A variety of modern techniques used for filling developed root canals differ significantly from each other, but are still foreseeable. For obturation of root canals, dentists are provided with a very large selection of materials, but there is no such confusion as when choosing a combination of solutions for root canal irrigation. At this stage of endodontic treatment, there are also no dangerous mutual effects between the materials used.
Gutta-percha
In fact, the most necessary material for filling root canals is undoubtedly gutta-percha, which is used in almost any filling method. This material has the elasticity of rubber and is by its nature a close relative. Gutta-percha is obtained by evaporating the milky juice of special varieties of gutta-percha tree. Gutta-percha was first used for filling root canals in 1867 by Bowman.
ISO-standardized tapered pins contain the following components:
- gutta-percha;
- zinc oxide - as a filler;
- barium sulfate - for radiopacity;
- waxes - to obtain the required consistency;
- dyes and small amounts of trace elements (Guldener, 1993; Hülsmann, 1993).
Gutta-percha points are most often used in combination with so-called sealers.
Sealers are pastes for filling root canals, which are mixed from two components and serve to fill the gap between the canal wall and the gutta-percha pin/pins. Sealers also fill small branches of the root canal and lateral tubules.
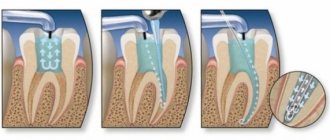
There are two options for applying paste to fill the canal:
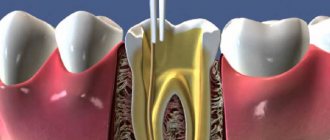
- first, using a canal filler (lentulo), the sealer is introduced into the canal, and then a gutta-percha pin is inserted, and the sealer is pushed towards the canal walls;
- The gutta-percha point is coated with a small amount of sealer and then inserted into the canal, thereby pushing the sealer into the canal.
This is the “standard concept” of root canal filling, which has been used by dentists in everyday practice for many decades. Sealers are pastes for filling root canals, which are mixed from two components and serve to fill the gap between the canal wall and the gutta-percha pin.
In his dental clinic, the author also uses this effective and efficient method of filling root canals as part of the services covered by public health insurance: the sealer is inserted into the root canal on one (central) gutta-percha pin. The author has been using AH Plus material as a sealer for 7 years. This method of filling root canals is called the method of one (central) pin, or monopin. Currently, this method is most often used for endodontic treatment as part of services covered by public health insurance.
This method has some significant advantages: a ready-made conical gutta-percha pin, due to pressure, moves the sealer paste, previously introduced into the root canal (or introduced simultaneously with the pin), to the canal walls and distributes it over their entire surface. Most often, due to the pressure of the gutta-percha pin, the sealer paste also penetrates into the areas of the apical branches of the root canal. In many cases, at the root apex there is a branching of the main root canal, resembling a river delta.
However, in principle, as a result of mechanical treatment of the root canal, according to all the rules, only the main axial central root canal is developed. Most often, at the moment when a gutta-percha pin is inserted into the root canal, additional (lateral) tubules that are completely inaccessible for mechanical treatment are also filled with filling material, since the excess applied sealer under pressure inevitably penetrates laterally and apically (!), i.e. into in all possible directions.
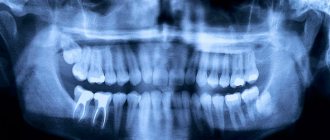
However, this often leads to unwanted removal of the sealer paste beyond the physiological or even anatomical apical foramen. The question of the negative impact of this phenomenon remains controversial. For example, in Germany, the removal of filling material beyond the apical foramen is an indicator of insufficiently high-quality treatment, and American colleagues believe that it is the (insignificant) removal of filling material beyond the apical foramen that serves as a sign of a particularly successful root canal filling (puff).
As with many aspects of practical endodontics, unfortunately, there is no evidence-based medicine yet on the issue of the acceptable level of root canal filling. All conclusions are made purely empirically. A good confirmation of this is the way dentists treat the removal of filling material beyond the apical foramen.
Of course, whether negative consequences will be observed when the material is removed beyond the apical foramen depends on what material was used to fill the root canals and to what extent it was removed beyond the apex. Thus, slight removal of a biologically inert sealer beyond the apical foramen when used correctly is most likely safe. In Germany, removal of filling material beyond the apical foramen is an indicator of insufficiently high-quality treatment. But the removal in a larger volume beyond the apex of a non-resorbable filling material with supposed cytotoxic properties (for example, the previously frequently used material Diaket, Seefeld) most likely poses a danger. In this case, if there is a significant amount of material removed beyond the apex, it is subsequently necessary to perform an operation of resection of the root apex. It all depends on the situation in a particular clinical case, i.e., it should be taken into account whether the material removed beyond the apex has an irritating effect on the periapical tissues.
There are completely new methods of filling root canals, which use ONLY heated gutta-percha (without sealer). When using these methods, gutta-percha softens to such an extent that, without the additional use of a sealer, it can penetrate into all the necessary areas of the root canal. The result is a hermetic root filling with good adaptation to the walls of the root canal.
Such methods (for example, the Thermafil system) are very rational, and therefore can be used as part of “generally available endodontic treatment”. However, the questions about whether it is necessary to abandon the additional use of sealer and whether a sufficiently sealed root filling is obtained without a sealer have not yet been finally clarified. There is also no evidence-based medicine on this important issue.
When briefly listing the current methods of filling root canals using gutta-percha, it is necessary to mention the methods of lateral condensation and vertical condensation (according to Schilder). These labor-intensive methods are used, as a rule, as private medical services and mainly by dentists specializing in the field of endodontics.
The author believes that due to the large investment of time and money, these methods are difficult to use as “standard” within the framework of “generally available endodontic treatment.” However, as a compromise solution, “mixed” methods can be used.
A Look at Some Popular Root Canal Obturation Materials
Malanin Igor Valentinovich Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Economics, President of the European Academy of Dentistry, Head of the Kuban Scientific School of Dentistry
Endodontics today continues to strive for high technology and new materials. As more and more researchers have proposed solutions to common clinical situations, the complexity of the arsenal of materials for root canal obturation has increased. The high level of manual skills required in endodontics inevitably determines the improvement of personal skills. Hence, it is quite obvious that numerous publications related to a specific material or method have appeared.
Most of the currently used root canal obturation materials have been used successfully for several decades. The focus has typically been on clinical data and research aimed at improving or modifying established clinical practices. This often resulted in improvements to known techniques rather than the development of new materials.
In addition to personal, subjective influences, the literature on materials for root canal obturation reflects the prevailing concepts in endodontic practice that are popular at a given time. This occurs despite the almost universal belief that the core of clinical endodontic practice is the cleaning, shaping and filling of the root canal system. For example, when experts were absolutely sure that pulpless teeth were “foci of infection,” they placed their main emphasis on instrumental techniques aimed at “disinfecting” the root canal and on filling materials with a strong and long-lasting antiseptic effect. Later, endodontic techniques were gradually reoriented to reduce traumatic instrumentation damage to the periodontal ligament and to use materials that were better tolerated by the pulp and periapical tissues. Until recently, materials for root canal obturation were not studied as such outside of clinical techniques.
What principles guides a modern endodontist when choosing a material for obturation of root canals? Does the doctor delve into the composition of the material he uses, or does he fill “like everyone else”? As a rule, “experienced” doctors have been using the same material for decades.
Modern, newly created material for obturation of root canals has a short life. Many of the technologies and treatments that students learn today will be modified or replaced by others by the time these students become doctors. In order to keep up with the times, the dentist must have the ability to evaluate the potential of each new material and treatment method.
It is well known that the last stage of endodontic treatment is the complete, dense and hermetically sealed filling of the root canal system and all hard-to-reach areas with non-irritating materials. For successful treatment, three-dimensional filling of the entire space of the canal, the apical hole in the area of the dentinal-cement junction and additional canals is necessary with an inert, biologically compatible material that has spatial stability. Amputation methods for the treatment of pulpitis, used until recently in domestic dentistry, are considered a gross mistake in modern dental practice.
Root canal materials come into contact with biological tissue that is not protected by an epithelial layer, so their biocompatibility is of particular importance. It is generally accepted that a biologically acceptable material must be inert. In practice this cannot always be achieved. Therefore, material creators strive to achieve a favorable interaction between the material and the biological environment in which it is located, and which would not have a negative impact on the material itself. It is important that the material does not cause an inflammatory reaction in the tissue, as this can cause irritation, pain and necrotic changes.
A constant problem in endodontic treatment is the possibility of recurrent infection at the apex of the tooth due to the presence of microorganisms there. This dictates another requirement for materials for filling root canals - to have an antimicrobial effect.
In modern dentistry, it is quite difficult to combine these two material requirements, since this implies the need to take into account a high degree of selectivity of the biological response. After all, it is well known that a material with an antimicrobial effect causes an inflammatory reaction in adjacent tissues, and those materials that do not cause it have the best bacteriostatic properties. If we agree that complete sealing of the root canal cannot be achieved, the materials used must have sufficient antimicrobial activity to prevent the infiltration of microbes into the canal space and their proliferation. At the same time, the antimicrobial properties of the material should not be achieved at the expense of its biocompatibility.
Gutta-percha is a biocompatible material with very low cytotoxicity, so only the cements used with it will determine the tissue reaction.
Gutta-percha points are used in combination with cement, which is necessary to fill the spaces between the point and the root canal wall, thus preventing the penetration of microorganisms. It also lubricates the pins as they compact, filling channel irregularities and side channels.
The use of cements to seal the root canal without obturating pins is not recommended. When cements are introduced into the canal in large quantities, they undergo more intense dissolution and exhibit excessive shrinkage during curing. In addition, it is quite difficult to determine adequate filling of the canal, and there is a danger of cement leaking beyond the root apex into the surrounding tissue.
Until recently, it was generally accepted that filling a canal with cement could not guarantee against permeability of tooth tissue, and therefore the main attention was paid to imparting antimicrobial properties to these materials.
In clinical practice, a large number of materials are used to fill root canals, including:
- Zinc oxide eugenol cements (eg Tubliseal, Kerr);
- Polymer cements (AH Plus, Dentsplay; Diaket, ESPE);
- Cements containing calcium hydroxide (Apexit, Ivoclar; Sealapex, Kerr);
- Glass ionomer cements (Ketak Endo, ESPE; Endion, Voko);
- Polydimethylsiloxanes (RCA RoekoSeal, Roeko).
In this article, the author did not intend to describe all known materials for permanent root canal filling. But I would like to focus on some of them, due to their prevalence in Russia and specifically in the Krasnodar Territory.
Endomethasone - unfortunately, this material is by far the most purchased and popular endodontic material in Russia.
Endomethasone is a material based on zinc oxide eugenol paste; contains corticosteroids (hydrocortisone and dexamethasone), antiseptics, diiodothymol and paraformaldehyde, as well as radiopaque filler.
Antiseptics provide sterilization of organic residues in microchannels, deltoid branches, and affect the microflora of the periapical lesion during periodontitis. As the paste hardens, the effect of these substances weakens and then stops. If endomethasone is excreted beyond the apex, then eugenol diffuses quite quickly into the bloodstream, and then the remaining components of the paste gradually dissolve (first behind the apical foramen, and then in the canal).
As for corticosteroids, in addition to their positive effects, they also have a number of negative properties. For example, they weaken the protective mechanisms of the periapical area, in particular due to the suppression of phagocytosis, resulting in the proliferation of microorganisms; Their side effects cannot be ruled out either.
Included in the composition of endomethasone to reduce complications after filling, there are also products containing formaldehyde. The resorcinol formaldehyde method, proposed at the beginning of the last century and very widely used for a long time, was subjected to careful analysis in the 80s and early 90s for its toxic effect, of which quite a lot of examples have accumulated.
Electron microscopic research has demonstrated that formaldehyde denatures pulp proteins and, deposited in crystalline form on the surface of the denatured alcohol, binds tightly to it. If the proteinaceous material in the root canals is sufficient to bind formaldehyde, its systemic effects are negligible. If the pulp is partially or completely removed, the antiseptic can enter the periodontium, causing local and general adverse effects.
Many negative effects are associated with the use of paraformaldehyde and corticosteroids. When formaldehyde comes into contact with living tissues, it spreads throughout the body. Systemic studies found labeled paraformaldehyde in the blood, regional lymph nodes, kidneys and liver after pulpectomy in dogs using labeled 14-degree formocresol. In addition, it is well known that formaldehyde has mutagenic and carcinogenic properties. In this regard, the question arises about the possibility of contact with living tissues.
The popularity of this material among some doctors is explained by the fact that the addition of corticosteroid drugs and paraformaldehyde to endomethasone can significantly reduce the risk of developing painful reactions from the periodontium after endodontic treatment, even with accidental (permanent) removal of the material beyond the apex.
If the material is not brought to the apex or the canal is processed poorly, endomethasone is good for so-called chemical pulpotomy. In the first case, the antiseptic effect is leading, in the second, it is also possible to cause aseptic necrosis and mummification of the pulp without complete mechanical extraction. In other words, this drug is the drug of choice for doctors who have insufficient manual skills.
Without listing the negative properties of endomethasone and similar drugs, I would like to add that not only the International Dental Association and the American Dental Association, but also many Russian educational centers do not recommend (prohibit) filling root canals with pastes, since the latter do not provide reliable obturation.
It is also inappropriate to use cements containing calcium hydroxide (Apexit, Ivoclar; Sealapex, Kerr) for permanent filling. This is due to the fact that calcium hydroxide released from the material reduces its spatial volume, which is unacceptable for permanent filling. Doctors also forget that calcium hydroxide acts for a short time and is used for temporary filling.
AN-26, AN Plus
According to the author, a good alternative to the above materials is AN-26, which is widely used not only in the Krasnodar region, but also in world endodontic practice. It was first reported around 1957. It is an epoxy resin with poor solubility. It consists of silver powder (10%), bismuth trioxide (60%), titanium dioxide (5%) and hexamethylene tetramine (25%), which are mixed to the consistency of a thick paste with a liquid - bisphenol diglycidyl ether (100%). It has good adhesive properties, antibacterial activity, low toxicity and is well tolerated by periapical tissues.
AN 26 is a thin-flowing, slowly curing material. If it cures in contact with tissue fluid, it releases small amounts of formaldehyde. Hardening time is approximately 34 hours. With some filling techniques, this is considered an advantage, since it provides time for filling correction after X-ray control. Subsequently, a modification of this filling material was presented - AN Plus, which is a two-paste system that excludes the content of hexamethyl-tetramine, which is responsible for the release of formaldehyde.
AN-26 contains silver powder, therefore, in order to avoid discoloration of the tooth, all remnants of root cement must be removed to the level of the gum edge. In this regard, AN-26 and AN Plus produced by modern industry do not contain silver.
The mild cytotoxic reaction to freshly prepared AN26 may be due to the release of formaldehyde, which is formed as a by-product of the polymerization process. Because AH26 takes some time to polymerize, patients may experience some degree of sensitivity that may be associated with its use. AH Plus has been shown to release only a small amount of formaldehyde (3.9 mg/kg) compared to AH26 (1347 mg/kg). However, AH26 has cytotoxicity, although this is significantly reduced after curing of the material.
Endion
In their daily work, many doctors prefer the use of glass ionomer cements for permanent filling of root canals due to their biocompatibility with tooth and periodontal tissues. Clinical studies of the material, Endion (Voko), conducted by the author, showed good long-term results (over 7 years), which were compared with data from studies of other filling materials. Studies have shown high biocompatibility, good adhesion to dentin and low shrinkage.
The disadvantage of glass ionomer cements is the difficulty of removing them from root canals. Although, according to the author, it is relatively easily removed from the root canal using ultrasound.
Also, the “dislike” of many doctors for this material is explained by the fact that due to the short hardening time, high-quality lateral condensation is difficult. When it goes beyond the apex, severe pain occurs. However, with improved manual skills, these problems can be easily eliminated.
Epiphany
In modern endodontic practice, gutta-percha is recognized as a weak link. Although the requirements for optimal instruments for root canal preparation are generally known and achievable, it is impossible to hermetically fill the root canal with gutta-percha. In fact, coronal restoration, not gutta-percha, is one of the cornerstones of success in endodontic treatment. Most materials used for coronary repair would be much more successful if they could be efficiently placed into a long, narrow canal and just as efficiently removed if complications arise after treatment.
Research has shown that the Epiphany obturator system combined with Resilon is more resistant to microleakage (6 times more) than a gutta-percha obturator system. The Epiphany system, combined with Resilon obturation material, strengthens the root by more than 20% compared to standard obturation techniques.
Advantages of the Epiphany obturator system: seals better; strengthens the root; easy to remove; provides immediate coronary sealing;
The main component of the Epiphany obturation system is Resilon, a root canal obturation material with a soft resin thermoplastic synthetic polymer backing. It contains bioactive glass and radio-resistant fillers in a resin matrix. The material is similar to gutta-percha in handling, physical properties and radiographs. It has the same properties for successful unfilling and re-treatment, softens under the influence of high temperatures, dissolves in solvents like chloroform, remains thermoplastic at low temperatures, and is biocompatible. Like gutta-percha, there are main cones in all ISO sizes, as well as additional cones in a variety of sizes available.
Resilon is based on a resin that, in combination with Epiphany dual-cure sealer and Epiphany primer, is bonded into the root canal in the form of a monoblock. The emerging monoblock also helps to strengthen the obstructed root - by filling the root canal, coronal sealing occurs, thereby eliminating the possibility of pathogenic bacteria penetrating into the apex. By replacing gutta-percha and the usual filler with materials from the Epiphany obturation system, there is no need to change the canal obturation technique. The fundamental point is the complete cleansing and formation of the channel.
The author, having worked with Epiphany material for a rather short time, nevertheless made an attempt to reflect his impressions of this material:
Because Epiphany obturation can be light cured immediately after filling the canal, an immediate coronal seal will occur. This will save the patient from having to visit again.
Epiphani can be used with any obturation technique and has high radiopacity.
If it is necessary to remove Epiphany from the canals, there are no difficulties; it is easily removed, no more difficult than gutta-percha with zinc oxide sealant.
Today, Epiphany represents an alternative to gutta-percha-based obturation systems, due to the fact that it has all the advantages of gutta-percha, but at the same time it is free from the disadvantages of gutta-percha.
Despite the introduction into practice of a large number of materials for filling root canals, many endodontists, unfortunately, prefer to use materials based on zinc oxide eugenol paste for these purposes.
Today, the success of endodontic treatment is a reality. Many of our happy patients, having gotten rid of pain, will agree with this. However, incorrectly performed techniques cannot be considered successful solely on the basis of the patient’s lack of obvious symptoms.
We are our own harshest critics and set too strict criteria for success. For oncological diseases, doctors consider survival to be 5 years a success, and for femoral prosthetics - 3-5 years. Are these numbers arbitrary? Do they have a real basis? Do doctors consider them reasonable if most of their patients fit within this 3-5 year period? Should we, like this, strive for short-term success or should long-term failure be anticipated in dentistry?
We must not deceive ourselves. Failures do happen and will continue to occur, despite the great efforts of doctors and the constant improvement of techniques. Our goals may be noble and lofty, but we cannot always achieve them, and this is often due to the fact that we are dealing with a human body that does not always behave as it is written in books.
Sealers
Pastes for filling root canals are usually self-hardening. They consist of two mixing components and have different chemical compositions.
The dental materials market offers a large number of sealers of the most varied composition from various competing manufacturers. Below the author provides a list of sealers currently used, and also mentions some materials that are no longer used.
Table No. 1. Sealers currently available on the market and their composition (in alphabetical order).
| 1. Acroseal (Septodont) | epoxy resin matrix containing calcium hydroxide |
| 2. AH 26, two versions (Dentsply) | matrix based on epoxy resin; composition options: with and without silver additives |
| 3. AH plus/AH plus Jet (Dentsply) | based on epoxy-amine polymers (AH plus Jet: automatic mixing system) |
| 4. Apexit Plus (Ivoclar Vivadent) | contains calcium hydroxide (base?) |
| 5. Endomethasone N (Septodont) | based on zinc oxide eugenol, currently free of formaldehyde |
| 6. Gangraena-Merz N (Merz Dental) | calcium hydroxide-based material that can be used for both temporary and permanent filling of root canals |
| 7. Hermetic (lege artis) | cement based on zinc oxide-eugenol for permanent filling of root canals |
| 8. Ledermix MTA | MTA cement for endodontic treatment of perforations or retrograde filling of root canals, as well as for apexification in the treatment of teeth with incomplete root formation |
| 9. N2 Endodontic Cement (Hager & Werken) | based on zinc oxide eugenol, with a reduced (!) formaldehyde content compared to the previous version of the composition (but still contains formaldehyde) |
| 10. Perma Evolution (Becht) | polymer based on epoxy resins |
| 11. RealSeal (Sybron Endo / Kerr) | thermoplastic synthetic polymer with bioactive (?) and radiopaque glass fillers |
| 12. rocanal r2 permanent vital (la Maison Dentaire) | cement based on zinc oxide-eugenol for permanent filling of root canals after vital pulp extirpation |
| 13. rocanal r3 permanent gangrene (la Maison Dentaire) | cement based on zinc oxide eugenol for permanent filling of root canals after treatment of gangrenous pulpitis, contains 5% orthophenylphenol (!) and 0.5% nitrofurazone (?) |
| 14. Sealapex (Sybron Endo / Kerr) | polymer, contains calcium hydroxide |
| 15. 2Seal (VDW) | based on epoxy-amine resin |
| 16. GuttaFlow (Roeko) | system for filling canals with cold gutta-percha in combination with a central gutta-percha pin (Master-Point) |
| 17. RoekoSeal (roeko company) | based on polymethylsiloxane (silicone), expands slightly during curing (0.2%) |
The list, for example, mentions material N 2 (, Sargenti), containing toxic formaldehyde. Currently, the material is no longer used in Germany. The list also includes the still widely popular material Endomethasone N (Septodont). Currently, the composition of the material has been slightly changed compared to the previously used original Endomethasone material. In the Endomethasone N material, the content of anti-inflammatory drug components (corticoids, diiodothymol) is significantly lower. These components in sealers have been subject to intense criticism for several decades in student textbooks and scientific papers.
Pastes for filling root canals are usually self-hardening. They consist of two mixing components and have different chemical compositions. The list of materials for filling root canals also includes hardening two-component sealers based on polymers (the polyketone-based material Diaket is no longer produced). The dentist has at his disposal various polymer-based sealer systems (AH plus, Sealapex, Apexit, etc.), as well as silicone-based systems (Roeko Seal). Such materials are highly elastic and have a relatively low final hardness. Due to this property, root fillings made from such materials are easily removed during endodontic revision (retreatment).
It is surprising that the nature of the chemical composition of sealers is completely different. There is no evidence-based medicine yet on whether calcium hydroxide (Ca(OH)2) additives are advisable in such materials.
According to the author, the “favorite” material of German dentists in clinics and dental offices is currently AH plus (Dentsply). Many scientific articles are devoted to this material. AH plus consists of two paste-like components mixed in equal parts and is very easy to use. The material replaced the previously widely used sealer AH 26 several years ago. The sealer AH 26 was developed back in 1954 (Schroeder), it released a small amount of formaldehyde (!) (Schäfer, Hickel, 2000). For this reason, the material in its original composition is no longer used.
However, this drug has its advantages and its adherents. Modern material AH 26 supposedly does not contain formaldehyde. And the currently used N2 Endodontic Cement material based on zinc oxide eugenol still (!) contains formaldehyde, but in a “reduced” concentration compared to the previously used similar material.
It is the use of formaldehyde, as well as chlorophenol-camphor-menthol (ChKM) drugs, that is the subject of debate in university circles. All eminent university teachers do not recommend the use of these drugs.
However, at present there is a time of “renaissance” for the Jodoform-Paste material, which contains the drug chlorophenol-camphor-menthol and has long been considered obsolete. According to modern publications, this material is again recommended for use in pediatric dentistry (endodontic treatment of baby teeth).
New materials based on glass ionomers and salicylates with calcium hydroxide additives, as well as MTA (mineral trioxide aggregate) cement, are currently undergoing the test of time in endodontics.
It is noteworthy that there is no single concept regarding the composition of a good “standard” sealer. Each manufacturer offers its own composition options.
There is no single concept regarding the composition of a good sealer. Each manufacturer offers its own option. Rubber-like, highly elastic preparations based on silicones are also advertised and used as materials for filling root canals. For example, the fairly commonly used material Roeko Seal has the property of expanding in volume by approximately 0.2% when cured. This property of the material should ensure a particularly good fit of the root filling to the walls of the root canal.
On the other hand, silicones have the ability to absorb moisture in small quantities. Are root fillings made from silicone-based materials really impervious to bacteria? The author still has serious doubts about this.
Thus, the variety of paste sealers offered for filling root canals is very large. And not only because they are represented on the market by a large number of competing manufacturers, but also due to the diversity of the composition of materials.
Endodontics is still a broad field of experimentation, especially in the field of root canal fillings.
Sealers - cements for sealing root canals
The main purpose of the sealer is to ensure complete filling of the root canals, tightness and easy insertion of the pin. The requirements for sealers are for the most part the same as for pins. Only fluidity, the need for slow hardening and careful adhesion to the channel walls are added. At the moment, dentists have a large selection of sealers at their disposal, however, none of them meets all the requirements.
Natural sealers
Natural cements tend to dissolve in tissue fluid, do not adhere well to walls and can stain the enamel over time.
| Cement Endomethasone N Poudre (Septodont) | pros: presence of aseptic additives, anti-inflammatory effect, radiopacity, easy introduction into the canal, slowly dissolves. Disadvantages : when filling canals with endomethasone, there is a risk of an allergic reaction and painful sensations when cement gets into the periapical tissue, as well as when it comes into contact with the mucosa, it contains toxic components. |
| Cortisomol powder (Pierre Rolland) | pros: radiopaque, due to the content of steroid hormones in the composition, it allows you to relieve postoperative pain, contains anti-inflammatory components. Disadvantages : due to the presence of dyes in the composition, it is not suitable for the restoration of anterior teeth, stains the enamel, and dissolves in tissue fluids. |
| Filling material Tubliseal (Kerr) | pros: rapid hardening under the influence of temperature and moisture, thanks to the composition it penetrates well into all microcracks in the tooth cavity. Disadvantages : it is quickly washed out of the canals; although corticosteroids have a positive effect in the postoperative period, they subsequently weaken the protective functions of the periapical tissues. |
| Specialized material Canason Combipack (Canason) | pros: has an antiseptic, anti-inflammatory and antibacterial effect, reliably isolates the canal, mixes easily and is clearly visible on x-rays, not absorbed. Cons : filling canals with Canason paste is a lengthy process. |
Polymer sealers
Polymer sealers, unlike natural ones, dissolve much less in tissue fluids, adhere better to root dentin, do not stain tooth enamel, and are more preferable materials for canal filling.
| Paste AH Plus (Dentsply) | pros: slight shrinkage of the filling, good connection with dentin, ideal sealing of the canal, long hardening period, easy penetration into microcracks and tubules. Disadvantages : possible allergic reaction and hypersensitivity to the components of the paste upon contact with the mucous membrane; it is necessary to mix the paste from two tubes. |
| Sealant sealer Adseal (META Biomed) | pros: complete sealing, absence of dyes and negative effects on tooth enamel, insolubility in tissue fluid, high level of radiopacity, biocompatibility with other materials. Cons : Possible irritation upon contact with periapical tissues. |
| Eugenol-free polymer sealer Diaket (ESPE) | pros: good adhesion and radiopacity, the material is plastic, does not shrink when hardening, does not irritate the mucous membrane and periapical tissue, has antibacterial properties. Disadvantages : low level of cytotoxicity, reaction with gutta-percha pins (during the insertion process they stretch and deform), pain symptoms for 2-3 days after filling the tooth. |
Glass ionomer cements
Glass ionomer cements consist of two components: liquid and powder. Since their main disadvantages are low strength and low aesthetic values, most often such materials for filling root canals are used in pediatric dentistry on baby teeth. Glass ionomer cements perfectly absorb liquid from dentin, thereby increasing their adhesiveness. However, due to the same hydrophilicity, such fillings must be coated with a protective varnish on top.
| Ketac-Endo (ESPE) | pros: high level of adhesion and good radiopacity, low degree of shrinkage, anti-caries effect due to the fluorine released by the filling. Disadvantages : small margin of safety, porosity, roughness, erosion, minimum filling installation time - a day. |
| Endion, Voco | pros: biological compatibility of the material with dental tissues, antibacterial components, absence of toxic components. Cons : the material is opaque, subject to rapid destruction, and not suitable for chewing teeth. |
Polydimethylsiloxanes
Polydimethylsiloxanes are sealants whose small particle size gives the material excellent ductility. It is this quality that contributes to the sealing of all microcracks and channels.
| RCA RoekoSeal (Roeko) | pros: insoluble, has a high level of biological compatibility with dental tissues and adhesiveness, has antimicrobial properties, a minimal level of shrinkage and expansion during polymerization. Cons : a fairly small volume of clinical studies conducted using this type of material. |
Cements containing calcium hydroxide
Cements containing calcium hydroxide are most often produced in the form of a set of two pastes, one of which contains calcium hydroxide. The main problem of this substance is its rapid dissolution under the filling, however, thanks to special additives, this property of calcium hydroxide has been minimized. Currently, filling dental canals with cement containing calcium hydroxide is very widespread.
| Apexit (Ivoclar Vivadent) | pros: if the dental cavity is not thoroughly cleaned, the material reacts with the remains of the pulp, turning it into hard calcified tissue, easily removed during repeated treatment, radiopaque, does not shrink, low solubility, complete sealing and compatibility with biological tissues, long-term storage of the finished cement at room temperature . Disadvantages : low strength, it is necessary to apply an insulating gasket under the material. |
| Sealapex (Kerr) | pros: bactericidal properties, absence of carcinogenic components, therapeutic effect, does not change the color of the tooth and permanent filling, ease of mixing the paste, good fluidity and adhesiveness to the canal walls. Disadvantages : sealapex canal filling must be spot-on, cannot be applied in a thick layer, and is destroyed under heavy loads on the tooth surface. |
Other obturation methods
A unique method of filling root canals is the so-called Russian Red, which was previously used in the countries of the Eastern Bloc, including in the former GDR. This filling material is a resin-based polymer in nature. Once cured in the channel, the material turns red and becomes incredibly hard. It is very difficult to remove from the root canal during root canal revision (only with the help of aggressive solvents). However, after filling the root canals with this material, a revision has to be carried out quite rarely, since teeth with these old root fillings are most often miraculously completely “cured” without causing complaints. The author cannot give an explanation for this phenomenon.
After Russian Red root canal filling, teeth are miraculously completely “cured.” With other exotic methods of filling root canals, completely different paste-like sealers without gutta-percha are used. Although these methods save time, such root fillings are less airtight. Therefore, such methods are generally not recommended, even within the framework of “generally available endodontic treatment.” There is still no evidence-based medicine for these methods.
At the beginning of the article, two very labor-intensive methods of root canal filling were already mentioned, which differ significantly from each other: lateral condensation (compaction) of gutta-percha using several pins and vertical condensation of heated gutta-percha. These treatment methods, as well as their various modifications/mixed variants, belong to private dental services in the field of endodontics and are outside the scope of public health insurance. Their use requires a lot of time and the purchase of expensive devices, so they can be classified as expensive private dental services, most often provided in dental offices specializing in endodontics, as well as in university clinics.
Materials for filling
The main purpose of dental canal filling is to fill the cleaned tooth cavity. Since root canals go deep into the gums, the material filling them is constantly in contact with periodontal tissues, i.e. in fact, canal filling is nothing more than an operation to replace damaged body tissues with an artificial analogue.
The requirements for the material used are very strict:
- It must absolutely hermetically isolate the canal from possible penetration of all kinds of bacteria through the apical opening.
- An important factor is the absence of an allergic reaction, dissolution and decomposition upon contact with periapical tissues and tissue fluid.
- Another important condition is radiopacity, i.e. The substance must be clearly visible in the image, otherwise it will be difficult for the doctor to understand whether the filling is installed properly. If the treatment is unsuccessful, the material should be easily removed from the root canal; moreover, when it hardens, it should not shrink and air cavities should not form inside.
Over the years, the root canal filling procedure has undergone many changes, with new methods and materials being tried. However, a universal material that satisfies all of the above requirements has never been found. That is why most dentists currently practice filling with combined materials. Next, we will consider the maximum number of materials currently used.
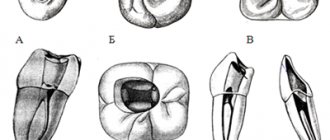
Lateral condensation (compaction)
With this method, sealer is first introduced into the root canal using an instrument, or the main (first) gutta-percha pin (Master Point) is wrapped in sealer and inserted into the root canal. Then, additional gutta-percha pins of a smaller ISO size (usually ISO size 25) are inserted next to the central main pin. To provide space for additional tapered pins, a special compaction tool (spreader) is used. The spreader is introduced into the root canal with some pressure and pushes the filling material already present in the canal to the opposite walls, and then removed from the root canal. After this, another additional gutta-percha pin is inserted into the root canal.
With this method, five, six or even more additional gutta-percha points can be inserted into the root canal. After completing the procedure for inserting the pins, before cutting off their protruding ends, such a root filling looks from the outside like a “bouquet” of flower stems without leaves.
The advantage of using this method is the ability to select pins of different sizes for the root filling consisting of several parts of the “gutta-percha core” and individually fit them in the root canal. In this way, it is possible to obtain a reliable and hermetic root filling, with a tight marginal seal, even in areas of the root canal that do not have a round cross-section.
In practice, the dentist almost never encounters the round cross-section of the canal, and the lateral condensation method is considered the “gold standard” for filling root canals. The actual clinical situation often looks very different from the idealized phantom root canal filling on plexiglass blocks that is taught in endodontic workshops. In practice, a dentist is faced with any shape of the canal cross-section, but not a round one. It is precisely because of this discrepancy between theory and practice that in some textbooks, including modern ones, the lateral condensation method is considered the “gold standard” for filling root canals, if we do not take into account another method (vertical condensation), which will be presented in the final parts of the article.
When carrying out endodontic treatment within the framework of public health insurance, a mixed method of filling root canals can be used: at least one very wide root canal or a canal with an oval cross-section is filled with several gutta-percha points using the labor-intensive lateral condensation technique, and narrower root canals with only one central pin in combination with sealer. The author has been using this “mixed” method for several decades.
Obturation using the Thermofil system
“Thermophile” is a titanium, plastic or steel cone-shaped rod coated with gutta-percha, which is in the alpha phase state. This coating is characterized by a lower melting point, increased fluidity and the ability to penetrate into the microtubules of the root passage. When introducing thermophile into the root canal, the base rod fills the main space, and gutta-percha fills only a small part of it. This is what makes it possible to solve the problem of significant shrinkage of the thermoplastic gutta-percha filler after cooling and to prevent the formation of microspaces between the walls of the root passage and the filler.
The procedure for sealing root passages, which involves the use of the Thermofil system, consists of the following stages:
- selection of suitable thermophile diameter;
- antiseptic treatment of the rod and its heating;
- introduction of sealant into the root canal;
- inserting the rod into the root canal until it stops;
- removal of excess gutta-percha from the dental cavity;
- restoration of a damaged tooth crown.
The use of the described technique allows for effective obturation of the main canal and its branches.
Vertical condensation
This very labor-intensive method of filling root canals is based on the use of hot (heated) gutta-percha. First, the apical part of the root canal is filled with heated and largely softened or almost liquid gutta-percha, and then compacted by machine (condensed).
This part of the vertically condensed gutta-percha root filling is called Downpack according to the English terminology currently used in Germany.
For compaction, heated instruments are used to keep the gutta-percha in a softened state until it is completely compacted. To condense gutta-percha, among many other systems, rotating instruments are used, which, due to the release of heat during friction, help to soften part of the Downpack root filling.
The part of a root filling made of vertically condensed gutta-percha is called a Downpack according to the English terminology currently used in Germany. The root canal filling technique, first described by Schilder in 1967, is very labor-intensive because it requires special devices for heating and condensing gutta-percha. In addition, tapered Master Points are required, which must exactly match the taper and volume of the root canal or the last instrument used to develop the root canal. Then, before inserting into the root canal, the gutta-percha pins are shortened at the apex by 0.5-1 mm so that if there is significant compaction (condensation) in the canal, the material is not removed beyond the apical opening.
In addition, according to the Schilder technique, the Master Point is first fitted into the root canal, after which a control radiograph is taken, which verifies the correct seating of the pin in the canal. Only after this is its final condensation in the root canal.
After filling the apical third, the middle and upper parts of the root canal (Backfill) are also filled with heated gutta-percha, which is injected directly into the canal using a syringe. To do this, gutta-percha is preheated in a special device (oven) to a liquid state. This labor-intensive method results in root fillings that adhere very well to the walls of the root canal.
Due to their almost perfect tightness, such seals effectively prevent the penetration of bacteria into it.
This is what the technique of vertical condensation of gutta-percha looks like in general. However, there are various modifications of Schilder's original method. Some dentists create a new “ideology” from every new little thing they come up with and do not allow the slightest deviation from “their” concept. The choice of one or another method of canal filling depends to a certain extent on the beliefs of the dentist.
Dental manufacturing companies have been very successful in making money from endless variations of the vertical condensation method, selling pluggers and ovens for preheating gutta-percha, as well as “special gutta-percha.”
Injection methods, Ultrafil, Thermafil
Recently, the method of introducing heated (liquid) gutta-percha using special syringe systems directly into the canal (Obtura system) has also begun to be used. In this case, gutta-percha, heated to a temperature of 160-200 ° C (!), is introduced directly into the root canal using a special injection needle (cannula) of sizes 40 and 60 according to ISO standards.
With this method of canal filling, there is no need to use a sealer. However, the high temperatures used can, in direct contact with tissues, lead to burn damage to surrounding tissues (at the root apex?).
The dentist also has some other systems at his disposal, in which only slightly heated gutta-percha is used, rather than heated to a molten state (Ultrafil, Thermafil). With this method of application, gutta-percha softens a little, after which it is very easy to apply it to those parts of the root canal of the tooth that are not round in cross section.
Thermafil and Thermafil-Plus systems are widely used. This method uses plastic pins coated with gutta-percha. Pin sizes are standardized according to ISO standards. Such a pin is heated for a short time in a small electric oven and, during a short plastic phase, the heated gutta-percha is inserted into the root canal. The protruding excess pin is cut off. But even with this method, accidental pushing of heated gutta-percha into the apical region is possible.
The method of filling root canals using the Thermafil system is quite economical, therefore, in some dental offices aimed at a certain social contingent, patients do not need to pay an additional amount: the treatment is carried out within the framework of state health insurance.
Charging additional fees for endodontic treatment as part of “cash” services from patients insured by public health insurance funds can sometimes be quite problematic. So, unfortunately, the question once again arises: are innovations like the Thermafil system applicable in everyday dental care, if this is associated with even minor additional costs?
The “Central Pin Technique” and Thermafil or Ultrafil systems are economical, effective and realistically applicable in the provision of services within the framework of public health insurance. A dental office that primarily serves patients under public health insurance is faced with a difficult dilemma. And in such a situation, it is the Thermafil system that could find its application within the framework of “generally available endodontic treatment”. However, the question of whether with this method it is necessary to additionally use sealers or whether heated gutta-percha ensures sufficient tightness of the root filling is still being discussed. Saving time does not always benefit the patient.
In dental offices, mainly serving patients under public health insurance, the most often used, described in detail at the beginning of the article, is the very economical “central pin method” in combination with two-component paste sealers.
The author came to these conclusions after numerous discussions on this issue with colleagues during numerous master classes and meetings of quality control groups.
As mentioned above, this standard method of root canal obturation, if necessary, can be easily modified by using additional gutta-percha pins of the “lateral condensation” type, for example in the distal root canals of molars that are very wide or do not have a round cross-section, as well as for filling “large caliber” root canals in incisors and canines.
The author successfully uses the central pin method, as well as the method of “partial” lateral condensation, in his practice and has obtained good treatment results when filling root canals within the framework of state health insurance services (more than 4000 root fillings).
The author uses AH Plus sealer to fill root canals. The only question that remains is which of the many described methods can be considered standard for endodontic treatment within the framework of public health insurance.
The author is convinced that such a method could be the “central pin technique” in combination with a two-component sealer (containing calcium hydroxide), as well as the use of Thermafil or Ultrafil systems. These methods are economical, effective and therefore really applicable in the provision of services within the framework of public health insurance.
This topic should be discussed in professional circles in order to resolve the question of how endodontic treatment can be included in the list of services provided under public health insurance. And it is possible that, based on methods confirmed by evidence-based medicine, such endodontic treatment can be carried out at a much higher quality level. This is certainly doable.
Filling methods
For many years, the main method of filling canals in Russia was filling with one paste. Of course, this method is very simple, does not require much time and is relatively cheap, however, it has a number of significant disadvantages:
- Firstly, not every paste has sufficient fluidity to seal all the microscopic holes in the dental canal.
- Secondly, during the filling process, voids appear in which pathogenic bacteria can subsequently develop.
- Thirdly, almost all pastes, after hardening, shrink the filling material and dissolve when in contact with tissue fluids; moreover, most of them also give an allergic reaction when interacting with periapical tissues.
That is why recently a wide variety of methods have appeared for filling canals. Let's take a closer look at them.
Depophoresis
None of the currently existing methods of filling dental canals can guarantee the absolute tightness of the filling. As a result, an infection may remain in the remaining microcracks in the root canal, which subsequently resumes the inflammatory process. This is why the depophoresis method, which allows the introduction of medications into the entire root canal system using a device of the same name, is so useful and unique. In fact, this method is aimed at complete sterilization of the canal.
Thanks to depophoresis, it is possible to treat teeth with the most curved and hard-to-reach canals, to treat previously filled teeth from which it is not possible to remove the filling material, as well as those teeth in which there is a particle of a broken instrument or the apex of the root of which is affected by a cyst.
In difficult cases, the depophoresis procedure itself can be performed several times with a difference of 1-2 weeks. And although the cost of the procedure is not as low as we would like, the results of treatment with this method are truly amazing. First of all, depophoresis helps maintain the hardness of the tooth, protects against the destruction of tooth tissue with removed pulp for many years, and also ensures complete sterility of the contents of the dental canal, which eliminates reinfection.
Obturation with Thermofil system
One of the clear advantages of the Thermofil system is that it allows you to seal not only the main root canal, but also most of the lateral tubules, and in case of repeated treatment, the treatment of sealed tubules will not cause any major problems for the dentist.
Thermophiles are plastic carriers coated with gutta-percha. After introducing a small amount of sealer into the canal to ensure better sliding and contact with the surface, the rod is heated in a special oven, inserted into the canal to the required depth and cut. Heated gutta-percha, due to its fluidity, fills all the cavities of the canal. The advantage of this system is its relative simplicity, speed and reliability. The only drawback of the method is the frequent removal of the filling material outside the root canal.
Filling with cold gutta-percha
Filling root canals with cold gutta-percha is divided into four subtypes:
| Single pin method | The essence of this method is to give the canal the desired shape, select the appropriate size of gutta-percha pin, which is inserted into a previously prepared tooth and trimmed with a heated instrument. In this case, the pin must lie close to the walls of the canal. An obvious disadvantage of this filling method is the lack of complete three-dimensional obturation of the entire canal, although it is better than the monopaste filling option. |
| Lateral (side) condensation method | Filling canals using the lateral condensation method has proven its high efficiency, reliability and simplicity over many years of use. However, when filling canals using this method, there is a high risk of root fracture. The essence of this filling is to densely fill the canal with gutta-percha pins lubricated in a hardening sealer. First, the central pin is inserted, and then the side ones, each subsequent one to a smaller depth until the material is completely compacted. The protruding ends of the pins are cut off. With this technique, it is rarely possible to achieve uniformity of the filling material, which can lead to the development of periodontal inflammation. In addition, the use of lateral condensation implies a uniform canal cone and an apical shoulder, which prevents the material from escaping beyond the tooth. |
| Thermo-mechanical condensation of gutta-percha | Another name for this method is filling the canal with a rotating condenser. Today, this method is practically not used, because has a lot of disadvantages. In particular, the risk of tool breakage inside the channel is very high, because it rotates at great speed. Part of the gutta-percha sticks to the instruments, which leads to the formation of voids. Moreover, this filling method does not ensure the closure of all canal cavities. |
| Method of filling with chemically softened gutta-percha | Another way to fill tooth canals with cold gutta-percha is chemical softening, or otherwise the immersion method. Despite the fact that this method of filling was one of the first, it is currently not used due to the poor quality of canal obturation, severe deformation of the material after the evaporation of solvents, and the inability to eliminate shrinkage of the filling. |
Filling with heated gutta-percha
Filling root canals with heated gutta-percha is also divided into four different subtypes:
| Injection (liquid) gutta-percha | The technique of filling canals with liquid gutta-percha uses material heated to two hundred degrees and fed into the canal in liquid form. This method ensures good penetration of gutta-percha not only into the central canal, but also into the lateral tubules and microcracks, while minimally damaging the tissue. The only requirement for using this method is the professionalism of the doctor. |
| Vertical condensation of gutta-percha | Another way to fill tooth canals with hot gutta-percha is the vertical condensation technique. The disadvantage of the method is its complexity and duration. Initially, heated material is placed into the canal, which is subsequently directed by instruments towards the apical foramen and lateral tubules. After complete sealing, a softened pin is inserted into the center, and excess material is removed. In this way, three-dimensional filling of the root canal is achieved with maximum use of gutta-percha and minimal sealer. |
| Continuous wave | This technique is a variation of the previous method and consists of two successive steps. First, the central pin is inserted into the canal with an instrument heated to two hundred degrees and cut off in the middle third, then pins of the same size are sequentially inserted in the same way with an instrument heated to one hundred degrees until the canal is completely filled. The advantage of this method is its ease of implementation compared to the previous one and also complete sealing of the canal. |
| Injecting gutta-percha with a syringe | The thermoplastic injection technique involves injecting molten gutta-percha into the root canal using a special syringe. This method is simple, quick and convenient, but it does not ensure filling of the side canals, and sometimes the gutta-percha does not reach the top of the root canal, which is why the work has to be redone. |
E&Q Plus system
The mixed version of canal filling using the E&Q Plus system is recognized by dentists as one of the best today, since this system allows you to fill the canals of the same tooth in different ways.
The main tools of this method are an injection gun and a handpiece with attachments, which heats the gutta-percha directly in the canal itself. Due to the constant compaction of heated gutta-percha, complete three-dimensional obturation is achieved in the canal, after which further filling can be done either using a gun or using the vertical condensation method.
Resorcinol-formalin mixture
The method of filling canals using a resorcinol-formalin mixture is not recommended for use in modern dental practice, since it has a lot of side effects: a large number of complications and repeated visits, the carcinogenic and toxic effect of the formaldehyde included in the composition, staining the tooth pink.
The essence of the method is to fill the canal etched with the mixture with a paste containing zinc oxide and resorcinol-formalin additives. According to statistics, complications when using this method occur in seventy-five percent of cases out of a hundred.
Mummification of the impassable part of the root canal
Another method, the use of which is currently extremely limited. Mummification is the impregnation of the soft tissues of the pulp with strong antiseptics in order to prevent its decomposition and inflammation. To carry out this procedure, mummifying components are added to the filling paste, which gradually dissolve and leave the tooth cavity. The effectiveness of such fillings is extremely low and is recommended for use only in the treatment of baby teeth. True, side effects may also occur here due to the release of carcinogenic substances by the mummifying components, causing general intoxication of the body.
Thus, having considered all the currently available methods of filling dental canals, we can conclude that the use of gutta-percha is so far the safest and most universal. And, despite the fact that dentists are actively looking for alternatives to this material, it can be assumed that in the coming years this option will remain the most popular among doctors and patients for endodontic treatment.
You just have to want it
For specialists in this case, the field of activity remains endodontic treatment in particularly complex root canal anatomy, as well as in particularly complex clinical situations, and for “particularly gifted” specialists - perhaps complex cases of root canal revision.
There is enough work for everyone. In any case, this would benefit “general-profile” therapeutic dentistry.
The article was provided by the magazine of the official publication of the Association of Dentists of Lower Saxony (Germany) NZB - Niedersächsisches Zahnärzteblatt (No. 6, 2011, pp. 31-34).
Translation by Inna Bichegkueva.