7% end up with permanent neuropathy.
According to some dentists, these data are underestimated, and the percentage of damage to NAS reaches 30%. In any case, this issue should be given sufficient attention.
Diagnostics
First of all, the doctor conducts a survey to determine the symptoms, nature and frequency of attacks. At this stage, it is important to differentiate the pathology from trigeminal neuralgia, which has similar symptoms. When the trigeminal nerve is damaged, the spasm is localized in the periolabial region, and damage to the glossopharyngeal nerve is accompanied by discomfort in the area of the root of the tongue.
To make a diagnosis, a number of clinical studies are carried out:
- orthopantomogram (to detect elongation of the styloid process);
- computed tomography of the brain;
- magnetic resonance imaging of the vascular system.
The patient needs to consult an oncologist to rule out cancer.