A. Zorian , Candidate of Medical Sciences, Department of Hospital Therapeutic Dentistry, Moscow State Medical University
A. Hovsepyan , director of dental clinical training, dentist V. Chilikin , associate professor, candidate of medical sciences, Honored Doctor of the Russian Federation, Department of Hospital Therapeutic Dentistry of Moscow State Medical University
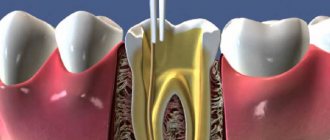
The success of endodontic treatment is largely determined by the quality of root canal filling. High-quality filling today means three-dimensional sealing of the entire branched root canal system, which plays the role of a reliable barrier between the tooth cavity and periodontal tissues.
Over the long history of endodontics, various techniques and materials have been used to fill the root canal.
Until recently, the main method of filling root canals in Russia was the method of filling with one paste. At the same time, pastes based on zinc oxide and eugenol, as well as preparations containing resorcinol and formaldehyde, were very popular. The technique of filling a root canal with paste is quite simple and does not require significant time and material costs. However, filling canals with one paste has a number of significant disadvantages: 1. With this technique, only the main canal is filled with the material, and numerous branches of the root canal system remain open. 2. Very often the paste is discharged beyond the root apex, since there is no adequate control over the filling of the root canal with material. 3. The paste fills the root canal unevenly, leaving voids and not providing adequate sealing. 4. All pastes shrink and dissolve upon contact with tissue fluid. 5. Most pastes have an irritating effect on the periodontium.
Considering all of the above, it is not surprising that the International Dental Association and the American Dental Association do not recommend the use of the root canal obturation technique with one paste.
Endodontic materials
An ideal root canal filling material must meet the following parameters: 1. Provide a reliable seal throughout the entire root canal system. 2. Be non-toxic and have good biocompatibility. 3. Do not irritate the periodontium. 4. Do not shrink in the canal. It is desirable that it expands slightly when introduced into the canal or during the curing process. 5. Have a bacteriostatic effect or at least not support the growth of bacteria. 6. Easy to sterilize before use. 7. Be radiopaque. 8. Do not change the color of the tooth. 9. If necessary, it can be easily removed from the canal. 10. Have a curing time sufficient for comfortable work. 11. Do not dissolve in tissue fluid. 12. Have good adhesion to dentin and filling material.
Such an ideal material does not exist today. However, these requirements are best met by the methods of filling root canals with gutta-percha and sealer. The vast majority of root canals around the world today are filled using gutta-percha.
Duration of filling
The need to replace the paste with which the canal cavity is filled is considered a controversial issue within the framework of scientific doctrine. Many dentists adhere to the position that a one-time filling is sufficient to obtain the desired effect, indicating that a repeat procedure should be carried out only in situations where the negative symptoms that bother the patient sharply increase.
Calcium hydroxide filling the root canal lasts no more than 1.5-2 weeks, which at first glance makes it difficult to follow the recommendations of the treatment protocol. However, in practice it turns out that pathogens lose their functions already on the second or third day from the moment the composition is applied. Clinical studies revealed that reducing the duration of action of the paste under a temporary filling to 48 hours reduces the likelihood of incomplete therapy by 10-15%. In addition, the addition of iodoform can reduce the frequency of complications in more than 20% of cases.
Filling root canals with gutta-percha
Gutta-percha is a hard, but at the same time elastic and flexible coagulation product of the latex of tropical gutta-percha plants. Gutta-percha is divided into two types - alpha and beta - which differ greatly in physical properties.
For the production of gutta-percha points, beta-gutta-percha is traditionally used, which has greater hardness and spatial stability and less stickiness. Beta gutta percha requires higher temperatures to soften. However, recently, more fluid and sticky alpha gutta-percha has become increasingly popular, providing, when used in a heated state, a more homogeneous filling of the entire branched root canal system.
Alpha gutta-percha is used for techniques that involve working with thermoplasticized (heated) gutta-percha: vertical condensation and thermoplastic injection techniques. In addition, there is a special type of gutta-percha used to produce Thermafil obturators. This patented type of gutta-percha is similar in chemical properties to beta-gutta-percha, but at the same time has the physical characteristics of alpha-gutta-percha.
The production of gutta-percha points is mainly concentrated in Southeast Asia. One of the largest suppliers of gutta-percha is Korea. However, recently gutta-percha points have begun to be produced in Brazil.
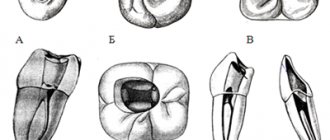
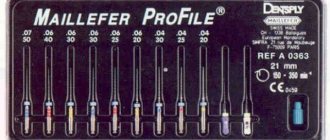
Pins are divided into standard pins, which have a 2% taper and ISO sizes from 10 to 140, and tapered pins, which have a 2% to 12% taper and sizes from 20 to 30.
Gutta-percha points are made either manually (“hand-rolled”) or by machine. It is believed that the manual method provides higher precision in making pins. Machine-made pins often do not guarantee accurate calibration. It should be especially noted that all pins made in Brazil are machine-made.
The commercial name “gutta-percha pins” has taken root well and is used everywhere, although the content of gutta-percha itself in these pins is about 20%. The main component of the pins (60-70%) is zinc oxide. The remaining 10% consists of barium sulfate, wax, dyes and other additives.
The main advantage of gutta-percha is the predictability of root canal obturation. Its advantages also include good biocompatibility and low toxicity, the ability to condense, ensuring dense and uniform filling of the root canal, softening when heated, which allows for three-dimensional obturation of the root canal system, spatial stability (in the hardened state it practically does not change its volume) and ease of its removal from the root canal if re-treatment is necessary.
Despite all the obvious advantages, gutta-percha also has a number of disadvantages associated with the peculiarities of its physical and chemical properties and the technology of application. The disadvantages of gutta-percha are as follows: 1. It cannot be used without a sealer, since it does not have adhesion to dentin. 2. Gutta-percha does not have a bactericidal or bacteriostatic effect. 3. Thin pins have very high flexibility and softness, which requires high qualifications and experience of the doctor, especially when filling narrow canals, and can also lead to deformation of the pins during their fitting. 4. Thermoplasticized gutta-percha shrinks when cooled. To compensate for this shrinkage, it is necessary to continue the condensation process until it cools.
Fillers - solid fillers
The most widespread are two types of fillers. Filling root canals with gutta-percha pins is more common than with metal ones.
Gutta-percha
Gutta-percha is a product of processing latex extracted from tropical plants. When heated, the structure of the substance softens to a fluid state, and when cooled, it hardens to a hard and elastic state. The composition of gutta-percha pins includes no more than 20% of gutta-percha itself, the rest of the composition is zinc oxide, heavy metal salts, dyes and other impurities of polymer compounds, waxes and antioxidants.
This material meets most requirements, in particular, its most positive properties are biocompatibility with human tissues and the absence of allergic reactions. Gutta-percha is easily inserted and removed from the canal, can be detected on x-rays and does not stain tooth enamel, but it also has a serious drawback. It does not create a hermetic protection against the penetration of pathogenic bacteria and does not have a bactericidal effect.
In an attempt to eliminate this drawback, dentists softened gutta-percha in chloroform and other solvents, but when the solvents evaporated, the material shrinked greatly. The same effect was achieved when heated.
As a result, it was found that gutta-percha pins are best combined with cements, which provides the filling with tightness and other positive properties of gutta-percha.
Silver pins
Metal pins entered dental practice much earlier than gutta-percha canal filling. Since silver is a very soft and pliable metal, it is easy to install even in a strongly curved root canal. Silver pins have an antibacterial effect, but they also have a significant drawback, which in recent years has increasingly reduced the use of silver in dental fillings to nothing. With prolonged contact with tissue fluid, the metal begins to oxidize, causing corrosion and the release of toxic silver salts, which can lead to the onset of an inflammatory process.
The pins themselves do not provide a seal during filling, and during repeated treatment, which is required very often, it can be problematic to remove them.
Titanium pins
Unlike silver, titanium is not subject to corrosion, is highly durable, hypoallergenic and does not irritate soft tissues. For years, dentists have been offering their patients root canal fillings with titanium pins to strengthen damaged teeth. This method is still used today because of its cheapness and the widespread myth about the miraculous nature of titanium pins.
However, everything is not so rosy and a pin can only be installed in a slightly damaged tooth with a removed nerve. The fact is that for the installation of a pin, a bed must be formed in the root of the tooth, which greatly thins the walls of the tooth. The titanium pin itself has very low elasticity and high rigidity, which automatically distributes the load on the thinned walls, ultimately provoking a root fracture. If, however, the tooth canal is filled with the installation of such a pin, the tooth itself needs a crown.
Sealers for root canal obturation
It should be noted that the need to use a sealer is a relative disadvantage, since there is currently no material that can provide predictable filling of the main channel, and at the same time be fluid enough to fill all its branches.
The sealer acts not only as a sealant that fills all branches of the root canal system and ensures adhesion of gutta-percha to the canal walls, but also as a lubricant that ensures free sliding of gutta-percha pins in the root canal.
The sealer must meet the following requirements: 1. After mixing, it must have a sticky consistency in order to ensure good adhesion to the canal walls after curing. 2. Seal the canal hermetically. 3. Be radiopaque. 4. Do not shrink during the curing process. 5. Do not stain tooth tissue. 6. Have a bacteriostatic effect or at least not support the growth of microorganisms. 7. Harden slowly. 8. Do not dissolve in tissue fluids. 9. Do not irritate periapical tissues. 10. Dissolve in standard solvents if it is necessary to unseal the canal. 11. Do not cause immune reactions in periapical tissues. 12. Do not have a mutagenic or carcinogenic effect.
None of the sealers presented on the modern market can meet all the requirements placed on it. Basically, either natural root cements or polymeric materials are used as sealers today. Natural sealers – Endomethasone (Septodont), Cortisomol (Pierre Rolland), Tubli-seal (Kerr), etc. – which are based on zinc oxide, dissolve in tissue fluid, which can lead to disruption of the tightness of the root canal system. In addition, they have low adhesion to dentin and can cause staining of tooth tissue. At the same time, polymer sealers - AH Plus (Dentsply), Adseal (META Biomed), etc. - are less soluble in tissue fluid, do not stain tooth tissue and have better adhesion to root dentin.
Until now, the question to what level to fill the root canal remains open. There is intense debate as to whether gutta-percha should not reach the anatomical apex by 0.5 mm or stop directly at it. Today, the only indisputable fact is that the less we expand the apical narrowing, the better the quality of obturation, the more reliable the isolation of periodontal tissues. In addition, it must be remembered that the theory of active apical therapy has shown its inconsistency. In modern endodontics, removal of sealer beyond the root apex is not encouraged, even in the presence of inflammatory processes in the periodontium, although studies have shown that when a small amount of sealer is removed into the periapical tissue, no serious complications are observed after treatment.
***
There are various methods for filling root canals with gutta-percha: the single (central) pin method, lateral condensation, thermomechanical condensation, filling the root canal with chemically softened cold gutta-percha, intracanal hot vertical condensation, thermoplastic injection technique and the use of thermophiles.
Depophoresis
Depophoresis is a therapeutic technique that allows you to completely disinfect the canal and make it sealed using a specialized device.
The procedure includes:
- anesthesia;
- exposure of the mouth of the root canal;
- introduction of an electrode with a negative charge into the root canal;
- applying a second electrode to the outer surface of the cheek, delivering a 2mA discharge and passing copper-calcium hydroxide through the root passage;
- treating the canal with a 10% suspension of calcium hydroxide or distilled water.
The average duration of the depophoresis procedure is 7-8 minutes. In this case, for a complete cure, the patient may need at least 3 sessions. In the pauses between these sessions, the root canal is filled with copper-calcium hydroxide paste. At the end of the procedure, the root passages are sealed with specialized dental cement.
Carrying out depophoresis can hardly be called affordable. However, the high cost of the procedure can be considered adequate if we take into account its high efficiency.
Filling root canals with cold gutta-percha
Single pin method
This method consists in the fact that after appropriate treatment of the canal, which means giving it a taper of 4, 6 or 8%, a sealer is applied to its walls using a paper point. After this, a pre-selected pin with an appropriate taper and tip size is inserted into the canal. The pin should fit snugly against the canal walls. Some authors recommend shortening the tip of the pin by 0.5 mm. Using a heated tool, the pin is cut at the level of the mouth and its condensation is carried out in the vertical direction.
This technique can be a good alternative for doctors who prefer to fill canals with monopaste, but this only ensures filling the lumen of the main canal, and not three-dimensional obturation of the entire root canal system.
You just have to want it
For specialists in this case, the field of activity remains endodontic treatment in particularly complex root canal anatomy, as well as in particularly complex clinical situations, and for “particularly gifted” specialists - perhaps complex cases of root canal revision.
There is enough work for everyone. In any case, this would benefit “general-profile” therapeutic dentistry.
The article was provided by the magazine of the official publication of the Association of Dentists of Lower Saxony (Germany) NZB - Niedersächsisches Zahnärzteblatt (No. 6, 2011, pp. 31-34).
Translation by Inna Bichegkueva.
Method of lateral condensation of cold gutta-percha
This scheme involves filling with gutta-percha pins with lateral pressing of each of the pins against the canal walls. For a long time, this technique was the “gold standard” with which all other canal obturation techniques were compared.
After drying the root canal using paper points, its walls are coated with sealer. Then a master pin selected to size is inserted into the canal, the tip of which is moistened in the same sealant. A spreader is then used to condense the master pin against the canal walls, providing sufficient space for the insertion of additional pins. The density of canal obturation depends on the depth of penetration and the shape of the spreader. According to Chohayeb (1993), ISO-standardized hand spreaders should be inserted into the root canal up to 1 mm from the tip of the gutta-percha point, which improves the homogeneity and density of the filling. After the master pin condenses, additional pins are condensed to it and the channel walls, the tips of which are also wetted in the sealant. Each subsequent pin enters the canal to a shallower depth. Lateral compaction of the pins is carried out until the canal is homogeneously filled, the criterion for which is the impossibility of inserting the spreader into the canal. The recommended time for pressing the pins against the canal walls with a spreader, according to various authors, is 15–30 seconds. After this, the protruding ends of the gutta-percha pins are cut off using a heated instrument, and the mouth of the canal is closed by vertical condensation of gutta-percha.
The quality of root canal obturation during lateral condensation of cold gutta-percha is influenced by many factors. First of all, this is the shape of the processed channel. The root canal must have a uniform taper along its entire length and an apical ledge that prevents material from being removed beyond the apex during condensation. The ratio of gutta-percha to sealer is also of great importance. The following ratio is recommended: 95% gutta-percha, 5% sealer.
Long-term use of the lateral condensation technique of gutta-percha has shown its high clinical effectiveness, ease of use and reliability. Many researchers point to the high filling density of the root canal when performing lateral condensation. However, other authors demonstrate that when performing lateral condensation, there is a risk of longitudinal root fracture due to the forces applied, especially when the root is weakened (for example, when the canals in thin roots are over-expanded). In addition, with this technique it is not possible to achieve homogeneity of the material and filling the lateral and apical branches of the canal with gutta-percha, which can lead to the development of complications from periodontal tissues - the development (or maintenance) of an inflammatory reaction, destruction of bone tissue.
It should be added that when working with cold gutta-percha, in order to adequately seal the mouth of the root canal, it is advisable to use a heated instrument to cut off the pins 2-3 mm deeper than the mouth of the canal and fill the remaining part with heated gutta-percha by injecting it.
In order to improve technologies for filling root canals with cold gutta-percha, various techniques have been proposed, which are currently of interest mainly only from the point of view of the history of the development of endodontics. Such techniques include thermomechanical condensation and filling with chemically softened cold gutta-percha.
Other obturation methods
A unique method of filling root canals is the so-called Russian Red, which was previously used in the countries of the Eastern Bloc, including in the former GDR. This filling material is a resin-based polymer in nature. Once cured in the channel, the material turns red and becomes incredibly hard. It is very difficult to remove from the root canal during root canal revision (only with the help of aggressive solvents). However, after filling the root canals with this material, a revision has to be carried out quite rarely, since teeth with these old root fillings are most often miraculously completely “cured” without causing complaints. The author cannot give an explanation for this phenomenon.
After Russian Red root canal filling, teeth are miraculously completely “cured.” With other exotic methods of filling root canals, completely different paste-like sealers without gutta-percha are used. Although these methods save time, such root fillings are less airtight. Therefore, such methods are generally not recommended, even within the framework of “generally available endodontic treatment.” There is still no evidence-based medicine for these methods.
At the beginning of the article, two very labor-intensive methods of root canal filling were already mentioned, which differ significantly from each other: lateral condensation (compaction) of gutta-percha using several pins and vertical condensation of heated gutta-percha. These treatment methods, as well as their various modifications/mixed variants, belong to private dental services in the field of endodontics and are outside the scope of public health insurance. Their use requires a lot of time and the purchase of expensive devices, so they can be classified as expensive private dental services, most often provided in dental offices specializing in endodontics, as well as in university clinics.
Thermo-mechanical condensation (or filling root canals with a rotating condenser)
This method is currently practically not used. With this technique, a tool that has in its design elements of an H-file (but with a reverse thread) and a channel filler is used to soften the gutta-percha and move it in the apical direction. This instrument is called a condenser or gutta condenser. To soften the gutta-percha and condense it, the instrument must be rotated clockwise at a speed of at least 8000 rpm.
A standard gutta-percha pin should be 1–2 sizes larger than the last instrument used to process the canal, that is, 1–2 mm shorter than the working length. Control of the level of gutta-percha filling is ensured by inserting the instrument, 1.5 mm short of the apical constriction.
The disadvantages of the method are the unpredictability of the level of filling, the high risk of breaking off the instrument in the canal, and the likelihood of voids forming in the gutta-percha due to its gluing to the instrument. In addition, this technique also does not provide reliable obturation of the lateral branches of the canal.
General overview
The composition used affects the periapical structure. The reaction of irritated tissues to the formation of a necrotic layer is the formation of a connective structure, which subsequently undergoes mineralization. The alkaline pH level is sufficient to neutralize the lactic acid of osteoclasts, so the mineral structure of dentin and bone tissue remains protected.
Calcium hydroxide, used as part of endodontic therapy, helps solve a number of functional problems, such as:
- Reducing the number of pathogenic bacteria located in the canal cavity;
- Maximum possible extraction of necrotic tissue;
- Reducing the volume of concentration of bactericidal endotoxins.
Using only mechanical instruments to treat the cavity, despite the use of an irrigator, does not provide a sufficient disinfectant effect, since not only pathogens, but also dead tissue particles remain in the canal. Calcium hydroxide, provided by the temporary filling protocol, has a positive effect on the general condition of the affected root, and creates conditions for full treatment.
Filling root canals with chemically softened cold gutta-percha
Filling techniques using chemically softened cold gutta-percha are also called “immersion methods.” Historically, these methods appeared almost simultaneously with the beginning of the use of gutta-percha. For obturation of gutta-percha softened with solvents (chloroform, some oils), no sealer was used. This led to micro-seepage due to shrinkage of the gutta-percha after the solvent evaporated and the root filling hardened. Therefore, the incidence of complications when using such techniques was very high. Despite the fact that later various sealers began to be used with “immersion” methods, these techniques are currently practically not used due to the inability to control the shrinkage and deformation of gutta-percha and the quality of canal obturation.
How to check the quality of canal filling?
Quality control of fillings is an integral part of the treatment process and is performed at every stage. X-ray control is especially important after filling. It allows you to identify areas of insufficiently dense obturation, detect pins or sealer residues protruding beyond the root apex, identify fragments of files and other defects. All this can lead to severe pain after treatment, as well as to the development of complications.
The x-ray image should clearly show the canal cavities, densely filled with filling material. There should be no enlightenment. The filling material should reach the very top of the canal.
Following simple rules of prevention also helps to avoid complications. Pain after treatment can last from several days to a month and does not always indicate ineffectiveness or low quality of treatment. However, if they appear, you should consult your dentist. Also, after treatment, it is recommended to abstain for some time from physical activity, drinking alcohol, and eating hot and spicy foods.
To prevent pulpitis, carefully monitor your oral hygiene. Use only professional products. If during the day you do not have the opportunity to brush your teeth after eating, use Asepta Fresh mouthwash. It disinfects the oral cavity, effectively fights caries, and normalizes acidity.
Choosing temporary filling material: proceed without mistakes
Every practicing dentist knows how important the correct selection of filling material is for effective treatment. Modern dentistry offers a huge selection of materials, which are divided into classifications depending on composition, properties, time of use, purpose, etc. A fairly large place among them is occupied by a group of filling materials for temporary fillings, as well as insulating and therapeutic pads.
Materials for temporary fillings
Based on the time of action, they are divided into bandages and temporary fillings. Inexpensive materials are used for dressings. The most common option: water-based dentin or dentin-paste. The period of use of these materials should not exceed 14 days. At the same time, the bandages do not differ in aesthetics and durability. All temporary fillings are cements : zinc phosphate, zinc eugenol, polycarboxylate, glass ionomer, etc. The period of their use in the patient’s oral cavity ranges from several weeks to six months.
1) Zinc sulfate cements (“artificial dentin”)
The main components of the composition are zinc sulfate and zinc oxide. Adding water helps the mass harden. The most famous materials of this group: “Dentin for dressings”, Dentine paste, Vinoxol, etc.
2) Zinc-eugenol cements
The basis of the composition is zinc oxide and eugenol. According to Smith's classification (1996), this subgroup includes three main types of cements: simple zinc oxide eugenol; reinforced zinc oxide eugenol with filler and cements based on orthoethoxybenzoic acid (EBA). The materials consist of zinc oxide powder, into which 1-2% zinc acetate, acetic anhydride or rosin are added, which accelerate hardening. Purified eugenol or clove oil is used as a solvent. Additionally, to speed up the hardening process of cement, acetic acid or 1% ethyl alcohol, as well as a small amount of water, can sometimes be added. The most popular representative of this group is Cariosan. Zinc-eugenol cements are used not only for temporary fillings , but also for therapeutic linings. It is important to take into account that eugenol disrupts the polymerization process of composites, so experts do not recommend using this type of cement in combination with them. That is why today zinc-eugenol cements are practically not used for therapeutic linings in commercial clinics, but they are still in demand in pediatric dentistry and in municipal clinics for the treatment of deep caries in two visits.
3) Zinc phosphate cements
75-90% of the cement base is zinc oxide with the addition of other modifying oxides. The liquid part is an aqueous solution of 38-44% orthophosphoric acid containing phosphates of zinc, aluminum, magnesium, etc. Among the most famous zinc-phosphate cements presented on the Russian market are: Phosphate cement from Raduga-R, Uniface ( “Medpolymer”), Adgesor (“Dental Spofa”), DeTreyZinc from “DeTrey/Dentsply”, etc. As a rule, metals containing silver are added to these compositions to impart a bactericidal effect. As an example, we can o), Phosphate with silver and bactericidal Foscin (“Rainbow-R”), as well as cements containing bismuth oxides: Visphate cement and Dioxyphosphate (Medpolymer).
The undoubted positive properties of these cements are: ease of use, low thermal conductivity, good X-ray contrast, and impermeability to acids and monomers. However, they have quite a lot of negative characteristics. Among them: weak adhesion, low resistance to the aggressive effects of saliva, shrinkage, low mechanical strength, the presence of free acid and lack of aesthetics.
Most often, zinc-phosphate cements are used as an insulating spacer for filling baby teeth and permanent crowns, fixing cast stump inlays, pins, crowns and bridges.
4) Polycarboxylate cements
The basis of cement is thermochemically treated zinc oxide with the addition of magnesium oxide, which reduces the reactivity of the first component. Aluminum is also often added to powders. The solvent is represented by a 32-42% aqueous solution of polyacrylic acid. During the hardening process, cement turns into an amorphous zinc-polyacrylate gel, which contains zinc oxide particles.
The positive properties of these cements include: satisfactory chemical adhesion to enamel and dentin, strong bond with metals, weak toxicity to the pulp compared to phosphate cement and high biocompatibility with tooth tissues. Negative properties: high solubility under the influence of saliva, short formation time in the oral cavity and insufficient fluoride adhesion.
Polycarboxylate cements are used as insulating spacers when filling teeth under artificial crowns, for fixing orthopedic and orthodontic structures, and in the treatment of baby teeth (1-2 years before their replacement).
All materials for temporary fillings must be:
- harmless to the pulp;
- have high plasticity;
- inactive for other drugs;
- insoluble under the influence of saliva;
- sealed for at least two weeks;
- have a certain strength;
- easily removed from the dental cavity using an excavator, probe or drilling.
Insulating and healing pads
The purpose of these materials follows from their name. Despite the fact that they can be conditionally classified as filling materials, the application of gaskets is an integral step in the treatment of medium and deep caries. spacers when treating medium and deep caries . They contain calcium hydroxide, which has an anti-inflammatory effect on the pulp and stimulates the deposition of replacement dentin. Among the most popular materials are: “Calmecin”, “Dycal”, “Calcimol” and “Alcaliner”, as well as modern insulating gaskets made from glass ionomer cements, such as: “Fuji 2”, “Chelon Fil”, “Base Line” and etc.
Today the following requirements apply to insulating gaskets:
- reliably protect dentin from chemical and temperature irritants;
- easy to install;
- withstand the effects of saliva when the filling is damaged;
- withstand chewing load;
- have good adhesion to tooth tissues;
- do not have an aggressive effect on the dental pulp;
- do not affect the color of tooth enamel.
Therapeutic pads have an anti-inflammatory, regenerating and analgesic effect, therefore they are used in the treatment of deep caries. They are characterized by good ductility, the material hardens quickly. Basically, the therapeutic component of modern medical pads is calcium hydroxide, which has a bactericidal effect and shifts the pH environment in the tooth cavity to the alkaline side, which ensures neutralization of acids. The base material can be polymer, water-based, oil-based or monomeric. Dentists use either ready-made medicinal pads or prepare them themselves. The use of a therapeutic pad significantly reduces the risk of the formation of microcracks and the development of secondary caries. However, with all their advantages and positive effects on the pulp, these compositions have noticeable disadvantages:
- low adhesion to dentin, which determines the weak adhesion of the filling to the tooth tissues;
- lack of resistance to the aggressive effects of saliva, which creates conditions for further infection;
- accidental contact of gasket particles with the walls of the formed cavity can lead to secondary caries.
It is recommended to apply therapeutic pads in cases where the bottom of the formed cavity is located too close to the pulp. It is believed that in order to prevent infection of the pulp by toxins, the minimum thickness of the dentin layer should be 2 mm. When placed correctly, the therapeutic material completely covers the bottom of the carious cavity or lies pointwise in the areas where the pulp horns adjoin. In this case, it is necessary to carefully remove it from the walls of the cavity in order to avoid disruption of the adhesion of the filling material and the development of secondary caries.
Regardless of their purpose, all temporary filling materials must meet the same clinical requirements:
- do not have a toxic effect on the enamel, dentin and pulp of the tooth, as well as mucous membranes;
- be harmless to the body as a whole;
- have antiseptic, anti-inflammatory and anti-caries effects;
- be chemically inert and resistant to aggressive environments such as alkalis and acids;
- have sufficient adhesion to dental tissues, mechanical strength and wear resistance;
- do not change the color of the tooth and do not lose its original color over time;
- do not cause the appearance of galvanic currents in the oral cavity;
- do not change shape and volume during hardening;
- have good radiopacity.
For an experienced specialist, purchasing filling material, like any other dental consumable, usually does not cause any particular difficulties. However, the dental market, being one of the most dynamic and rapidly developing areas of global business, is constantly changing, which makes it difficult to keep track of new products and truly profitable offers in a timely manner. Today, the marketplace of the Internet portal “Dentists Club” is rightfully considered one of the most reliable and positively proven resources. This aggregator has been successfully operating in the dental market since 2017 and has already proven itself as a proven and honest partner. At the same time, the Dentist Club market is the only aggregator of offers in the field of dentistry today, which allows you not only to purchase the necessary goods at the guaranteed best prices, but also in addition to receive a cashback of 1.5% back to your account!
What other benefits does the Dentist Club market provide?
1. Time saving
- You don’t need to go to all the search results sites to find what you need
- There is no need to call companies and try to explain to them over the phone what you need
- No need to send a request and wait for managers of trading companies to answer or call you back
2. The Dentist Club Market service helps when communicating with doctors
- You can easily find the desired product by description and photo
- Determine the desired model and its modification
- Check all these parameters directly with your doctor and get his approval
- Place an order in one click.
3. Lowest prices on the market guaranteed
- You can simultaneously see the prices of all companies offering the required product
- Compare the prices presented and choose the most profitable one
- The manager of the selected company will call you back. He doesn’t need to explain ten times what you need, because... He sees all the necessary information in the generated order.
- And don't forget about cashback!
4. 100% order security
- Absolutely all companies - suppliers of dental equipment and consumables, collaborating with the marketplace, have already been checked for legal purity by lawyers of the Dentists Club. That is why all purchases made on the Dentists Club market are absolutely reliable!
5. Ease of use
- You can install the Dentist Club Market service on your phone so that it is always at hand. Open the app, find the products you need, and order. Everything is quick, accessible and simple. Application in the App Store on iPhone (iOS) or on Google Play for Android.
Aida Levasheva – senior nurse at the dental clinic (Samara):
“To be honest, purchasing dental supplies was my least favorite job until recently. I do not have a dental education, and until recently this created certain difficulties. Of course, before purchasing, I asked doctors what material was more convenient for them to work with. The problem was that everyone had their own preferences. I had to search for what I needed all over the Internet, compare prices, and call managers of trading companies for half a day to find out the terms of payment and delivery. This often took almost the entire working day. And in the end, the head physician, looking at the list and prices, crossed out half of the points. The Dentist Club Market was recommended to me by one of my classmates at medical school. I really liked the resource. For me, the most important thing is a very convenient and simple interface, which you can easily understand even without a dental education. I especially liked the function where you can compare prices for the desired product! If you need professional advice, you can get it directly on the website and immediately pay for your order there. All this is very convenient and saves a lot of time!”
Go to Market >>>