Giuseppe Cantatore University of Verona (Italy). Department of Endodontics. Assistant professor.
In a classic study published in 1985, Bystrom et al. compared the sterilizing effectiveness of three different methods of endodontic treatment of infected canals and found that mechanical treatment in combination with irrigation with saline solution ensures canal sterility in 20% of cases, while replacing NaCl with a 5% sodium hypochlorite solution leads to canal sterility in 50% of cases. cases, and the addition of the latter scheme with a single temporary filling of the canal with calcium hydroxide increases the percentage of canal sterilization to 97%. Does this mean that when treating infected root canals, temporary filling with medicated paste is required in all cases? More than 15 years have passed since the Bystrom et Al study; Today we know much more about the properties of microorganisms associated with pulp-periodontal pathology: from virulence to mobility, from the ability to penetrate dentinal tubules to sensitivity to various antiseptics. 15 years of research experience have shown that many irrigation solutions have pronounced bactericidal activity against microorganisms such as enterococcus faecalis or candida, which are resistant to calcium hydroxide or chlorophenol. In this article, we will discuss in 7 points how to improve the root canal irrigation procedure, using the right products in the right sequence, in order to reduce the need for additional medicinal treatment of the canals between visits.
Key Factors for Effective Cleaning and Irrigation of the Root Canal System
1. Careful diagnosis of existing pulp-periodontal pathology
2. Taking into account the condition of the tooth tissues and the complexity of the anatomy of the root canal system 3. Removal of the endodontic smear layer 4. Compliance with indications when choosing means for irrigation 5. Optimization of the active components of the irrigation solution 6. Correct sequence of application of the irrigation solution during root canal treatment 7. Mandatory costs of at least 5 minutes for irrigation before filling
Root canal irrigation protocols
One of the reasons for the failure of endodontic treatment is the problem of high-quality root canal irrigation.
Irrigation has two major goals:
- Cleansing the root canal system due to the chemical dissolution of organic and inorganic residues, as well as their mechanical washing out with a stream of liquid;
- Disinfection of the root canal system, high-quality preparation and formation of the root canal helps to create the necessary reservoir for the irrigation solution and opportunities for its activation.
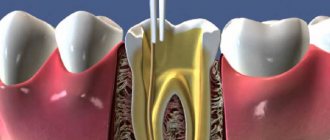
The root canal system has a very complex morphology, which is often characterized by the presence of lateral canals and anastomoses, and a branched structure in the apical part.
In the event of pulp death, dehydration of the dentinal tubules occurs, in the lumen of which only tissue decay of the processes of odontoblasts remains; the migration of microorganisms and toxins easily occurs along the lumen of the tubules; the dentinal tubules may contain bacteria that penetrate into them both from the oral cavity and from the root canal system. Since these bacteria can lead to failure of endodontic treatment, they must be eliminated.
During the preparation of hard tooth tissues with hand or machine instruments, a microscopic layer of sawdust is formed on the surface of the dentin. The smear layer formed during endodontic treatment is characterized by a high content of organic components in the form of pulp fragments, odontoblasts, and weakly mineralized predentin. At the same time, there are also inorganic components, the source of which is dentin. In this regard, to remove the smear layer from the walls of the root canal, it is necessary to use solutions that are effective against both organic and mineral components.
The smear layer of the root canal may contain microorganisms and serve as a breeding ground for them, as well as disrupt the adhesion of filling materials to the walls of the root canals. In connection with the above, the smear layer of the root canal must be completely removed. Peritubular dentin, highly sensitive to EDTA or acid solutions, is completely dissolved.
Irrigation solutions
- Sodium hypochlorite
Sodium hypochlorite (NaOCl) has both oxidizing and hydrolyzing properties: it has bactericidal and proteolytic effects. The solution was proposed for use as a wound irrigant as early as 1915, and began to be used as an irrigant solution for endodontics in the United States around 1920.
Many studies have demonstrated its antiseptic and solvent properties. In particular, NaOCl has a rapid bactericidal effect against vegetative forms, spore-forming bacteria, fungi, protozoa and viruses (including HIV, rotavirus, HSV-1 and -2, hepatitis A and B viruses). The exact mechanism of the antimicrobial activity of NaOCl is not entirely clear, but it may be determined by the formation of hypochlorous acid and the release of active chlorine, which leads to the oxidation of sulfhydryl groups of important bacterial enzymes. Sodium hypochlorite has pronounced dissolving properties against pulp residues, even those located in lateral and additional canals.
The dissolving effect is determined by the concentration of sodium hypochlorite: the maximum severity of the effect is manifested in a 5% NaOCl solution. To increase the effectiveness of sodium hypochlorite as a solvent for tissue decay, it is recommended:
- use a heated solution with a temperature of about 40°C;
- activate and heat the solution using ultrasonic files;
- use temporary root canal filling with calcium hydroxide to take advantage of the synergistic effect of these two substances;
— EDTA components
EDTA is used in endodontics in the form of a liquid or gel as a chelating agent that extracts calcium ions from hydroxylapatite, thereby dissolving the mineral fraction of the smear layer of the root canal O'Connell in a recent study indicates that the isolated use of EDTA without sodium hypochlorite does not In one case, it did not ensure complete removal of the smear layer of the root canal. This explains the advisability of alternating EDTA-containing agents and hypochlorite during endodontic treatment; their combined effect provides an excellent degree of cleaning of the dentinal walls in the apical third of the root canal, provided that both substances are brought to the apex and activated using ultrasound or manual files
— Acidic components
The acids used in endodontics for washing canals are phosphoric and citric in concentrations from 6% to 30%. Acid solutions are highly effective in removing the mineral component of the smear layer of the root canal and in the treatment of obliterated canals. However, since their effectiveness as antiseptics and organic solvents is limited, combined use with sodium hypochlorite is recommended. One recent study examined the effectiveness of two different combinations of irrigation solutions (NaOCl + EDTA and NaOCl + phosphoric and citric acid) for smear layer removal. The results obtained indicate that both concentrations were effective, although the use of EDTA was characterized by a more gentle effect on peritubular and intertubular dentin.
After using acids, it is recommended to rinse the canal with distilled water, since there is a tendency for crystallization and precipitate to form on the canal walls.
— Chlorhexidine
The dissolving effectiveness of chlorhexidine relative to organic and mineralized tissues is not expressed. Chlorhexidine can be used for short-term temporary filling of root canals.
You cannot combine chlorhexidine with hypochlorite; a carcinogenic precipitate called parachloraniline is formed!
You can do this: Hypochlorite - distilled water - chlorhexidine.
Irrigation sequence during root canal preparation
- Remove the roof of the pulp chamber and rinse with sodium hypochlorite to remove residual pulp and identify root canal orifices;
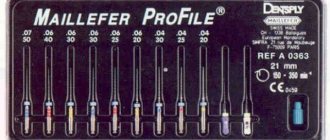
- Begin instrumental treatment of the canal lumen, alternating it only with sodium hypochlorite;
- When starting to excise dentin, fill the canal lumen with EDETAL material.
- Continue instrumentation
- Rinse the channel with sodium hypochlorite until foaming stops;
- Complete the instrumentation, ensuring that the canal always remains filled with EDETAL, flushing the canal with sodium hypochlorite after every 3-4 instruments;
In the vast majority of cases, some of the canals remain untreated and unfilled, and the results of endodontic treatment, despite this, are satisfactory. This is the merit of a good immune system. But in many cases, insufficient cleaning of the root canals leads to unsuccessful results of endodontic treatment.
An attempt should be made to dissolve the remaining pulp tissue using chemical methods, and then, if possible, completely remove it from the root canals. This is the purpose of continuous root canal irrigation.
What concentration of hypochlorite should I choose? There are as many opinions as there are authors.
Very interesting research by Dr. David Sonntag: "Sodium hypochlorite at a concentration of 1 to 5.25% is by far the most suitable solution for chemical cleaning of the root canal system. NaOCl has the unique ability to dissolve necrotic tissue debris as well as organic components of the smear layer. However the activity of chlorine in the root canal can be exhausted within two minutes at the first stage of tissue dissolution. Therefore, in the process of developing the canals, irrigation should be carried out constantly with new portions of the solution. The effectiveness of the antimicrobial and tissue-dissolving effects of an aqueous solution of sodium hypochlorite increases with increasing concentration of the solution. However, the reduction in the number of bacteria in the canal after root canal irrigation with a 5% solution is no higher than after using a 0.5% solution for this purpose (Bystrom and Sundqvist, 1985; Cvec et al., 1976). When using a solution of 1% concentration, the necessary tissue dissolving effect is achieved. Since the concentration of a solution may decrease with changes in temperature or exposure to light, it is possible that, practically speaking, it would be better to use the solution in higher concentrations. To increase the effectiveness of NaOCl, it is advisable to heat the solution, for example, to 55 °C. When the temperature increases by 5° in the range from 5 to 60 °C, the bactericidal effect of NaOCl more than doubles. A 1% NaOCl solution at a temperature of 45 °C is as effective at dissolving organic tissue residues as a 5.25% NaOCl solution at a temperature of 20 °C. At the same time, the toxicity of a one percent solution and, accordingly, the risk of using such a solution in a heated state is much lower . A chlorhexidine solution (obviously, regardless of concentration) does not have the ability to dissolve tissue.
For complicated forms of pulpitis and periodontitis, a protocol with chlorhexidine is proposed:
The irrigation protocol is as follows: sodium hypochlorite 5.25% - distilled water - EDTA 17% - distilled water - chlorhexidine
The intermediate irrigant should be distilled water to prevent as much as possible the chemical interaction between the remainder of one solution and another solution introduced into the canal on different bases (alkaline and acidic). Chlorhexidine does not need to be washed out of the canal; it is enough to just dry the canal, since it does not affect the polymerization and adhesive properties of obturation materials. After this, it is necessary to evacuate moisture from the canal using paper points, while it is important not to overdry the root canal, so as not to make the dentin more fragile.
A little more about EDTA. In gel form, EDTA-based preparations are an excellent lubricant, ensuring better contact of the cutting tool with the cut surface, which also increases the efficiency of machining the tooth canal. Many authors point out another interesting property of EDTA gels. They optimize the electrical conductivity of the root canal system during apex location. It is believed that apeslocation carried out in the presence of a large amount of lubricant gives the most accurate results.
Omega Dent produces two EDTA-based drugs:
- "Edetal liquid"
- "Edetal gel"
The gel has a foaming effect, which promotes better evacuation of dentinal filings that arise during the mechanical treatment of the canal.
Sodium hypochlorite solutions also facilitate mechanical treatment of the canal along with EDTA preparations. There are techniques in which only sodium hypochlorite is used to soften the dentinal canal wall, which, however, can make the apex locator readings less accurate due to the high electrical conductivity of the solution. Preparations based on sodium hypochlorite are the most active antiseptics. This property is due to a high degree of electrolytic dissociation with the release of atomic oxygen and chlorine. The release of gases promotes foaming, which, as already mentioned, facilitates the evacuation of the canal contents during preparation.
"Omega Dent" produces: preparations "Hypochloran-3" and "Hypochloran-5", containing 3.25% and 5% sodium hypochlorite.
In modern endodontic practice, various concentrations of sodium hypochlorite solutions are used. There is a well-established opinion that the antiseptic activity of this antiseptic depends not so much on its concentration as on exposure, that is, the time of exposure of the solution to the contents of the canal. With longer rinsing, the canal is better cleaned mechanically and a larger number of microorganisms die and leave the canal. The antiseptic properties of solutions are also significantly enhanced when heated. However, only a 5% concentration of sodium hypochlorite solution has proteolytic properties, which is important in the treatment of periodontitis teeth, the canals of which are filled with pulp decay, microorganisms and their toxins. But it is important to consider that the entry of sodium hypochlorite solutions into the oral cavity causes such unpleasant reactions in patients that it may make it impossible to continue treatment. Therefore, the use of a rubber dam is mandatory when performing endotherapy.
To obtain a 0.5% solution, hypochlorite 3% concentration should be diluted with distilled water in a ratio of 1:5 and heated to 37 degrees.
As a result of the purulent-inflammatory process in the pulp and periodontal tissues, the infection penetrates through the dentinal tubules and into the thickness of the root dentin. Therefore, the traditional method of antiseptic treatment of the root canal does not guarantee against its reinfection. Based on this, along with the traditional method of canal treatment, it is necessary to carry out temporary root obturation with sterile calcium hydroxide for a prolonged antiseptic effect on the root canals.
General concept and rules of conduct
Irrigation is the cleaning and disinfection of the root canal of a dental element. Everyone who has visited the dentist at least once has encountered a similar procedure. Treatment of the oral cavity with a special device, from which liquid under pressure is supplied to the future area of work, allows you to reduce the concentration of bacteria and pathogenic microbes, eliminating the likelihood of inflammation developing when the cavity is opened.
In endodontic treatment techniques, irrigation is considered one of the key processes to get rid of excess microorganisms, residual dentin elements and tissues. In this case, the solution used should not provoke the patient to a negative reaction or stimulate the gag reflex. The choice of the optimal composition should be based on the results of tests that make it possible to identify the causative agent of the pathology - this requires diagnostics, including x-rays.
The procedure includes several manipulations performed by the dentist:
- external examination of the condition of the pulp and assessment of the periodontium;
- analysis of the tissue structure characteristic of the affected element;
- assessment of the specific structure of root canals;
- careful removal of the upper dentin layer;
- compliance with safety standards when working with aggressive compounds;
- consistent implementation of antiseptic procedures.
When planning to install a filling, the doctor should allocate at least five minutes for irrigation - this period is enough to clean the oral cavity from bacteria and possible pathogens. Otherwise, the risk of infection increases.
Temporary canal filling
If indicated, the doctor can fill the canals after depulpation not with filling material, but with a medicinal agent (antibacterial, anti-inflammatory). The drug remains in the tooth cavity for a certain time, after which it is removed, and the vacated canal is sealed.
The procedure can be prescribed:
- if there is a need to sanitize the canals if a deep infectious process is suspected;
- if the patient has acute periodontitis;
- for temporary sealing of the canal, if it is necessary to monitor the condition of the tooth cavity after removal of the inflamed pulp.
In addition, the procedure can be prescribed for tooth injuries, for example, a fracture of the crown or root.
Treatment regimen
- Diagnostics Before treatment, an x-ray or computed tomography must be done to determine the number of channels, their location and shape.
- Anesthesia The doctor selects an anesthetic and, if necessary, conducts sensitivity tests to various drugs.
- Installation of a rubber dam An obligatory aspect of modern treatment is the isolation of the tooth from oral fluid using a special latex scarf (rubber dam).
- Instrumental and medicinal canal treatment The essence of root canal treatment is high-quality disinfection of the tooth cavity. To do this, the doctor expands the canal with instruments, gives it the desired shape and rinses it with disinfectant solutions to destroy the infection.
- Preparing the canals The doctor measures the length of the canals using an apex locator, after which they are mechanically expanded and smoothed out the walls.
- Filling canals Cement, a pin, or a combination of both are injected into the prepared cavities, depending on the chosen treatment method.
- Control image The doctor evaluates the quality of canal filling, after which he performs tooth filling and other necessary procedures. In addition, the patient receives recommendations for further oral care.