Osteosarcoma (or osteogenic sarcoma), which is sometimes not quite correctly called bone cancer, is the most common malignant tumor of the skeletal system.
Some numbers and facts:
- In most cases, osteosarcoma is diagnosed at a young age - from 10 to 30 years.
- The prevalence of the disease is highest among teenagers, but this does not mean that people of other ages cannot get sick.
- Every tenth case of osteogenic sarcoma occurs in people over 60 years of age.
- Among other cancers, osteosarcoma is rare. In children it makes up 2% of all types of cancer, in adults it is even less.
Most often, osteosarcoma occurs where the growth plates are located - closer to the ends of long bones. Favorite places for tumor localization: the knee area (lower end of the femur and upper end of the tibia), upper part of the humerus. Much less common are lesions of other bones: the pelvis, jaws, etc. Rare localizations are in most cases found in older people.
General information
Primary tumors of the skeletal system are rare. They are observed between the ages of 15 and 40 years, that is, children, adolescents and young people are more often affected. In 10% of cases, the disease is detected in people over 60 years of age - in them the tumor may be associated with radiation or develop against the background of benign diseases of the skeletal system. The term “bone cancer” is applied to various types of oncopathology of the skeletal system. Among malignant tumors of this system, the most common are osteogenic sarcoma (synonymous with osteosarcoma in 50-60% of cases), Ewing's sarcoma (the second most common type of tumor), chondrosarcoma , giant cell tumor , fibrosarcoma .
Secondary bone tumors (bone metastases) are much more common. The source of metastatic tumors are primary tumors of the lung, prostate, breast and thyroid gland. Bone sarcomas are a group of tumors of nonepithelial origin. In 80-90% of sarcomas, they are highly malignant tumors that are localized in different bones of the skeleton. However, the tubular bones most often affected are the femur and tibia. The tumor develops in the metaphyses (growth part) of long bones, especially in the area of the knee joint. Men get sick more often than women. An increased risk of the disease is observed with genetic abnormalities: hereditary retinoblastoma and Li–Fraumeni syndrome .
General information about the disease
The most common location of a malignant tumor is long bones (80% of cases). Most often the femur, its distal part, is affected. The pathology also affects:
- foot bones;
- flat bones;
- spine;
- Hands;
- skull (in rare cases).
In most cases, the tumor forms near the joints (metaphyseal area). Less commonly, the tumor occurs in the central part of the bone. Experienced doctors who treat osteosarcoma abroad can guess where the tumor is based on the location of the pain.
Osteosarcoma is an aggressive malignant pathology that tends to metastasize through the bloodstream. Metastases of this tumor often affect the lungs, lymph nodes, and somatic organs. From the start of treatment until the appearance of metastases, it can take from two to nine months. Most patients are diagnosed with multiple metastatic lesions of the lungs. Single lesions are detected in approximately 10% of patients.
Pathogenesis
Carcinogenesis is triggered under the influence of many factors, which include:
- radiation treatment for other cancers;
- suppression of tumor suppressor genes;
- prosthetics performed;
- hereditary diseases;
- complex chromosomal aberrations.
Frequent deletion, as well as loss of heterozygosity of 3q13, are specific aberrations for osteosarcomas. One of the tumor suppressor genes is localized in this region, which regulates cell proliferation and plays a major role in tumor pathogenesis. 3q12 deletion is associated with progression and poor prognosis.
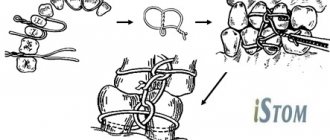
An important morphological feature of bone tumors is the infiltrative nature of growth, or circular (encompasses the entire area of the bone around the circumference). The tumor spreads through the bone marrow spaces and replaces them, destroys and surrounds the bone beams. Neoplastic cells are characterized by severe cellular atypia. The architecture of the newly formed bone determines the tumor potential.
Classification
The most common malignant bone tumors are:
- osteogenic sarcoma;
- Ewing's sarcoma;
- chondrosarcoma;
- fibrosarcoma;
- parosteal sarcoma;
- fibrous histiocytoma;
- lymphosarcoma.
Bone sarcoma
The most common tumor develops from osteoblasts and in the process of neoplasm develops altered, atypical bone. This tumor is called differently - synonyms are osteogenic sarcoma, osteosarcoma, osteoidsarcoma, osteoblastosarcoma. Chondrosarcoma and fibrosarcoma are distinguished as independent forms.
Classic osteosarcoma is a highly malignant intraosseous tumor. If a tumor appears in an unchanged bone, it is a primary sarcoma; if it develops after irradiation or against the background of Paget’s disease , it is a secondary sarcoma. The tumor affects the metaphysis (growth zone) of the tubular bone of the arm or leg. Active growth processes occur in the metaphyses, so they are associated with a high risk of tumor transformation. The appearance of a tumor is associated with the rapid growth of bone tissue.
The peak incidence is observed in children aged 10-14 years. They are more likely to affect the tubular bones of the leg - osteosarcoma of the femur in the hip joint, as well as the bones of the knee joint (femur and tibia). When the femur is affected, a large lesion zone of 5-10 cm is revealed. Hemorrhages , necrosis and cystic cavities are found in the newly formed bone. The tumor gradually destroys the periosteum. Sarcoma of the hip occurs at any age, but is more common in young men.
It is characterized by aggressive growth and metastasizes early. Malignant formation of the knee joint in most cases is a secondary metastatic process and less often - as a primary process. In adults, osteosarcoma affects the spine and maxillofacial bones. This type of tumor rarely develops in the area of the coccyx, shoulder girdle, ulna and humerus. Primary osteosarcoma of the ribs is less common, but secondary (metastatic) tumors predominantly affect the ribs, vertebrae and pelvic bones. Malignant transformation of Paget's disease to sarcoma occurs in 1% of cases and the peak incidence occurs at 60 years of age and older. Of all the bones, the jaw is the most commonly affected. Jaw cancer is a tumor with rapid aggressive growth and early metastases to the lungs (most often). There are isolated cases of metastases to the stomach and soft tissues. Damage to the lower jaw is somewhat more common than to the upper jaw (corresponding to 58% and 42%).
Hand bone cancer in most cases is metastatic. In the bones of the skull there are various types of primary sarcomas, as well as secondary metastatic tumors from the primary focus (uterus and prostate). Skull bone tumors cause headaches due to compression of the brain. Spinal cancer is characterized by active growth and rapid progression. Patients develop movement disorders: when the lumbar region is affected, the lower limbs and the functions of the pelvic and genital organs are affected. Cervical spine cancer is very dangerous and requires immediate treatment. When the cervical vertebrae are damaged, the functions of the arms and legs are affected.
Ewing's sarcoma
This type of tumor occurs in children and adolescents. Develops in bone tissue and soft tissues. It is aggressive and metastasizes quickly. There is a high mortality rate in the first year of diagnosis. If we consider damage to the inert system, then in 70% this type of tumor occurs in tubular bones, flat bones (scapula, ribs) and pelvic bones. Compared to osteosarcoma, the diaphyses of bones are more often affected. Many patients have genetic mutations that cause disruption of cell differentiation processes.
Chondrosarcoma
The neoplasm develops from cartilage tissue. Occurs in people over 40 years of age. The course of this type of cancer is difficult to predict. In some, chondrosarcoma develops slowly, while in others it develops very quickly and metastasizes . This type of tumor affects any bone, but the femur and pelvic bones are predominant. The tumor can also develop in flat bones (scapula, skull, ribs). Most often, the course of chondrosarcomas is slow and metastases appear late. The appearance of pain is characteristic, and when the pelvis is damaged, the nerve roots are involved, therefore, in addition to pain, the function of the pelvic organs will be impaired.
Fibrosarcoma
A rare tumor that develops from connective tissue. Tumor cells are located between the collagen of the connective tissue and look like a spindle. In most cases, fibrosarcoma appears after radiation treatment.
Classification of osteosarcomas according to the TNM system
- T0 - no data on the tumor process.
- T1 - formation no more than 8 cm.
- T2 - neoplasm larger than 8 cm.
- T3—tumor continuity is disrupted.
Involvement of lymph nodes (“N”) is rare, since bones do not have a lymphatic system. But if there are metastases to the nodes, this is a poor prognostic sign. Regional lymph nodes are nodes that correspond to the location of the primary tumor.
- N0 - no metastases in the lymph nodes.
- N1 - metastases are present.
Osteosarcoma is characterized by the development of hematogenous metastases, which in the diagnosis of o. By the time of diagnosis, 20% of patients already have small metastases in the lungs. Metastases can also be in the pleura, pericardium, bones, kidneys, and central nervous system.
- M0 - no distant metastases.
- M1 - distant metastases are present (“a” - to the lungs, “b” - to organs and tissues).
An important point is histological examination, which confirms the diagnosis, determines the type of tumor and its malignancy. There are five forms of osteosarcomas, with different degrees of differentiation.
Metastatic bone lesions
The course of metastatic bone lesions is not asymptomatic - pain is the first manifestation of bone metastases. Most patients describe it as unbearable. Patients with metastases also experience:
- pathological fractures of tubular bones;
- vertebral compression fractures;
- spinal cord compression;
- hypercalcemia.
A quarter of breast cancer have fractures of long bones associated with destruction of the cortical layer. radiation therapy or surgery is required .
Benign bone formations
Bones are affected by benign tumors ( chondroblastoma , fibrous dysplasia , osteoclastoma , aneurysmal cyst and others), with which a malignant formation must be differentiated.
Aneurysmal bone cyst
A benign tumor-like bone lesion, which is characterized by the proliferation of connective tissue. It contains cavities filled with blood. A distinctive feature of this cyst is its spread through the epiphyseal plate, as well as to adjacent bones. The cyst appears at any age, but more often in adolescents and children. Its most common location is the bones of the spine, the distal part of the femur, the proximal part of the humerus and tibia, and the pelvic bones. A secondary cyst is formed after damage to benign chondroblastoma , fibrous dysplasia , giant cell tumor and malignant neoplasms - osteogenic sarcoma .
Chondroblastoma
A benign tumor that forms at the articular ends of a bone. It develops from chondroblasts and resembles mature cartilage tissue. It is characterized by slow growth and a favorable course, but there is information about cases of a malignant course or malignancy by chondroblastoma. Like all bone tumors, it affects children and adolescents, and in rare cases, older people. Clinical manifestations are pain and swelling of the joint. Treatment is surgical. The prognosis is favorable.
Reasons and forms
The most common form of spindle cell sarcoma has two types: small cell and large cell. The spindle-shaped shape of the cells is especially pronounced in small cell sarcoma. The large-cell variety is characterized by polymorphism of cellular elements, and along with spindle-shaped cells, round and, often, branched cells are observed. Both varieties have a common feature - the development of powerful cords consisting of closely lying cells of the described shape. The stroma is rather weakly expressed, especially in the early stages of tumor development. On each preparation, strands are visible in longitudinal, oblique and transverse sections. Round cell sarcomas and pigmented tumors developing in the jaw area do not differ in histological picture from the same tumors of other organs.
The rapid growth of sarcoma and its tendency to extensively invade neighboring organs, no less than in jaw cancer, make it difficult to determine the primary focus of sarcomatous growth. Often the jaw is affected secondarily, for example, when the initial lesion is localized in the nasal cavity. With primary damage to the jaw, sarcoma develops either from the central part of the bone, or the primary source of malignant growth is the periosteum. Accordingly, in relation to the lower jaw, two forms of sarcomas are distinguished: central, arising from the cancellous bone of the bone, and periosteal. The source of sarcoma of the jaws can also be the connective tissue of the submucosal gum and the periodontium of the tooth.
Sarcoma is characterized by a rapid increase in tumor mass: this sign is, to a certain extent, important in the differential diagnosis. Large sarcomatous tumors without ulceration are often observed, which is very rare in cancer. Periosteal sarcomas of the lower jaw envelop the outside with a thick layer of bone and early cause protrusion and displacement of the surrounding soft tissues. The floor of the mouth rises on the diseased side, the tongue shifts to the healthy side. Often, bone substance takes part in the structure of these tumors: bone plates begin to form in the tumor mass, sometimes having a radial arrangement, sometimes anastomosing with each other. These bone plates make up the skeleton of the tumor.
Central sarcomas of the jaw are often intraosseous giant cell tumors. For a long time, these formations were described as “striped”, “brown” tumors. Their tendency to intratumoral hemorrhages and to the formation of necrosis of significant parts of the tumor is striking, accordingly, alternating red and yellow areas are visible on the section of the tumor. This picture is very typical for the described group of tumors. Growth is relatively slow, but, in any case, until the cortical layer breaks through. As it germinates, the latter begins to show signs of increased growth. In advanced cases, it is sometimes difficult to decide whether the tumor originates from the periosteum or from the central parts of the bone.
With sarcoma of the upper jaw, especially coming from the periosteum of the outer wall, there is a very large deformation of the face with a sharp displacement of the eye, nose and corner of the mouth.
Causes
The causes of bone tumors are not well understood. To a certain extent, bone cancer is caused by:
- Chronic diseases of the skeletal system ( osteomyelitis , Paget's disease , benign tumors ).
- Smoking.
- Injuries.
- Foreign body in the bone (orthopedic implants). Tumors of the skeletal system are more often detected in patients who have had implants used for osteosynthesis or have undergone joint replacement. Dentures use hexavalent chromium, which is a carcinogen.
- Previous radiation therapy , which induces the development of osteosarcoma. Radiation-induced sarcomas develop 3 years after irradiation.
- State of immunodeficiency .
- Skeletal abnormalities ( Olier disease ).
- Mutations of the p53 gene and the retinoblastoma Rb1 gene.
- Hereditary diseases ( retinoblastoma , Li-Fraumeni syndrome , Rothmund-Thompson syndrome , Werner syndrome , absent thumb).
- Benign bone tumors that can become malignant.
- Taking the drug Natpara (a drug for the treatment of hypoparathyroidism ). This drug increases the risk of osteosarcoma.
There is evidence of an increased risk of osteosarcoma in children born weighing more than 4500 g and above average height. However, in most patients no specific factors are identified.
Reasons for development
It is still unclear why soft tissue sarcomas occur, but certain risk factors have been identified.
Genetic predisposition
- nevoid basal cell syndrome (Gorlin syndrome);
- neurofibromatosis (von Recklinghausen disease);
- tuberous sclerosis (Bourneville disease);
- Gardner's syndrome;
- Werner's syndrome.
Carcinogens
The risk of developing angiosarcomas increases significantly with previous exposure to phenoxy herbicides (2,4-dichlorophenoxyacetic acid, 2,4,5-trichlorophenoxyacetic acid) and dioxins.
Immunosuppression
The most striking example is Kaposi's sarcoma in people with AIDS, autoimmune hemolytic anemia, and organ transplant recipients.
Most patients come with a complaint of tumor growth after an injury or bruise. There is no connection between trauma and the development of soft tissue sarcomas.
Symptoms and manifestations of bone cancer
A characteristic manifestation of malignant bone formation of any location is constant, aching pain, disturbing for several weeks or months, not eliminated by analgesics and increasing over time.
For a long time, patients associate the appearance of pain with a former injury, so they do not consult a doctor and this becomes the reason for a late diagnosis. Pain from bone tumors does not depend on physical activity and bothers patients even at rest. Sarcoma is characterized by pain that worsens at night and relief does not occur in any position of the limb. Symptoms of osteosarcoma also include swelling of the tissue in the area of the tumor. But local swelling appears later - at first it is a deeply located tumor in the soft tissues, and then the swelling area increases, the affected area swells, and a venous network appears on the skin, sometimes the skin turns red.
When joints are affected, swelling appears in their area. Cancer of the knee joint or any other joint disrupts the function of the joints - they bend poorly and movement is limited. Movements are impaired not only when there is a tumor in the joint, but also in the nearest joint when the bone is damaged. A tumor of the joints changes their shape. In some cases, effusion appears in the joint cavity.
Photo of osteosarcoma of the knee joint
Bone cancer is accompanied by fragility, so patients often experience spontaneous fractures due to minor trauma. When the tumor process affects the spine, difficulties appear when walking, weakness in the limbs, and paretic phenomena. A tumor of the leg bones is accompanied by numbness of the limb and lameness. Symptoms of advanced bone sarcoma include abdominal pain, nausea and vomiting, which is associated with increased levels of calcium in the blood ( hypercalcemia ) due to bone breakdown. In the advanced stage, general symptoms are also noted - fatigue and weight loss. The appearance of general symptoms indicates a process with metastasis.
Symptoms of jaw cancer
Osteosarcoma that occurs in the thickness of the jaw is called central, and that developing in the peripheral parts is called peripheral. For a long time, signs of bone cancer do not appear. Then pain appears that is not associated with tooth pathology. Long-lasting pain should alert the patient. The tumor process can be recognized using radiography and MRI. With a tumor formation in the lower or upper jaw, pain in the teeth occurs for no reason and radiates to the ear and eye. It gets worse at night and becomes unbearable, forcing patients to wake up and take painkillers.
Palpation of a tumor in any part of the jaw is painful. In addition, osteogenic sarcoma of the jaw changes the sensitivity of the trigeminal nerve and causes changes in tooth position. The teeth within the tumor become mobile. paresthesia and anesthesia occurs (Vincent's symptom).
Photo of sarcoma of the lower jaw
As the jaw grows, it becomes deformed. The tumor quickly grows, spreads to the surrounding tissues and compresses them, causing exophthalmos and congestion in the soft tissues. Lymph nodes are often not enlarged. The mucous membrane of the alveolar process at the site of the tumor is red and swollen, and when the mucous membrane is injured, ulcers appear on the gums. In some cases, osteosarcoma festeres (the temperature rises, weakness and malaise appear).
Symptoms
Clinical manifestations and severity of symptoms depend on the primary location and size of the tumor.
Most often, soft tissue sarcomas of the head and neck are asymptomatic.
May be observed:
- pain;
- paresthesia is a disturbance of sensitivity along the course of peripheral nerves, which can manifest itself as burning, numbness, tingling;
- nerve palsies;
- trismus – spasm of the masticatory muscles, which is characterized by limitation of movements in the temporomandibular joint;
- ulceration of the mucous membrane;
- dysphonia is a phenomenon characterized by impaired vocal function;
- dysphagia – difficulty swallowing.
When soft tissue sarcomas are located near the nose, nasal congestion may occur that does not go away over a long period.
Tests and diagnostics
- X-ray of the affected area in two projections. X-ray examination covers the entire affected bone and joints nearby. This is necessary in order not to lose sight of the “step-by-step” metastases. With osteosarcoma, the x-ray picture may be different. A large tumor node with unclear outlines. The cortex and medulla of the bone are affected. The tumor destroys the periosteum, often revealing a “cloud-shaped” component, which is associated with uneven ossification of the tumor. In the newly formed bone, osteosclerotic and osteolytic (sparse) areas alternate. However, areas of bone change become visible on x-ray when the tumor grows to a certain size. Therefore, to avoid diagnostic errors, you need to use MRI and CT.
- MRI and CT provide layer-by-layer visualization of bone, bone marrow, soft tissue and connective tissue. They are carried out with contrast. These methods clarify the size of the lesion, the exact location and spread of the tumor beyond the bone.
- To detect distant metastases, a CT scan of the chest and abdominal pelvis is performed. Chest X-ray also reveals metastases in the lungs.
- To identify lesions in other bones, skeletal scintigraphy (radionuclide scanning) is prescribed.
- The main method to confirm the disease is a biopsy and histological examination of the obtained material. The patient's bone tissue is collected and the type of tumor is determined. Tissue collection is carried out by excision of the bone, which makes it possible to obtain sufficient material. If the lymph nodes are enlarged, a biopsy (puncture) is also performed.
- Histological examination. To make a diagnosis, detection of neoplastic tissue (osteoid) is mandatory. The amount of osteoid is not important because it is different in different fields of view. Osteoid is produced by tumor cells and may be found adjacent to or surrounding the cells.
- Angiography. Detects vascular damage.
- Molecular genetic diagnostics. It determines the presence of mutations in the genome. This is necessary to determine the need for targeted therapy (biological).
Specific markers for osteosarcoma are currently unknown. Sometimes patients are prescribed a CEA test. Let's find out how necessary this is. Carcinoembryonic antigen , what is it? This is a tissue marker of cancer. What does this marker show? This type of protein is detected in minute quantities in a healthy person, but during the oncological process its level increases.
Determination of this antigen is used to diagnose the following tumors:
- colon and rectum;
- stomach;
- mammary gland;
- pancreas;
- lungs;
- metastases to the liver and bones (the sensitivity of the method in the metastatic process is much lower).
This test is not specific for malignant tumors, since an increase in antigen is observed in inflammatory and autoimmune diseases, benign tumors (intestines, liver, pancreas), liver cirrhosis , hepatitis , Crohn's disease , tuberculosis , pneumonia , cystic fibrosis . During a malignant process, the level increases throughout the entire period of the disease. CEA analysis is used to monitor the effectiveness of treatment of malignant neoplasms. A decrease in its level during the course of treatment indicates a positive result. The norm of carcinoembryonic antigen for non-smokers: 0-3.8 ng/ml, the norm for women who smoke is slightly higher than 0-5.5. A negative result does not exclude cancer.
Diagnostics
The diagnosis is made based on histological examination of tumor tissue.
There are two methods for obtaining material for research:
- core needle biopsy;
- open biopsy.
The biopsy should be performed in the location that during the operation will be included in the area of excision of the tumor formation.
Diagnostic algorithm:
- Examination: A lumpy, rounded yellow or gray nodule may be observed. It can have different densities and consistencies. Soft nodes - with liposarcomas, dense - with fibrosarcomas, jelly-like formations - with myxomas;
- Complete blood count with calculation of leukocyte formula and platelet count;
- Biochemical blood test with determination of liver and kidney function indicators (including electrolytes);
- Coagulogram;
- MRI of the head and neck area;
- CT scan of the lungs;
- Ultrasonography;
- Radioisotope study of skeletal bones (for myxoid liposarcomas);
- CT scan of the brain (for alveolar soft tissue sarcoma and hemangiopericytoma).
Important: for the purpose of initial examination and clarification of the stage, routine PET scanning is not recommended.
In children
Among all tumors in children, 5% are bone sarcomas : 3% osteosarcoma and 2% Ewing sarcoma . The lack of alertness among doctors and the atypical nature of the course greatly complicate early diagnosis. Osteosarcoma in children in half of the cases is localized in the knee joint (the femur and tibia are affected). In second place is damage to the metadiaphysis of the humerus. The most common symptom of osteosarcoma is constant, dull pain with a gradual increase. Most children have a soft tissue component - swelling and an increase in the volume of the limb. Weight loss and fever at the onset of the disease are rare.
Ewing's sarcoma occurs before the age of 17 years, but the peak incidence occurs between 12 and 15 years of age. Boys are most often affected. Ewing's sarcoma, unlike osteosarcoma, does not synthesize osteoid . Often this tumor is located in the scapula, ribs, vertebrae, pelvic bones, as well as the femur, fibula, and humerus. Unlike osteosarcoma, flat bones are affected. Signs of Ewing's sarcoma are increasing pain, tissue swelling, dysfunction, and fever. The soft tissue component is more pronounced than bone destruction. An increase in local temperature due to the appearance of hemorrhages and necrosis in the tumor complicates diagnosis, since osteomyelitis is suspected. Neurological symptoms are associated with nerve damage.
Combined treatment for Ewing's sarcoma:
- Chemotherapy courses (standard drugs for this pathology).
- Surgery (similar to osteosarcoma).
- Radiation therapy. It is carried out on the area of the primary tumor and on distant metastases.
Treatment
Thorough removal of a malignant tumor within the boundaries of healthy tissue is the most reliable way to treat sarcoma of the jaw. The features of jaw surgery are determined by the need to restore as best as possible after removal of all affected parts both the external appearance of the face and very important functions: eating and chewing food, isolated nasal breathing and speech.
Typical operations are possible only in cases where the tumor extends within the bone and is surrounded by an unchanged bone or fibrous capsule, pushing aside the adjacent soft tissue. Then it is possible to relatively easily extirpate the tumor and enlarged lymph nodes and maintain normal soft tissue relationships, the shape of the face and, subsequently, restore the skeletal defect.
Less typical operations for sarcoma of the jaw, in which parts of the muscles, salivary glands, tissue, mucous membrane and skin have to be excised along with the bone, give a worse prognosis, both in terms of relapse and in relation to the immediate outcome of the operation and the immediate restoration of the defect. Nevertheless, here too it is very important to immediately, within the limits of the possible, form the natural outer walls of the oral cavity, thanks to which the patient retains the ability to speak and eat food more or less normally.
In young people, with fairly well-defined sarcomatous tumors, complete removal of the tumor is easier, and restoration should be carried out as completely as possible. The skeletal defect is initially replaced by a prosthesis and can subsequently be restored by free bone grafting. After removal of large cancerous tumors in old age, the main focus should be on thoroughly removing all diseased tissue and keeping recovery to a minimum. Large defects in the mucous membrane and skin lead to severe wrinkling of soft tissues with scars, which, as a result, poorly retain the prosthesis and are subsequently unsuitable for bone transplantation. The possibility of relapse is often a contraindication to any irritation of a healed surgical wound by either a prosthesis or plastic surgery. Complete closure of the surgical defect with large plastic flaps is not indicated in some cases because it subsequently makes it difficult to control local relapse and prevents radiation therapy.
The information presented in this article is intended for informational purposes only and cannot replace professional advice and qualified medical care. If you have the slightest suspicion that you have this disease, be sure to consult your doctor!
Diet
Dietary table No. 1a
- Efficacy: therapeutic effect after a week
- Terms: 3-10 days
- Cost of food: 900-1100 rubles per week
Diet table No. 5a
- Efficacy: therapeutic effect after 5-7 days
- Time frame: 2-6 weeks
- Cost of products: 1300 - 1400 rubles per week
Diet 11 table
- Efficacy: therapeutic effect after a month
- Terms: 2 months or more
- Cost of products: 1800-1900 rubles. in Week
of diarrhea while undergoing chemotherapy . In this regard, a diet excluding spicy, fatty foods containing fiber (vegetables, nuts, seeds, bran bread) is recommended.
Fried foods and simple carbohydrates, which increase intestinal motility, are also excluded. A balanced diet during this period should contain a sufficient amount of protein (boiled meat, fish, steamed cutlets, meat soufflé). Dishes must be pureed - soups, cereals, meat. During this period, you can use Diet No. 1B and No. 5P . When diarrhea disappears and the patient’s condition improves, the patient is transferred to Table No. 11 . The diet of this diet is suitable for the recovery period. The patient’s diet is complete, containing the necessary vitamins, nutrients and minerals. Daily calorie content is increased (3000 kcal). Food is taken in 5 divided doses. The goal of the diet is to normalize weight while reducing it and improve the function of all body systems.
All foods and cooking methods are allowed, but nevertheless, it is better to adhere to a healthy diet, in which preference is given to stewed, boiled or baked dishes, vegetable and cereal soups that are not fried. To replenish vitamins, the diet should contain fresh seasonal vegetables, fruits and berries. It is important to choose healthy and natural products that do not contain dyes, flavor enhancers or preservatives. The diet must contain dairy products: natural milk, kefir, cottage cheese, cheeses, yogurt. Dairy products are important for replenishing calcium, which is constantly lost from bones. The calorie content of the diet should not be increased by fatty foods, cakes, cream pies, semi-finished products, beef and lamb fat, fatty sausages, ready-made sauces, pastes, mayonnaise, and sweet carbonated water.
Prevention
There is no specific prevention. However, you can perform non-specific activities:
- Observation and treatment of precancerous diseases of the skeletal system. Processes that tend to become malignant include chondroma, fibrous degeneration, Paget's disease, and osteochondral exostoses. The malignancy rate of these benign formations reaches 15%. It is important to undergo follow-up examinations annually to detect malignancy at an early stage. Healthy lifestyle. Balanced diet. Avoiding injuries and occupational hazards.
Secondary relapse prevention includes:
- The use of drugs that restore the immune system after chemotherapy and radiation therapy .
- Complete nutrition, rich in vitamins, antioxidants, proteins.
- Rejection of bad habits.
- Prevention of viral infections.
- Preventive examinations with an oncologist. Local relapses can be detected visually. It is important to have examinations during the first 4 years. After this, local relapses are rare.
- Carrying out diagnostic procedures according to the protocol. Metastases develop in 95% of cases within the first 5 years and most often affect the lungs. Bone metastases present with pain, and they appear simultaneously with pulmonary metastases.
Characteristic signs of osteosarcoma
The triad of clinical manifestations characteristic of osteosarcoma:
impaired mobility of the affected limb;- the appearance of swelling;
- pain that gets worse over time.
These signs can be attributed to many diseases of the musculoskeletal system, so there is a possibility of misdiagnosis. The Meir Clinic in Israel conducts examinations using advanced programs and uses the latest equipment, so errors in diagnosis are excluded in the hospital.
Depending on the clinical signs, the disease is divided into two types:
- rapidly developing osteosarcoma - the disease begins suddenly, is accompanied by severe pain and rapid progression; if the patient does not go to the hospital in time, the outcome will be unfavorable;
- slowly developing osteosarcoma - the disease manifests itself poorly; if you consult a doctor in a timely manner, bone cancer treatment abroad will be successful.
Tumors that grow rapidly metastasize to the lungs. Such metastases are detected during the first diagnostic procedures. Often aggressive forms of the disease are found in children.
Pain is a cardinal symptom of the disease. At first, the pain is moderate and intermittent, often occurring during physical activity. Pain appears when the disease spreads to the periosteum. As the disease progresses, the intensity of the pain increases and it is constantly present.
A high degree of intensity is characterized by osteosarcoma, which develops in the bones near the lower leg. The pain often occurs at night, and there is no sign of a deterioration in the person's general health. Some patients note a slight increase in body temperature.
The main diagnostic indicator of osteosarcoma is swelling in the affected area. It occurs against the background of tumor progression, while the soft tissues located above the tumor become tense, a shine appears on the skin, and the subcutaneous veins dilate. As a result, the mobility of the affected limb is limited - it bends poorly, and the patient begins to limp. Gradually, the muscles of the limb atrophy.
General clinical signs of osteosarcoma occur in the later stages of the disease and are manifested:
- general malaise;
- losing weight;
- weakness;
- insomnia;
- Pathological fractures often occur in 10% of patients.
To ensure a good prognosis for osteosarcoma, it is necessary to visit the clinic at the first signs of pathology and undergo advanced cancer treatment in Israel.
Consequences and complications
The course of the disease itself is complicated by fractures and infection of soft tissues. All bone cancers after treatment have consequences:
- Secondary cancer , which develops as a result of exposure to radiation.
- Chronic heart failure (exposure to doxorubicin ).
- Osteoporosis.
- Hearing and vision impairments.
- Renal dysfunction and renal failure .
- Endocrinopathies.
- Impaired fertility ( infertility ). Reproductive functions suffer after chemotherapy with alkylating drugs ( Ifosfamide , Carboplatin , Cyclophosphamide ) and after the use of radiotherapy in the pelvis, abdomen, and spine. Menstrual irregularities are always observed after high-dose chemotherapy and stem cell transplantation.
- The consequences of the operation are significant - after amputation, limb prosthetics and long-term rehabilitation are necessary.
Forecast
The prognosis of osteosarcoma is determined by many factors: age, size, localization, stage, “purity” of the resection margin, histological conclusion.
How long do people live with bone cancer? With complex treatment of osteosarcoma, 70% of patients live 5 years or more, with Ewing's sarcoma - 60% of patients.
Some authors give a higher survival rate. If there is a localized distal lesion, radical resection is performed and the result of chemotherapy treatment is more than 90% tumor necrosis, then 5-year survival is observed in 80% of cases.
The prognosis is worse in case of proximal localization, large tumor size, poor response to chemotherapy before surgery and metastases. Poor prognosis for tumors in the pelvic bones and weight loss at diagnosis. It is known that the intensity of tumor cell apoptosis also affects prognosis. Also unfavorable factors are early relapse, multiple lesions in the lungs and pleural involvement. If patients have stage 4, how long do they live in this case? When removing metastases in the lungs, 12-20% occur; if metastasectomy is not performed, 2.5% of patients survive. Life spans are calculated in months.
List of sources
- Clinical guidelines for bone sarcomas, 2022, 51 p.
- Practical recommendations for the treatment of primary malignant bone tumors (osteosarcoma, Ewing's sarcoma) / Malignant tumors. Russian Society of Clinical Oncology. 2022, pp. 283-295.
- Clinical guidelines for the diagnosis and treatment of patients with primary malignant bone tumors. 2014, 25 p.
- Clinical protocol for diagnosis and treatment. Bone sarcoma, 2015, 19 p.
- Belokon O.V., Nechval V.N. Surgical treatment of children with osteogenic sarcoma with metastases to the lungs/Health of Ukraine, 2012, pp. 34-35.
How is osteosarcoma treated?
Treatment of osteosarcoma consists of three stages.
They begin with a course of preoperative, or neoadjuvant, chemotherapy. On average it lasts 10 weeks. A combination of several drugs is prescribed - this helps to enhance the effect. The goals of neoadjuvant chemotherapy are to reduce the size of osteosarcoma and destroy metastases. Thanks to preoperative chemotherapy and modern chemotherapy drugs, survival for osteosarcoma has improved significantly in recent years.
This is followed by surgical treatment. In the past, the only option was to amputate the affected arm or leg. Modern surgeons can most often get away with removing part of a bone or joint. They can be replaced with a special prosthesis and almost completely restore the function of the limb. Surgeries for osteosarcoma have become more gentle.
A postoperative course of chemotherapy (adjuvant) is needed to remove cancer cells that may have remained in the body after surgery. On average it lasts 18 weeks, sometimes longer. How to treat relapse of osteogenic sarcoma? In general, the treatment regimen is approximately the same - surgery, a course of chemotherapy. After a relapse, the prognosis is much worse, but there is still a chance of recovery.