A. V. KuzinCandidate of Medical Sciences, Doctor - Dental Surgeon, Department of Surgical Dentistry, Federal State Budgetary Institution Central Research Institute of Dentistry and Maxillofacial Surgery, Ministry of Health of the Russian Federation (Moscow)
Recently, there has been an increase in the number of young and middle-aged patients visiting a dental surgeon for the removal of impacted third molars. This is not just about providing them with emergency care for pericoronitis. Quite often, the patient is referred for removal of intact impacted teeth for orthodontic reasons. Clinical symptoms include: close position of teeth “bouquet symptom”, lack of space in the retromolar fossa for full eruption of the third molar, lack of dynamics in orthodontic tooth movement, relapse of bite pathology after orthodontic treatment.
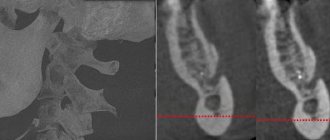
As a rule, such teeth are located inside the alveolar part and body of the lower jaw at different angles to the second painter standing in front. In most cases, a close relationship between the roots of the impacted molar and the mandibular canal is observed. In some cases, there is a risk of iatrogenic injury to the neurovascular bundle when tooth roots are dislocated. Violation of the integrity of the canal and nerve injury leads to a persistent disorder of sensitivity of the lower lip, which can last from several days to several months. Externally, facial expressions and the smile line are not deformed, but the constant feeling of “numbness” of half the chin and lower lip from the side of the extracted tooth causes significant discomfort to the patient.
Probability of occurrence
The mandibular nerve fascicle is a fragment of the trigeminal nerve. It provides sensitivity to intraoral and facial tissues, and is responsible for contraction of the facial muscles and dentofacial apparatus. The bundle consists of motor and sensory fibers and nuclei.
The inferior alveolar nerve (IAN) is located in the lower jaw and is one of the three endings of the trigeminal nerve. The NAN borders the root system of the mandibular arch. In this regard, there is a high risk of damage during dental treatment.
The statistics of nerve damage are especially high during the period when dental operations were performed without the use of modern technologies.
According to the latest data, the incidence of nerve damage during dental implantation does not exceed 3%. Of this number, only 1.7% end up with permanent neuropathy.
According to some dentists, these data are underestimated, and the percentage of damage to NAS reaches 30%. In any case, this issue should be given sufficient attention.
Causes of trigeminal neuralgia
Trigeminal neuralgia occurs due to various reasons, among which the following are common:
- Compression (squeezing) of the trigeminal nerve by vessels or neoplasms.
- Pathologies of the nervous system (multiple sclerosis, meningitis).
- Malocclusion.
- Inflammatory pathologies of the nasal sinuses.
- Injuries.
- Hypothermia.
- Viral or bacterial infections of the upper respiratory tract.
Damage to the trigeminal nerve after tooth extraction
There is also trigeminal neuralgia of odontogenic origin. In this case, the pathology is caused by diseases of the teeth, jaws or oral cavity. Sometimes such complications arise after tooth extraction.
You can suspect damage to the facial nerve after tooth extraction if pain occurs in the eye area, temporal area or nose. In this case, the trigger for pain is harmless procedures or events, for example, a gust of wind or brushing your teeth.
Important! Don't be afraid to have teeth removed when it is medically necessary. Damage to the facial nerve during tooth extraction is extremely rare. But complications in the absence of proper dental treatment occur much more often. Therefore, it is important to trust an experienced doctor, with whom the likelihood of complications is minimized.
There are two main reasons why the trigeminal nerve is damaged due to tooth extraction:
- Diagnostic error . Sometimes neuralgia is so successfully disguised as a toothache that the doctor makes an erroneous diagnosis. Instead of treating trigeminal neuralgia, the patient is treated or the tooth is removed. At the same time, the pain intensifies.
- Difficulties in dental treatment . Sometimes, when treating severe stages of pulpitis, the nerve is often injured, which causes neuralgic symptoms.
Complication after implantation
Among the complications encountered in implant dentistry is damage to the trigeminal nerve. In this case, the nerve fibers are affected mechanically (during the procedure), due to the inflammatory process or against the background of an infectious complication.
Damage to the trigeminal nerve during implantation can occur at various stages of the procedure, starting with anesthesia. Careful diagnostics using computed tomography, as well as surgical templates, will minimize the risks of complications in implantology.
Complications from the trigeminal nerve also occur with an incorrectly selected implant, when the risk of injury to nerve fibers increases. Increased pressure on the implant during installation is also fraught with damage to the trigeminal nerve.
Important! According to statistics, the likelihood of complications from the trigeminal nerve during implantation is less than 3%. At the Center of Israeli Dentistry this figure is even lower. In this case, an experienced team of doctors and careful preparation for the implantation procedure can minimize the likelihood of complications. Therefore, our patients do not need to worry about the consequences.
First symptoms
Clinical signs of damage to the mandibular nerve are expressed in discomfort in the area of innervation: the area of the mental foramen, the lower lip, the membrane of the gums and cheeks to the borders of the second molar.
Pathology is expressed:
- Paresthesia – change in sensitivity (no painful sensations during injection, etc.).
- Dysesthesia is a change in sensitivity that brings discomfort (pain, “pins and needles”).
- Anesthesia – complete loss of sensitivity.
When extracting wisdom teeth, the lingual nerve is most often damaged (up to 2.1%). During implantation, damage to this nerve is less common and manifests itself with the following symptoms:
- increased salivation;
- speech defects;
- involuntary tongue biting;
- problems with swallowing;
- loss or change in taste;
- burning sensation of the tongue;
- numbness of the mucous membrane of the tongue and gums.
Up to 90% of lingual nerve injuries heal on their own within 7-10 weeks of onset.
Classification of manifestations
According to Seddon's classification, injuries to the trigeminal nerve are of several types:
- Neuropraxia. The damage is reversible. The sheath of the nerve fibers is not affected. There is no degeneration. Sensitivity returns a few weeks after treatment.
- Axonotmesis. Requires long-term therapy for up to six months. Fiber damage occurs and degeneration develops. The damage is reversible.
- Neurotmesis. Nerve structures, fibers and connective membranes are affected. Scars form. The pathological process is irreversible. Surgery is required.
According to the WHO classification, there are five categories of NAS lesions:
- compression or traumatic injury;
- edema;
- gap;
- final break;
- post-traumatic fibrosis.
Assessing the complexity of a clinical situation
To diagnose neurological pathologies, two research methods are used:
- Mechanoceptive. The tissue response to mechanical action and stimulation is recorded.
- Two-point irritation.
- Brush test.
- Nociceptive. Determine the perception of pain.
- Using a pin.
- Temperature test.
You can determine a taste deficiency by using a cotton pad with sugar or salt.
Research is carried out simultaneously on the affected and healthy sides of the maxillofacial apparatus.
Symptoms are documented. Areas of neurosensory deficit are measured with an accuracy of 1 mm.
Therapy concept
Medical tactics for pain and discomfort:
- Monitoring the patient and tracking the dynamics of the condition over a certain period of time.
- Drug therapy. The use of painkillers, hydrogen pump blockers, glucocorticosteroids and other drugs.
- Removing or unscrewing the rod several turns. It is carried out within 24 hours after implantation. The critical period of treatment is three months. It is during this period that improvement should occur.
- Carrying out a microsurgical operation.
There are no strict treatment protocols. The doctor selects the best option based on practical experience and knowledge.
It is generally accepted that the clinical result of the operation is achieved only if it is performed within a year after implantation.
Surgery
Indications for the operation:
- Confirmed nerve damage.
- Persistent sensory impairment for three months.
- Pain due to a pinched nerve.
The result of surgery depends on certain factors:
- Time elapsed from injury to surgery.
- Type and severity of manifestations.
- Features of blood supply in the pathological zone.
- Proper selection and preparation of the rod.
- The general health of the patient.
- Age.
- Presence of tension zones.
- Experience and practical skills of the surgeon.
Speed of diagnosis is key. Especially with minor damage. Late diagnosis threatens the formation of carpal tunnel syndrome.
Post-traumatic sensory nerve damage. Terminology.
The Association for the Study of Pain has standardized a nomenclature system that defines the most commonly used neurosensory descriptive terms Classification of Chronic Pain, Second Edition: International Association for the Study of Pain Task Force on Taxonomy, ed.: H Merskey and N. Bogduk. IASP Press IASP Council in Kyoto, November 29-30-2007.
- Paresthesia is a non-painful altered sensation. May be described by patients as a pins and needles, slight burning or tingling sensation. NEW sensations - stretching, pulling sensations.
- Dysesthesia is perverted sensations. Abnormal, sometimes unpleasant sensations experienced by a person with partial damage to sensory nerve fibers when touching the skin. - Unpleasant abnormal sensation, spontaneous or provoked. Note : Dysesthesia is not pain when it hurts or paresthesia. Special cases of dysesthesia are hyperalgesia and allodynia. Dysesthesia should always be unpleasant , and paresthesia should not be unpleasant, although it is recognized that the boundary can create some difficulties when it comes to whether these sensations are pleasant or unpleasant. It should always be stated whether the sensations are spontaneous or provoked.
- Neuropathic pain (IASP) is pain caused by damage or disease of the somatosensory nervous system.
- Neuropathy (IASP) is a dysfunction or pathological change in a nerve: in one nerve - mononeuropathy; in several nerves - mononeuropathic multiplex; if diffuse and bilateral - polyneuropathy. Note : Neuritis is a special case of neuropathy and is currently a term reserved for inflammatory processes affecting the nerves. - sensitive (touch, heat, pain) - motor (movement).
- Allodynia is pain from non-noxious stimuli (pain with light touch/cold/heat). The appearance of pain in response to a stimulus that does not cause pain in healthy people. Thermal allodynia, especially cold allodynia, is a feature of the extraoral dermatome in patients with IANIs. Some patients report decreased taste and heat sensitivity. Perversion of sensitivity is characterized by an increased threshold of sensitivity and increased duration of perception, lack of precise localization of sensations of an unpleasant nature, and a tendency to irradiate. The pain continues when the stimulus is removed.
- Hyperalgesia - increased sensitivity to painful stimuli
- Anesthesia - numbness
- Hyperesthesia and Hypostesthesia are terms that are often used to describe changes in sensitivity that increase or decrease, respectively.
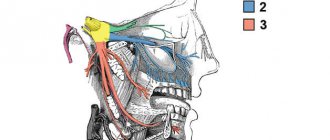
Rice. 5 Anatomy of the II (maxillary) and III (mandibular) branches of the trigeminal nerve. It is important to note that the branches of the superior alveolar nerve retrogradely “merge” into the infraorbital nerve, which explains the symptoms of swelling and pain in the infraorbital region when the superior dental plexus is damaged.
Post-traumatic sensory neuropathy is pain that develops after medical intervention (surgery, treatment, anesthesia), with a minimum duration of 2 months, while other causes of pain are excluded (infection, persistent malignancy, misdiagnosis, etc.), preoperative pain from others must also be excluded reasons.
It is important to add that the neuropathic area does not have to be clearly indicated by the patient, however, about 80% of patients can localize and indicate the neuropathic area.
HERE you can read more about the incidence of “phantom toothache” (atypical odontalgia) after endodontic treatment, which is classified as persistent dentoalveolar pain (PDAP type 2) and occurs in up to 3% of cases.
You should immediately consult a doctor if:
- pain intensifies or persists for more than 24 hours;
- bleeding from the socket intensifies or persists for more than 12 hours;
- one or more sutures placed by a doctor are lost;
- there was a putrid odor from the mouth;
- it is difficult or painful to open your mouth;
- the increase in body temperature is significant (more than 39 degrees Celsius) or persists for more than 24 hours;
- swelling increases or persists for more than 3 days;
- mobility of adjacent teeth occurred.
Our contacts
Top Contents
- How to remove a tooth
- Wisdom tooth removal
- Root removal
- Recommendations after removal
In dentistry, there are specific indications that explain why a tooth should be removed, the main one of which is to prevent the development of inflammation, loss of adjacent teeth and general infection of the body. If you have the following conditions, your doctor will recommend extraction surgery:
- complete destruction of the crown and root;
- crown fracture;
- advanced pulpitis;
- severe periodontal damage;
- mobility grades 3 and 4;
- purulent processes (flux, cyst formation at the root apex);
- incorrect positioning, which leads to injury to the cheek or tongue;
- correction of the bite when one element interferes with others, including before installing braces.
The final decision on whether a tooth needs to be removed is made by the doctor after examination and x-ray diagnostics. If there is a possibility of restoration, the dentist will definitely use it, since the tooth-preserving approach is the basis of dental treatment.
Often the question of whether to remove or treat a tooth arises in pregnant women, since surgical intervention during this period has an extremely adverse effect on the development and health of the fetus. Doctors prefer symptomatic treatment, which alleviates the condition and allows you to delay the time before childbirth. Removing a tooth while breastfeeding is not dangerous, and the operation does not carry any risks.
Extraction is not performed if there are contraindications:
- acute infectious diseases;
- bad feeling;
- Drunk;
- mental disorders;
- inflammatory diseases of the oral cavity, etc.
If you have chronic diseases or diseases that require special treatment, check with your doctor whether a tooth can be removed in your case. The dentist must be aware of possible risks and take all measures to prevent them.
How long can your gums hurt after tooth extraction?
Severe pain that interferes with normal life activities lasts no more than 3 days after the surgical procedure. It will take up to 7 days for the discomfort to disappear completely. For complex removal, this period increases to 2 weeks.
If during the rehabilitation period you feel pulsation in the socket, bleeding, or bad breath, then you need to contact a surgeon at the Cerekon clinic as soon as possible, because all these signs signal the development of inflammation.
What should you not do during the healing period?
- It happens that after a tooth is removed, the doctor puts sutures - under no circumstances should they be touched with a brush for the first week or even two after the operation.
- Do not rinse your mouth on the first day after surgery.
- It is strictly contraindicated to create increased pressure in the mouth - when sucking from tubes, sucking secretions from a wound, etc. This can quickly restart heavy bleeding.
- After the first two weeks, you can brush your teeth with a soft brush without touching the socket.
- In the first days, you can only eat soft or semi-liquid food, and later you cannot chew on the side where the tooth was removed.
- Do not touch the hole with your tongue.
- It is better to stop smoking for the first three days of healing, if possible. In addition, you should not use alcohol or alcohol-containing tinctures of medicinal plants for rinsing your mouth.
How to remove a tooth
There are two extraction methods used in dentistry: simple and complex. Their choice depends on which teeth are being removed - premolars and molars with tangled branched roots are removed using a complex method. It is very difficult to pull out such elements entirely due to the fact that the tooth socket is penetrated by retaining ligaments and alveolar processes. Errors during the procedure or insufficient experience of the specialist lead to serious complications. Therefore, even despite the acute condition, always find out in advance where you can have a tooth removed from a good doctor with positive recommendations.
Factors complicating the operation:
- complete destruction of the coronal part;
- high fragility;
- acute inflammatory diseases;
- Unerupted or misaligned wisdom teeth.
The technology of the procedure depends on which teeth are removed. In some cases, tissue incision and suturing are performed.
Doctors providing this service
Tooth extraction is an extremely painful undertaking that causes a great deal of stress for most people. When the operation has already been performed, you can breathe more freely - all that remains is to follow fairly simple recommendations during the recovery period. After tooth extraction, a swollen and sharply painful wound remains in the mouth for some time, which interferes with eating. The timing of its healing depends on the general condition of the body, but the average period is considered to be 2-3 weeks. If a single-rooted tooth was removed, the hole heals in about 16 days, and if it is multi-rooted, it takes about 22 days. In addition, the length of the postoperative period depends on several other factors, for example, a young body heals such damage faster.
Ways to relieve pain and inflammation
The safest and most effective way to reduce the pain and swelling that occurs after tooth extraction is to apply a cold compress to the cheek. If this measure does not bring the desired effect, then it is recommended to take analgesics: analgin, ibuprofen, ketanol, diclofenac, etc. The dosage regimen of the drugs is indicated in the instructions for them.
After complex extractions, patients are additionally prescribed antibiotics, since in these cases there is a high probability of developing purulent and inflammatory processes.
Important information! It is strictly forbidden to rinse your mouth for 7 days after removal of the chewing organ. This manipulation leads to the washing out of the blood clot from the socket.
Wisdom tooth removal
Wisdom teeth are considered full-fledged elements of the oral cavity. They are involved in chewing food (if they are located above each other and have contact), and can act as a support for bridges and removable dentures in the future. There are specific indications for extraction in their case. For this reason, the decision about whether wisdom teeth need to be removed is made only by the attending physician.
The most common problem with eighth teeth is their growth. Only some teeth form and grow completely without complications, but often these processes are accompanied by a number of difficulties:
- semi-retinated or impacted elements that have formed in the bone tissue, but have not erupted or only partially erupted. Their position can be vertical, horizontal, or with their roots outward. Because of this, neighboring elements suffer, constant pain appears;
- violation of position (dystopia). Since wisdom teeth erupt without predecessors (baby teeth), and the jaw bone is already formed and does not develop, the position of the elements is often incorrect. They injure the mucous membrane, overlap other crowns, and put pressure on neighbors. This leads to inflammation. The doctor will determine whether the position can be restored with orthodontic treatment or whether it is better to remove the wisdom tooth;
- appearance of a gingival hood. When slowly cutting through the mucosa, an area is formed in which bacteria and food debris accumulate, which are difficult to clean. This leads to acute inflammation, which can provoke the appearance of pus;
- destruction, caries. Elements may appear immediately underdeveloped with carious lesions.
The doctor determines whether wisdom teeth should be removed or not based on complaints and the clinical picture. Problems with even one or two teeth interfere with the normal functioning of the entire dental system. Pain appears when opening the mouth and chewing. The bite and position of the incisors may even change.
How a wisdom tooth is removed depends, as in the case of permanent elements, on the condition of the dental system. In the absence of contraindications, manipulation is carried out with ordinary forceps.
Oral care after tooth extraction
In the first two weeks, it is better not to brush your teeth at all, as this may resume bleeding and disrupt the entire healing process. Instead of brushing, you can rinse your mouth with hot water and clean your teeth with your finger until a characteristic squeak occurs. After this, be sure to rinse your mouth with special disinfectant solutions prescribed by your doctor. It should be borne in mind that frequent (more than three times a day) rinsing your mouth only slows down the healing process.
If the tooth was removed during the acute stage of the inflammatory process, then the healing of the hole takes longer and is much more painful. In this case, the doctor may prescribe oral or local use of anti-inflammatory drugs. Antibiotic mouth rinses should be alternated periodically to prevent bacteria from becoming accustomed to a particular drug. Lubricating the hole with the juice of the medicinal plant Kalanchoe works well - it gives a very strong analgesic and healing effect - often the wound heals within a few days. To increase biological activity, a plucked Kalanchoe leaf can be kept for 5 days on the bottom shelf of the refrigerator, preventing it from freezing.