Causes of mucositis after implantation
In the oral cavity, the disease usually develops due to chemotherapy or improper implantation. The following medical errors can provoke the appearance of mucositis:
- Incorrectly selected dental implant. Leads to uneven load and loosening of the abutment. Subsequently, the load on the bone increases, inflammation appears, and the hard jaw structures lose volume.
- Gaps between the abutment and the implant or crown. The joints are most vulnerable to bacterial penetration. It is very difficult to achieve absolute tightness, so implant manufacturers are constantly improving the connection system.
- Excessive screwing of the implant into the bone can lead to its destruction.
- Infection during surgery.
- Incorrect calculation of loads on the prosthesis and implant.
- Incomplete patient history.
- Inappropriate prosthetic technique - the success of the operation depends on the qualifications and experience of the specialist.
- Inadequate oral hygiene in the postoperative period.
- Periodontitis and pyorrhea are diseases that lead to inflammation of the tissue around the crown.
- Nicotine addiction.
Degree of complications
Side effects are classified according to severity as follows:
- 0 degree - no manifestations;
- 1st degree - minor manifestations that do not change the quality of life;
- Grade 2 - moderate symptoms that force the patient to limit activity; it is difficult to cope with them without treatment;
- Grade 3 - severe manifestations requiring hospitalization;
- Grade 4 - life-threatening requires emergency treatment measures.
For each cytostatic drug, grade 3-4 toxicity is calculated as a percentage, but the use of drug combinations can lead to unplanned consequences.
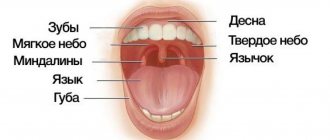
Clinical signs of disease on the gums and soft tissues of the mouth
Mucositis is the first stage of implant rejection, in which only soft tissue is affected. When there is inflammation of hard tissues, we have to talk about peri-implantitis. Oral mucositis is characterized by characteristic manifestations such as:
- expansion of capillaries (erythema), are a consequence of inflammation;
- swelling of the affected area, hyperplasia;
- tissue death of the oral mucosa, expressed by white spots;
- thinning of the mucous membrane;
- the formation of small ulcers located in several places at once: on the gums, palate, and the inside of the cheeks;
- infection of ulcers, which is accompanied by suppuration.
Oral mucositis also has systemic manifestations:
- increased body temperature over a long period;
- pain;
- discomfort while eating, talking;
- loss of appetite, weight loss;
- inflammation of the submandibular lymph nodes;
- itching, dry mouth.
Reviews
Oral mucositis is a fairly common phenomenon that occurs in patients undergoing cancer treatment.
Proper oral hygiene, a properly selected diet and timely administration of medications can quickly relieve the painful syndrome and prevent the progression of the disease.
If you have had to deal with mucositis of the oral mucosa, share your experience of getting rid of the disease in the comments to the article.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags medicines oral cavity
Did you like the article? stay tuned
No comments yet
Stages and criteria of toxicity
According to WHO, mucositis develops in stages:
- Stage zero is the absence of characteristic signs of the disease. In medicine, this stage is called incubation, since the infection is only gaining momentum.
- The first stage is accompanied by redness and the appearance of small ulcers. During eating and talking, discomfort is felt due to isolated lesions of the oral mucosa. Patients often complain of itching in the mouth. The patient's condition is satisfactory.
- The second stage - the number of redness and ulcers increases. There is pain when talking, chewing and swallowing.
- The third stage - ulcerative lesions rapidly spread throughout the oral mucosa, swelling appears. To prevent damage to the affected areas, it is advisable to eat only soft or liquid foods.
- The fourth stage is the most severe degree of the disease. Accompanied by severe constant pain and intense bleeding. Nutrition is possible only by probing.
The disease requires urgent medical attention and, if not provided, can be fatal.
What it is
Oral mucositis is a common and quite dangerous disease. This is a peculiar reaction of the body to a number of negative factors, the main of which is a pathological complication in patients after undergoing chemotherapy.
It is accompanied by extensive local inflammation of the mucous tissue, which greatly interferes with food intake, complicates the swallowing process, even when it comes to soft foods and liquids, which has an extremely negative effect on the general condition of the body - sudden weight loss occurs, and as a result - anorexia.
Risk factors for developing mucositis
- Failure of metabolism, disturbances in the gastrointestinal tract;
- weakened immunity due to past illnesses;
- stomatitis in the chronic stage;
- untimely treatment of dental diseases;
- allergies to medications: antitumor antibiotics (Mitomycin, Vinblastine, Dactinomycin);
- antimetabolic drugs (Thioguanine, Fluuracil, Cytarabine);
- alkylating drugs (Cyclophosphamide, Cisplatin, Temodal).
Diagnostics of the oral cavity
The specialist’s task is to make a differential diagnosis. It is necessary to exclude other diseases with a similar clinical picture:
- aphthous, gangrenous stomatitis;
- acute necrotizing stomatitis, which occurs due to the active proliferation of bacteria and the inability of the immune system to resist infection;
- fungal infection - oral candidiasis, etc.;
- herpes virus, manifested by white spots;
- mechanical damage to the mucosa during adaptation to dentures.
For diagnostic purposes, the oral cavity is sanitized, laboratory blood tests and culture of inflamed tissue are prescribed. The origin of the pathogen is determined and an effective treatment option is selected. Sometimes a CT scan of the mouth is performed.
Treatment of complications
Traditional treatment of complications is not always possible. Vomiting is well controlled, medications cope well with leukopenia, with a high probability of 3-4 degree inhibition of the white blood sprout and before the appearance of leukopenia, the introduction of colony-stimulating factors begins in advance.
There are no specific drugs to relieve the neurotoxicity of chemotherapy, so there is an urgent need for physical therapy and various neurorehabilitation techniques.
In case of complications from the gastrointestinal tract, mainly mucous membranes and the liver, only symptomatic treatment is possible, which is why the professionalism of the medical team and the clinic’s capabilities in organizing intensive care and conducting auxiliary rehabilitation treatment, and selecting adequate nutrition are so important.
Complex of medical care
Treatment should be comprehensive, including mechanical cleaning with mucosal disinfection and antimicrobial therapy. The course lasts for two weeks.
What drugs to treat
The stage of the disease and the complexity of its course influence the choice of medications. To alleviate the patient’s condition, prevent additional infection and rapid wound healing, the following drugs are used:
- iodine-containing rinse solutions;
- local action gels (Cholisal-gel);
- local corticosteroids (gels, solutions based on Dexamethasone);
- anesthetics (Lidocaine, Trimecaine) for severe pain;
- group of biological drugs (Filgrastim, Palifermin);
- Interferon - for antiviral therapy;
- products with aloe extract, zinc.
Treatment protocol
In case of transition of mucositis to peri-implantitis, a surgical protocol is indicated during treatment:
- the size of the affected area is visually determined;
- the surface of the implant is cleaned;
- a gauze swab soaked in a 2% chlorhexidine solution is applied to the area of the bone defect for 5 minutes;
- Having removed the gauze swab, the defect is washed with a mixture of 1 g of tetracycline and 20 ml of sterile saline;
- a bioactive material (hydroxyapatite) is moistened in a tetracycline-based solution;
- the material is injected into the defect site and covered with a collagen membrane soaked in a tetracycline solution.
2 days before surgery, a course of systemic antibiotics is prescribed three times a day. Before surgery, rinse the mouth with a 0.2% chlorhexidine solution for 1 minute.
Prevention recommendations
Following simple rules of prevention helps to improve the patient’s well-being. By following simple recommendations, you can reduce painful symptoms caused by inflammation and increase the effectiveness of treatment.
Oral care rules
- You need to brush your teeth with a soft-bristled toothbrush, which is washed with a disinfectant ;
- brushing your teeth after meals and before bed helps stop the development of pathogenic microorganisms in the mouth;
- do not use removable dentures during therapy to prevent further aggravation of the disease;
- rinse with solutions with antiseptic properties;
- use lip balms to prevent lip chapping.
Successful fight against the disease depends on the amount of fluid you drink - drinking at least two liters a day will help you avoid dehydration and speed up the elimination of toxins.
What foods to eat
Nutrition during the treatment of mucositis involves eliminating damage to the affected mucosa, for which it is recommended:
- give up alcohol;
- exclude too hot, sour, spicy foods and drinks;
- You need to include protein-containing and low-calorie foods in your diet.
- Complete restoration of the dentition in just 4 days!
more detailsRoott Pterygoid Implants Sinus lift is no longer needed!
more details
Once and for life! Express implantation in 4 days with a permanent ReSmile prosthesis
more details
All-on-4, All-on-6, ReSmile, Zygomatic implantation We use all modern methods of dentition restoration
more details
Features of peri-implantitis
The course of the inflammatory process with peri-implantitis is more severe. The peculiarity of peri-implantitis is that the area of inflammation is not separated from the bone by a zone of connective tissue, as in periodontitis (as can be seen in the figure above), but is in contact with the bone. In periodontitis, the gum pocket has a layer that separates it from the bone, so the bone tissue is separated from microbes. With peri-implantitis there is no such layer. The degree of bone resorption (bone loss) can be assessed using a control x-ray taken after the installation of dentures.