In surgical dentistry, one of the most common pathologies is osteomyelitis of the jaw - a purulent-necrotic pathological process that affects the bone tissue of the upper or lower jaw. This is a serious disease that, without timely treatment, can lead to serious consequences. Young men under 40 years of age are at risk.
Why this disease develops, how to recognize it in time and what the treatment is - we will look in more detail in our article.
Osteomyelitis of bone: what is it?
Bone osteomyelitis in the concept of general surgery is an inflammation of bone tissue, which has a rather complex pathogenesis. In modern medicine there are many theories of its origin. However, it is impossible to determine the most reliable one, since each of the theories does not exclude the others, but complements them. Thus, osteomyelitis is a multifactorial disease, in the development of which not only the penetration of any infectious agent into the bone tissue plays a major role, but also the state of the human body’s immune system, local circulation disorders with deterioration of trophism.
When an infectious agent enters bone tissue, a violent reaction of the body develops, manifested by purulent inflammation. To destroy the infection, leukocytes begin to actively migrate to the site of the lesion, which produce a huge amount of enzymes. They gradually destroy bone structures and form cavities filled with liquid pus, in which pieces of bone or sequestra can be found. Sometimes the inflammation spreads to the surrounding soft tissue, which leads to the formation of fistula tracts that open on the skin.
If the immune system of a sick person is active enough, then inflammation can be limited on its own and become chronic. But if there is an immunodeficiency in the body, then the infection spreads further with the development of severe purulent complications, such as sepsis, which often leads to disability or even death.
General information about the disease
With osteomyelitis, destructive changes in the bone tissues of the oral cavity are observed. It is this diagnosis that most often forces dental surgeons to pick up a scalpel. In terms of prevalence, it can be compared with periodontitis and periostitis.
If the disease is not treated, the bone tissue will bend, become thinner, and become incredibly fragile. Painful fistulas will begin to form. A person will still not be able to tolerate such symptoms for a long time, so there is no need to lead to complications.
Osteomyelitis in dentistry
Osteomyelitis of the jaw bones accounts for approximately a third of all identified cases of this disease. This statistical feature is not accidental and is determined by the presence of teeth, which are often a source of infection of bone tissue. In addition, there are a number of features in the jaw that predispose to the development of such a disease:
- a very abundant network of arterial and venous vessels in the maxillofacial region;
- active growth of the jaw and rapid changes in its structure during the period of replacement of milk teeth with permanent ones;
- the presence of relatively wide Haversian canals;
- very thin and delicate bone trabeculae;
- high sensitivity of myeloid bone marrow to infection.
All this leads to the fact that the penetration of almost any microorganism deep into the bone tissue provokes the development of osteomyelitis.
What is it and how to treat it?
Osteomyelitis is an inflammation of the bone marrow with a tendency to progress.
This is what distinguishes it from the widespread dentoalveolar abscess, dry socket, and osteitis seen in infected fractures. Osteomyelitis affects adjacent cortical plates and often periosteal tissues. In the era of preantibiotics, osteomyelitis of the mandible was not uncommon. With the advent of antibiotics, the disease began to be detected less frequently. But in recent years, antimicrobial drugs have become less effective, and the disease has reappeared.
Causes
The main reason for the development of osteomyelitis of the jaw is the penetration of highly pathogenic microorganisms into the bone tissue. Infection can occur in several ways:
- Odontogenic way, when the source of the infectious agent is a tooth affected by caries. In this case, microorganisms first enter the pulp tissue, after which they spread through small lymphatic vessels or dental tubules to the bone tissue.
- Hematogenously, when pathogenic microorganisms spread to the maxillofacial area through blood vessels from the primary source of infection. This role can be played by any infectious focus present in the body: acute or chronic tonsillitis, erysipelas or furunculosis. In addition, some specific infections can provoke osteomyelitis: typhus, scarlet fever or even the common flu.
- Traumatically, when osteomyelitis occurs against the background of infection after a fracture or surgery on the jaw. It is most rarely seen in dentistry.
With the odontogenic route, the lower jaw is most often affected, and with the hematogenous route, the upper jaw is most often affected. If the infection occurs hematogenously, then the localization of the purulent focus will be deep in the bone tissue, and the phenomenon of periostitis will be minimal.
Classification of pathology
Depending on the method of infection, the following types are distinguished:
- Hematogenous - bacteria spread through the circulatory system from other infectious foci. This path is typical for secondary osteomyelitis of the upper jaw, which develops against the background of another disease. This could be scarlet fever, purulent otitis media, tonsillitis, or diseases of the larynx. First, the infection affects the bone tissue of the jaw, and then only the teeth and gums.
- Odontogenic – external route of infection. The cause is an infected pulp or tooth root. Predisposing factors include advanced dental diseases. These are pulpitis, periodontitis, the presence of cystic formations, alveolitis.
- Traumatic – fractures and injuries of the jaw joint with damage to soft tissues and the presence of fragments of the dentition. Often occurs due to late seeking medical help.
According to the course and nature of the manifestation of symptoms, the pathology can be acute, subacute and chronic. Based on the area of distribution, local (limited) and diffuse (diffuse) forms are distinguished.
Symptoms
The clinical picture of osteomyelitis depends on whether the disease occurs in acute or chronic form.
Spicy
Typically, the symptoms of this pathology occur suddenly and manifest as local and general manifestations.
General symptoms are nonspecific and reflect only the presence of a severe inflammatory focus in the body:
- A significant increase in body temperature to 39 degrees and above.
- General severe weakness, malaise, headaches and aches in the joints.
- Paleness of the skin and mucous membranes, increased sweating.
Against the background of such general manifestations, local signs of the disease also arise:
- Constant unbearable pain in the area of the tooth that has become a source of infection. As the inflammatory process spreads, the pain syndrome intensifies, loses its clear localization and sometimes spreads to the entire jaw or half of the skull, radiating to the ear area or eye.
- Often inflammation seizes the jaw joint, and arthritis develops, which leads to the fact that a person cannot close his jaw and keeps his mouth open all the time.
- The tooth that caused the disease begins to loosen. With diffuse inflammation, neighboring teeth may also become loose.
- The mucous membrane of the gums and oral cavity becomes sharply swollen, hyperemic and painful.
- Increasing swelling of soft tissues leads to facial asymmetry and spasm of the masticatory muscles.
- Significant increase in the size of regional lymph nodes.
Hematogenous osteomyelitis usually has the most severe course, since it is characterized by a combination with damage to other skull bones and internal organs, which significantly worsens the further prognosis.
A feature of the course of the traumatic variant of the disease is that the clinical picture in the early stages can be erased due to manifestations of injury. However, when, 3-5 days after a jaw fracture, complaints of increased pain appear, and the patient’s condition worsens, body temperature rises, severe swelling of the oral mucosa and purulent discharge from the wound occurs, then the diagnosis becomes clear.
Chronic
As the disease becomes chronic, the patient's condition improves. However, over a fairly long period of time, such people experience severe pallor of the skin, lethargy, sleep disturbances and lack of appetite.
During examination for chronic osteomyelitis, fistulas are revealed that open both on the surface of the face and in the oral cavity. A small amount of purulent contents is released from the fistula tracts. You can also identify swelling of the mucous membranes, pathological mobility of one or more teeth, and enlargement of regional lymph nodes.
During the remission stage, pain may be absent or insignificant. But during an exacerbation, the pain syndrome may intensify, and the patient cannot always indicate the exact location of the pain.
Acute odontogenic osteomyelitis
The development of an infectious lesion of the jaw most often occurs in an acute form. The clinical picture of acute osteomyelitis of the jaw is pronounced, so treatment, as a rule, begins in a timely manner.
There are three types of acute stages of osteomyelitis of the jaw.
- Toxic. The patient's body experiences severe intoxication due to the activity of the infection. Symptoms occur suddenly without any warning signs of the disease. the course of the disease is severe.
- Septicopyemic. Signs of osteomyelitis are pronounced, but the patient's condition is stable. If left untreated, symptoms expand and become more intense.
- Local. A mild form of inflammation in which tissues are affected locally (usually in the area of the tooth socket).
If acute odontogenic osteomyelitis of the jaw is not treated, a purulent process, abscesses and other complications may develop.
Diagnostics
Based on the patient’s complaints and objective data from a general examination, the doctor may suspect osteomyelitis of the jaw bone. Confirmation of such a disease and a full formulation of the diagnosis are possible only after radiological diagnostics (x-ray diagnostics).
There are early and late radiological signs that indicate the presence of such severe pathology.
Early X-ray signs include:
- the presence in the images of areas of rarefaction of bone tissue, which alternate with its compaction;
- blurriness and extreme indistinctness of the bone pattern in the jaw;
- a slight increase in the thickness of the periosteum as a consequence of periostitis.
Late signs of osteomyelitis on a radiograph are:
- the formation of foci of destruction with the formation of sequesters by 7-12 days from the onset of the disease;
- thickening and moderate compaction of bone tissue around the inflamed lesion.
In difficult cases, patients are advised to undergo MRI, which allows them to more clearly see the extent of bone tissue damage, as well as visualize small purulent foci.
In addition to the X-ray examination, general clinical tests are carried out, which reflect the activity of the inflammatory process:
- a general blood test, which can reveal an increase in the number of leukocytes, changes in the leukocyte formula of an inflammatory nature, a decrease in the number of red blood cells and hemoglobin;
- biochemical blood test to identify electrolyte disturbances and the appearance of inflammatory markers.
In order to determine the causative agent of osteomyelitis and identify its sensitivity to antibacterial drugs, a bacteriological study of the discharge of the fistula tracts is carried out with the inoculation of pus on special nutrient media, followed by microscopy of the obtained samples.
Chronic osteomyelitis in children
Most often it is a consequence of the acute form of this pathology and is secondary in nature. It often occurs against a background of weakened immunity, sensitization of the body by foci of chronic infection, or as a result of incorrect diagnosis and therapy. But in childhood, there are also primary chronic forms of the disease that have an atypical clinical picture.
Secondary chronic
Unlike adults, in childhood the chronicity of inflammatory phenomena occurs quite quickly. After 2-3 weeks, acute symptoms subside, but recovery does not occur.
The basis of the chronic inflammatory process is the active process of destruction of bone substance with the melting of all its elements and the formation of large areas of necrosis. At the same time, the bone tissue restoration system is activated due to intraosseous structures and periosteum. One of the most important features of secondary chronic osteomyelitis in children is the presence of permanent tooth buds, which, when involved in pathological processes, can die and behave like sequestra.
Symptoms
As inflammation becomes chronic, all its acute manifestations subside. Approximately 7-10 days after the onset of the disease, the child’s condition improves significantly: fever and symptoms of intoxication go away, sleep and appetite normalize. All that remains is increased fatigue, sweating, weakness, and pale skin. In some cases, children report slight pain in the jaw on the affected side.
But upon examination, local manifestations of inflammation remain:
- soft tissue infiltrates over the focus of osteomyelitis;
- pain on palpation of the jaw;
- single or multiple fistulas with purulent discharge;
- enlarged and painful lymph nodes in the jaw and neck;
- poor healing of the extracted tooth socket, from which pus often comes out;
- pathological loosening of teeth.
In the acute stage, general and local symptoms of the disease are similar to those of acute osteomyelitis.
Diagnostics
To confirm, an x-ray of the maxillofacial area is performed. In this case, the images will visualize foci of bone tissue destruction, sequestration and dead rudiments of permanent teeth, which alternate with areas of bone compaction. Against the background of extensive damage, it is possible to identify pathological fractures of the jaw.
Blood tests in the remission stage may show a moderate increase in the number of leukocytes (leukocytosis), an increase in the ESR value.
Treatment
In the treatment of secondary chronic osteomyelitis of the jaw, conservative methods come first:
- Antibiotic therapy. Which antibiotics to take will be decided only after performing cultures of purulent discharge from fistulas to determine the type of pathological microorganism and its sensitivity to antibacterial agents.
- Desensitizing therapy, which includes the use of antihistamines to eliminate allergenicity in the body and increase its resistance.
- General strengthening and immunostimulating therapy.
- Physiotherapy: laser irradiation, UHF therapy.
It is advisable to carry out no earlier than 2-3 months after its start. Indications for osteotomy and sequestrectomy are:
- the presence of large sequesters that do not undergo spontaneous lysis over a long period of time;
- dead rudiments of permanent teeth that support inflammatory phenomena;
- the emergence of a threat of amyloidosis of internal organs.
During an exacerbation, treatment tactics will not differ from those for acute osteomyelitis. In this case, the main method of treatment will be surgical intervention with the opening of purulent foci and their drainage.
Primary chronic
It is quite rare. It is caused by weakly active microorganisms penetrating from carious teeth, which for a long time can support the processes of inflammation of bone tissue.
As a rule, this variant of osteomyelitis is productive in nature, i.e. processes of destruction in bone tissue are weakly expressed, but active formation of new bone occurs.
Clinically, it occurs without an acute period. The general condition of the child is not disturbed. Only nonspecific symptoms are noted: weakness, pallor, increased fatigue. Local manifestations include an increase in the thickness of the jaw bones, slight pain in the area of the causative tooth, and signs of lymphadenitis in the regional lymph nodes. There are no fistulas on the mucous membranes or skin.
On radiographs there are no foci of destruction and sequestration. The active formation of new bone tissue comes to the fore, as a result of which the jaw increases in size, and its structure resembles a marble pattern.
The productive form of osteomyelitis in the initial stages responds well to conservative treatment. With a properly selected course of antibacterial, anti-inflammatory and desensitizing agents, cure occurs quickly enough without negative consequences. In advanced cases, surgical treatment is indicated, the main purpose of which is to remove excess bone tissue and dead tooth germs, modeling the normal contour of the jaw.
Differential diagnosis
Differential diagnosis of osteomyelitis with other diseases that have similar symptoms is important, since an incorrect diagnosis can lead to an incorrect choice of treatment tactics and ineffective therapy. All this increases the risk of an unfavorable outcome of the disease and a poor prognosis for future health.
The differential diagnosis of osteomyelitis should include such diseases as:
- acute form of periodontitis,
- acute pulpitis,
- periostitis,
- suppuration of a tooth cyst,
- acute sinusitis of odontogenic origin,
- abscess of soft tissues in the maxillofacial area (MFA).
Complications
An incorrect diagnosis or untimely initiation of therapy for osteomyelitis leads to the development of severe complications, which have a high mortality rate and often cause disability.
The most common complications of osteomyelitis of the jaw are:
- Abscesses of soft tissues, perimaxillary phlegmons and purulent leaks, which tend to quickly spread to the cervical region and the mediastinum. This pathology is extremely dangerous, since the sepsis associated with it (in non-medical vocabulary the term “blood poisoning” is used) quickly leads to damage to vital organs with the development of septic shock and death.
- Thrombophlebitis of the facial veins, mediastinitis, pericarditis or severe pneumonia.
- Purulent damage to the membranes of the brain with the development of meningitis.
- If the purulent focus is localized in the upper jaw, the infection may spread to the orbital region with damage to the eyeball, atrophy of the optic nerve, which leads to irreversible loss of vision.
Treatment
Treatment of osteomyelitis of the jaw bones consists of simultaneously solving two important problems:
- The fastest elimination of the focus of purulent inflammation in the bones and surrounding soft tissues.
- Correction of functional disorders that were provoked by the presence of a severe infectious process.
All patients, without exception, are subject to hospitalization in a surgical department specializing in maxillofacial surgery. If there is no such hospital, then treatment is carried out in a department with experience in dental surgery.
The complex of treatment measures includes:
- Surgical intervention with opening of the purulent focus, cleaning it of necrotic masses and complete drainage.
- The use of antibacterial drugs with a wide spectrum of activity.
- Detoxification and anti-inflammatory treatment, strengthening the immune system.
General care is also important, with strict bed rest, nutritious but gentle nutrition (hypoallergenic diet including all necessary nutrients, vitamins and minerals).
How to get rid of osteomyelitis of the lower jaw
This is achieved by a combination of:
- radical surgical treatment;
- drug therapy;
- physical methods.
With the odontogenic type of osteomyelitis, they begin with the removal of the affected tooth, with the retrograde type - with sanitation.
This is followed by:
- opening of foci of suppuration to ensure free outflow of exudate, followed by antiseptic treatment of the oral cavity;
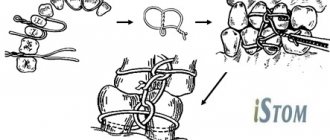
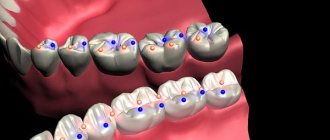
- splinting unaffected but loose teeth. This is done when there is a risk of jaw fracture;
- removal of areas of dead tissue, followed by the introduction of osteoplastic materials and antibiotics into the cavity.
Drug therapy includes the use of:
- broad-spectrum antibacterial drugs or those that are harmful to the pathogen identified during the diagnostic period;
- immunomodulatory medications;
- desensitizing and antihistamine drugs;
- general strengthening agents.
Physiotherapeutic methods are indicated at the final stage of treatment. On days 5-6 after surgery, the doctor may prescribe:
- magnetic therapy;
- interstitial electrophoresis;
- laser treatment.
Treatment is always complex. It is aimed at eliminating the causes of pathology, its consequences, and restoring health.
Consequences and rehabilitation after osteomyelitis of the jaw
The consequences of acute or chronic osteomyelitis of the jaw bone can be quite serious and significantly worsen a person’s quality of life.
- Often, during the surgical treatment of such a pathology, it becomes necessary to remove not only the causative tooth, but also several others. This leads to the fact that in the future the person will need orthodontic treatment and prosthetics.
- Extensive bone tissue defects can lead to jaw deformities, which is not only a cosmetic defect, but also significantly disrupts the normal functioning of the maxillofacial apparatus.
- Damage to soft tissues often leads to scar deformation, which is also a serious cosmetic problem that needs to be solved with plastic surgery.
- The spread of infection to the joint can provoke inflammation (arthritis) or arthrosis, which subsequently causes the development of ankylosis and a sharp limitation of jaw mobility.
- The consequences of septic conditions against the background of osteomyelitis may also include disruption of the functioning of internal organs, hematopoietic processes and the functioning of the immune system.
- Osteomyelitis affecting the upper jaw can spread to the zygomatic bone and even the orbit with the development of an abscess or phlegmon of the eyeball. This leads to complete loss of vision without the possibility of recovery.
Rehabilitation after suffering purulent inflammation of the oblique jaw sometimes continues for several years. All patients are subject to dispensary registration, from which they are removed only after correction of all violations that have arisen.
Rehabilitation measures include:
- use of physiotherapeutic techniques;
- if necessary, prosthetics for lost teeth;
- repeated surgery for cosmetic or medical reasons;
- prevention of recurrence of such pathology.
Preventive actions
Prevention is important not only to prevent the development of purulent inflammation, but also to minimize the likelihood of complications. With the help of preventive measures, you can also speed up rehabilitation if it was not possible to prevent the disease:
- Timely elimination of carious formations, even if there are no clinical symptoms.
- Sanitation of various foci of infection.
- Physical activity, a balanced and nutritious diet, which contribute to the effective functioning of the immune system.
- Compliance with the doctor’s recommendations after injury, during recovery after surgery or tooth extraction.
In conclusion, I would like to emphasize that although modern medicine has made great progress, osteomyelitis of the jaw bone still remains a serious problem. Thanks to the timely detection of symptoms of pathology and proper treatment, it is possible to significantly increase the likelihood that the patient will be able to fully recover and the quality of his future life will not be affected.
Prevention
Preventive measures are not only the key to preventing the development of osteomyelitis, but also a factor that reduces the risk of complications and shortens the recovery period if the disease cannot be avoided:
- Timely treatment of caries, even if it has no clinical manifestations.
- Maintaining normal immune status through regular physical activity, rational and nutritious nutrition.
- Sanitation of all chronic foci of infection in the body.
- In case of injury, in the postoperative period or after tooth extraction, compliance with all preventive medical prescriptions.
In conclusion, it should be noted that, despite all the achievements of modern medicine, osteomyelitis of the jaw in adults and children does not lose its relevance. Timely detection of its signs and adequate treatment increase the patient’s chances of a full recovery and maintaining a high quality of life.
»
Toothache after caries treatment
Constant pain after filling can occur for many reasons. A common cause of discomfort is the application of an insulating lining made of glass ionomer cement (GIC) and filling on the same day with a composite. The polymerization times of GIC and composite differ, which can result in displacement of the gasket and its pressure on the pulp.
If the pain is short-term in nature as a reaction to cold, sour or sweet and quickly passes after removing the irritant, it may be due to the fact that during the treatment there was a mechanical effect on the pulp. After 2-3 days, the pulp will return to normal functioning and the pain will stop.
If you experience pain when biting, you need your dentist to grind the filling to fit your bite.