Inflammatory gum disease in adults and children is called gingivitis. It is most often observed in children a few months from birth to 13 years of age, which is explained by the characteristics of the child’s body and poor oral hygiene.
According to statistics, in a child from 2 to 4 years old, gum inflammation occurs in 2% of cases, and by the age of 13, the proportion of this disease in children reaches 80%. Gingivitis cured in time does not become chronic, but if left untreated it can cause the development of periodontitis.
Causes of gingivitis in children
There are many causes for childhood gingivitis. The gums become inflamed due to the functional immaturity of their tissues. In babies under one year of age, the cause of the disease is often teething, when the gums become red and sore. Sometimes inflammation is caused by an allergic reaction to food.
In adolescents, the disease may manifest itself due to the eruption of a permanent tooth. When soreness during brushing does not allow this procedure to be performed efficiently, microbes multiply and gum inflammation develops.
The most common factors that provoke the development of gingivitis in older children are:
Action of microbes
In 90% of cases, the disease appears in a child due to insufficient oral hygiene, as a result of which microorganisms multiply intensively, plaque and tartar form, and stomatitis develops.
Mechanical injury
The integrity of the mucous cavity can be compromised by teething, cuts, scratches, burns, biting, improper brushing of teeth, and eating solid foods.
Foci of infection in the oral cavity
If children have carious teeth, there is a chance that they will develop infectious gingivitis, which affects the gums. Therefore, teeth that require treatment must be treated as soon as possible.
Excessive loads on the dental system
Other causes of gum damage in children may include:
- presence of malocclusion;
- poor nutrition with a lack of vegetables and fruits;
- uneven load on the dental system due to bad habits;
- defects of the oral cavity (short frenulum of the tongue, lips);
- the presence of caries, various infections;
- thermal burn from hot food;
- wearing braces.
Diagnosis and treatment of oral lesions in newborns
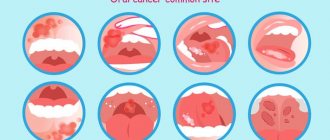
Infants often develop lesions in the oral cavity, which cause discomfort for themselves and cause anxiety for their parents. The most common disorders and diseases include congenital and neonatal teeth, various oral mucous cysts in newborns, ankyloglossia and congenital epulis of the newborn. In this article we will look at the features of diagnosis and treatment of this type of disorder and try to give readers an idea of the correct methods of treating and counseling young patients and their parents.
During their practice, doctors encounter various cases of oral lesions in newborns: from physiological characteristics associated with the development of the child to cancerous tumors. Awareness of such disorders plays an important role in correct diagnosis, counseling and treatment planning. The purpose of this article is to inform healthcare professionals about the diagnosis and treatment of the most common oral disorders in newborns.
Congenital and neonatal teeth
The eruption of the first baby tooth occurs approximately six months after the baby is born. But some babies reach this age already having congenital (the baby is born with them) or neonatal (erupted during the first month of life) teeth in their mouths.
Almost all congenital teeth (about 90%) erupt in the incisor area of the lower jaw. As a rule, they have the correct shape, but may be characterized by discoloration and an uneven surface. Their typical distinguishing feature already during the development period is increased mobility due to the absence or short length of roots. Most of the congenital teeth are subsequently included in the row of twenty primary teeth, but about 10% of them turn out to be supernumerary. Congenital teeth are rare: one case in two to three thousand births of healthy children, and, as a rule, this deviation is random. But in some cases, the appearance of congenital teeth can be a symptom of certain syndromes, malformations and gingival tumors.
If the congenital tooth turns out to be supernumerary and is not included in the row of baby teeth (this can be determined using an x-ray) or interferes with breastfeeding, it is recommended to remove it. Excessively mobile teeth should also be removed to prevent possible aspiration. In addition, congenital teeth can cause traumatic ulceration of the ventral surface of the tongue (Rigi-Fede syndrome), but this disorder is not an indication for tooth extraction and is cured by smoothing the rough cutting edge of the congenital tooth.
Newborn cysts
To refer to oral mucous cysts in newborns, many terms are used that replace each other, causing some confusion. But, based on the different histogenesis of the lesions, all of them can be divided into two categories: palatal and gingival.
Palatal cyst of a newborn
The palatal plates are bilateral rudimentary processes that join along the midline of the oral cavity in the eighth week of fetal development to form the hard palate. They also fuse with the nasal septum, resulting in complete separation of the oral and nasal cavities. In this case, the connective epithelial lining between the plates is destroyed under the action of enzymes, providing the possibility of fusion of the connective tissue. Neonatal palatal cysts, or Epstein's pearls, form from epithelial inclusions along the fusion line of the palatine plates. This disorder is characterized by high prevalence and is observed in 65%-85% of newborns. Cysts are small (1-3 mm) yellow-white bumps along the palatal suture, especially often located at the junction of the hard and soft palate. Histological examination reveals that these cysts are filled with keratin. No special treatment is required, since the cysts atrophy and disappear soon after their contents are removed.
Gingival cysts of newborns
Gingival cysts develop from the dental lamina (ectodermal ligament), which serves as the basis for the formation of primary and permanent teeth. Its remains can proliferate to form small cysts and subsequently cause the development of various odontogenic tumors and cysts. Depending on the location of formation, cysts that appear on the gums of newborns are called Bohn's nodes (present on the buccal and lingual surfaces of the alveolar ridges) or gingival cysts (formed on the process of the alveolar ridge).
Neonatal gingival cysts have a high prevalence: for example, Taiwanese infants screened within three days of birth had a 79 percent prevalence of the disorder.
Typically cysts look like small whitish lesions of constant size. Those that form on the anterior ridge of the lower jaw can be mistaken for congenital teeth. No separate treatment is required as cysts often rupture due to secondary trauma or friction.
Ankyloglossia
The term “ankyloglossia” (tongue-tied) describes the clinical situations of fusion of the tongue with the floor of the oral cavity or insufficient length of the frenulum of the tongue, limiting its mobility. Ankyloglossia can occur in representatives of various age groups, but is most often observed in newborns. According to research, the frequency of this disorder in newborns ranges from 1.7% to 10.7%, in adults – from 0.1% to 2.1%. Based on this, it can be assumed that some milder forms of ankyloglossia resolve with age.
Ankyloglossia of an infant can cause difficulty in breastfeeding and even cause pain in the nipple area for its mother or wet nurse. The preferred treatment for this disorder in newborns is simple frenectomy, where the frenulum is cut off at its thinnest point with small scissors. The procedure can be performed under superficial anesthesia, which ensures minimal discomfort and reduces the likelihood of bleeding. But bleeding is not necessary. Thus, according to the results of a study involving 215 newborns who underwent frenectomy without anesthesia, 38% of children had no bleeding, and 52% had only a few drops of blood. In 80% of cases, nutrition improved within 24 hours after the start of the procedure.
Congenital epulis of the newborn
This disease is a rare tumor of unknown histogenesis. As a rule, the lesion forms on the alveolar ridge of newborns. The course of the disease is as follows: the tumor does not increase in size from the moment of birth, sometimes it can decrease over time, which indicates a reactive rather than a neoplastic etiology. Most often, this tumor is found in the frontal part of the alveolar ridge of the upper jaw and has the appearance of a round attached formation, usually less than 2 cm in diameter (but sometimes larger ones are found), with a smooth lobulated surface. These types of tumors are more common in girls, which may indicate the influence of hormones, although estrogen and progesterone receptors have not been identified. In 10% of cases, multiple lesions may occur, confirming the need for a thorough oral examination.
As a result of histological studies of congenital epulis, large granular cells with small nuclei were identified. Unlike granular cell tumors, staining with the S100 protein antigen in congenital epulis gives a negative result. Other markers of neurogenic origin also showed negative results, confirming a nonspecific mesenchymal origin of the tumor. Surgical removal is recommended for the treatment of congenital epulis, especially if there is difficulty breathing or feeding problems, or if there is a need for histological confirmation of the diagnosis. For smaller tumors, a wait-and-see approach is acceptable, since cases of spontaneous regression of the tumor are known. There were no cases of relapse, even with incomplete removal of the tumor, or malignant degeneration.
Authors:
Van Heerden, Van Zyl
Symptoms
Gingivitis has a main symptom by which it is easily identified - inflammation affecting the child’s gums. The process begins with a slight redness that quickly gains strength. This signal often goes unnoticed by parents, and children go to the dentist with an active inflammatory process, bright red swollen gums, burning, and pain. These signs indicate that the disease has entered an acute phase.
Children suffer most from the catarrhal form of this disease, which can be chronic or acute. In the first case, the symptoms are not pronounced, pain occurs only when brushing, there is slight swelling, redness, and cyanosis of the gums.
A sign of an acute form of the disease is intoxication of the child’s body. It manifests itself as headache, nausea, lethargy, and fever.
The most complex type of disease, ulcerative gingivitis, manifests itself as follows:
- the inflammatory process progresses;
- their structure changes;
- there is an unpleasant odor from the mouth;
- lymph nodes in the neck enlarge;
- saliva is produced profusely;
- the skin turns pale.
If these signs are left unattended, an ulcerative-necrotic form of the disease may occur, when necrotic areas with a gray-green coating and a putrid odor appear on the gums, saliva becomes viscous, body temperature rises and the general condition significantly worsens.. All this indicates severe intoxication in organism.
During puberty in a teenager or if he has problems with hormones, hypertrophic gingivitis occurs. It occurs due to improper orthodontic treatment of dental anomalies. The inflammatory process is accompanied by increased growth of gingival tissue, which leads to partial closure of dental crowns. This form of the disease is usually localized. One or two gums are affected, sometimes the affected area expands. The most common location is the lower anterior incisors and canines.
Atrophic gingivitis does not have a pronounced inflammatory process and occurs without pain, although over time it can be complicated by periodontal disease.
Causes
The cause of the development of the pathology is the herpes simplex virus type 1. It belongs to DNA viruses belonging to the Herpesviridae viral family. The pathogen multiplies rapidly in the epithelial cells of the oral mucosa. Then it enters nearby lymph nodes (submandibular) and continues to reproduce in them. Then it enters the blood and migrates to the parenchymal organs (spleen, liver, kidneys). There it multiplies and enters the bloodstream again. As a result, it again appears in large quantities in the epithelial cells of the skin and mucous membranes. They are massively defeated. It is localized in the oropharynx, oral cavity, nose, lips, and nearby skin. Stomatitis and herpes of the skin and mucous membranes develop when the infection generalizes simultaneously.
Children become infected with it as follows:
- through contact and everyday life (using shared utensils, toys, through kissing);
- airborne (coughing, sneezing);
- from a sick mother to the fetus through the placenta or during childbirth.
A baby can become infected from sick adults, children, and carriers.
The following factors contribute to the development of the disease:
- previously suffered inflammatory processes;
- previous antibiotic therapy;
- deficiency of microelements and vitamins in the body;
- mechanical damage to the skin and mucous membranes;
- insufficient fluid intake;
- poor oral hygiene.
In children, the virus is especially easily transmitted through contact. The infectious process quickly spreads to healthy areas.
Diagnostic methods
The diagnosis is made by a doctor based on the results of studying the medical history and life of the child in combination with a dental examination. The patient’s complaints, the presence of somatic diseases, and whether he is taking medications that may cause the development of gingivitis are clarified.
Then the doctor conducts an external examination, paying attention to maxillofacial anomalies, the condition of the teeth and gums, and makes a diagnosis. The dentist does not require the help of other specialists, since the disease clearly manifests itself externally and does not require instrumental examination.
Prevention
To prevent the occurrence of pathology, preventive measures should be taken.
- The baby’s mouth should be cleaned after any meal and rinsed with boiled water.
- Mother and child should eat a balanced diet.
- It is necessary to protect the baby from kissing people who have sore gums, from traumatic games, and from chewing objects with sharp edges.
- Pacifiers, toys, bottles should be perfectly clean, like the hands of a toddler.
- See your dentist regularly for preventative checkups.
- The baby must use a separate towel and utensils.
Treatment
Treatment for childhood gingivitis is practically no different from how adults are treated. Only medications used for them are softer and more gentle. Treatment begins with professional cleaning of hard deposits and plaque of tooth enamel - mechanical or ultrasonic.
If caries is detected during the examination, then therapeutic treatment is carried out. Gingivitis is then treated with medications with antiseptic and anti-inflammatory properties. Measures are taken to eliminate detected pathologies (bite, frenulum, etc. are corrected).
Ointments and gels are considered effective for children under 4 years of age. For example, Cholisal ointment has analgesic and anti-inflammatory properties, which makes it possible to prescribe it to alleviate the patient’s condition, especially when baby or permanent teeth are cutting. Ointments and gels are applied directly to the inflamed area.
Antibiotics in tablets or in the form of injections are prescribed to children in difficult cases (the presence of infections of bacterial origin in the body). At elevated temperatures, rinses, drinking plenty of fluids, antioxidants, antipyretic drugs for children, and taking vitamins are prescribed.
Prevention measures should include regular visits to the pediatric dentist, training in oral care rules, and parental monitoring of the development of hygiene skills.
Symptoms
Oral candidiasis in children can have different forms of manifestation and severity of symptoms: mild, moderate and severe. As a rule, each form corresponds to the stage of development of the disease. If therapy is not carried out in a timely manner, the signs of fungal infection become more intense and the number of symptoms increases.
In mild forms of the disease, a red rash appears on the oral mucosa, which is covered with a white coating on top. At the next stage, the child experiences swelling of the tissues and the formation of localized white spots with a coating of curd consistency. Gradually these spots merge into a larger affected area. When plaque is removed, bleeding ulcers open. If thrush starts, the fungus spreads to the entire oral cavity, including the lips, tongue and throat. All fabrics are completely covered with a curd coating.
Common symptoms of candidiasis in children include:
- burning and itching sensation in the mouth;
- discomfort and pain when eating;
- frequent regurgitation in babies;
- formation of cracks in the corners of the lips;
- temperature increase.
Children in the first two years of life report their condition by refusing to eat, constant whims and crying for no reason. It is not difficult to see the signs of candidiasis, so if a child has a sharp rise in temperature or refuses to eat, pediatricians and dentists recommend checking the oral cavity for the presence of white plaque. If you suspect thrush, it is not advisable to delay a visit to a specialist, since the fungal infection progresses quickly.