Osteomyelitis of the jaw
In surgical dentistry, osteomyelitis of the jaw is considered a common disease. Osteomyelitis of the jaw (ICD 10 code M.86) - (osteomyelitis from the Greek osteon bone + myelos bone marrow) is a severe inflammation affecting soft tissue elements, bone tissue and periosteum. It is accompanied by necrotic damage (decomposition) of the bone, which subsequently leads to its deformation. The development of the pathological process is provoked by bacteriological microorganisms that penetrate the jaw bone together with infected blood or in response to post-traumatic damage - fractures and wounds.
Osteomyelitis of the jaw (ICD code M.86) is a serious pathogenic process that, without timely treatment, can lead to complications. The risk group consists of male patients under 40 years of age. The primary and main thing is to identify the symptoms of the disease, thanks to a clear differential diagnosis. Thus, dental surgeons from the West Dental family clinic network in Yanino-1 and Vsevolozhsk will help diagnose and treat the problem at a reasonable price.
The causes and symptoms of the disease, which specialist to contact and how to treat - we will consider below in the article.
Osteomyelitis in the dental field
Osteomyelitis of the jaw accounts for about 1/3 of the total number of cases of detection of this problem. This is due to the presence of elements of the dentition, which become a source of infection of bone tissue. In addition, the jaw has certain features that are ideal for the development of osteomyelitis:
- rapid growth of the jaw and significant changes in its structure during the transition from baby teeth to molars;
- increased propensity of myeloid bone marrow to become infected;
- a large number of vessels in the maxillofacial area;
- minimum thickness of bone trabeculae;
- Haversian canals are relatively wide.
For this reason, the penetration of various microorganisms into bone tissue very often leads to osteomyelitis.
Causes
The main provocateur of the formation of osteomyelitis in the upper and lower jaw is considered to be pathogenic microflora - streptococci and anaerobes, present in the oral cavity of every person. They aggravate the infection, affecting the soft and hard components of the mouth. There are several ways to penetrate deeper into the pathological process:
- Missed dental caries, which destroyed the enamel with dentin and penetrated into the pulp chamber.
- Traumatization – crack, violation of the sealing material. The damage must be deep (fracture of the HF or LF) to provoke an infectious process (staphylococci).
- Chronic infection occurs in other parts of the body. Pathological microorganisms can reach the jaw through the lymph nodes or blood vessels (ENT organs).
In most patients, osteomyelitis is located on the lower jaw, since the lower units are more likely to be affected by caries or trauma. Also, people with immunodeficiency and blood diseases are at risk, because they have difficulty healing wound surfaces and the immune function of the body is weakened.
Other factors:
- smoking;
- alcohol;
- Diabetes type I and II;
- eating disorders;
- syphilitic infection;
- radiation and chemotherapy.
If you miss and do not treat acute osteomyelitis in the upper or lower jaw, then the process becomes chronic, which is more difficult to treat and leads to many complications.
Symptoms
Acute osteomyelitis appears very suddenly. If children are small, then they are noted to be moody and lethargic. They don’t want to eat, they don’t sleep well, and their temperature rises. If the child is older, then he may feel unwell, general weakness, and may complain of toothache.
When the disease is still in its early stages, the following manifestations may be present:
- bone pain. Initially it has a local character, and then diffused;
- the oral mucosa swells, hyperemia is noted;
- on the side that is affected, the soft tissues become swollen;
- the face becomes asymmetrical;
- chewing muscles may spasm.
If an injury occurs, signs of the disease appear after 3-5 days. The child feels much worse, the temperature rises, and pus may also be released if the mucous membrane has been damaged.
Classification
According to the method of penetration of osteomyelitis infection on both jaws, a classification has been compiled:
- Hematogenous - pathogenic microorganisms move through the blood from other foci of infection. This feature is characteristic of secondary pathology of the upper oral part, which develops against the background of another disease (scarlet fever, diseases of the ENT organs). The bone elements of the oral apparatus are primarily affected, followed by the gingival tissue.
- Odontogenic – infection comes from a tooth, damaged pulp or root (pulpitis, periodontitis, cyst, alveolitis).
- Traumatic – advanced fractures and injuries of the maxillofacial area.
According to the symptoms, the process happens:
- spicy;
- subacute;
- chronic.
By distribution:
- local (with clear boundaries);
- vague (diffuse).
Consequences of the disease and methods of recovery
Suffered purulent inflammation of the jaw in acute or chronic form often has serious consequences that negatively affect the quality of life.
- Often, surgical intervention during the treatment of a disease is accompanied by the removal of one or more elements of the dentition. As a result, the patient has to subsequently contact an orthodontist and undergo prosthetics.
- In many cases, infection of soft tissues causes scar deformation. This complex cosmetic problem can be corrected using plastic surgery methods.
- Septic conditions, which can develop against the background of the underlying pathology, can disrupt the full functioning of internal organs and negatively affect the functioning of the immune system and hematopoiesis.
- Severe bone lesions can change the natural shape of the jaw. This is not only a cosmetic problem, but also negatively affects the efficiency of the maxillofacial apparatus.
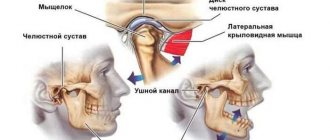
- Infection of a joint can lead to arthritis or arthrosis. This often leads to the formation of ankylosis and significant impairment of jaw mobility.
- Damage to the pathology of the upper jaw can affect the zygomatic bone and orbit with the further appearance of phlegmon or an abscess of the eyeball. Ultimately, the patient loses vision and it is no longer possible to restore it.
In some cases, the recovery period after osteomyelitis of the jaw is several years. All patients are monitored at the dispensary until all emerging violations are eliminated.
Rehabilitation involves the following procedures:
- application of physiotherapy methods;
- performing surgery for medical or cosmetic reasons;
- prosthetics of removed elements of the dentition (if necessary);
- preventive measures to avoid recurrence of the problem.
Osteomyelitis of the upper and lower jaw: symptoms
The course of the disease process is slow, and the first sign is pain in the area of the affected unit.
Then joins:
- spread of pain to nearby segments;
- swelling and redness of the gum tissue;
- periodontal damage, which causes mobility of units;
- pain in the temporal region;
- numbness of the chin;
- difficulty eating;
- speech defects;
- unpleasant odor from the mouth;
- increase in l/u;
- swelling in the problem area.
Acute osteomyelitis on the lower jaw (ICD M.86) develops very rapidly in conjunction with an increase in temperature and chills. In the absence of outflow of pus, abscesses and phlegmons form, which requires immediate surgery. This pathology in a child may be confused with mumps (mumps).
With osteomyelitis on the lower jaw (ICD-10 code M.86), in addition to damage to the alveolar part and body, the inflammatory process can spread to its branch and processes. One important feature is complications from the soft tissue elements around the NP - many muscles and tissue spaces.
After the acute period (1-2 weeks), the subacute period begins, after the formation of a fistula for the discharge of pus. The condition improves, pain decreases, and the mobility of units increases—gastrointestinal diseases develop. The subacute form becomes chronic, which lasts several months. As a result, in adults the clinical history ends with the removal of necrotic tissue, with a favorable outcome.
Features of symptoms
The main noticeable symptom is called pain, but in fact it is far from the first, it’s just that the symptoms of the disease are not obvious at the initial stage. In addition, pain also occurs with all other diseases of the spine, so even with the onset of pain, the infection goes unnoticed for a long time, for months. Patients begin to worry when general intoxication, a feeling of chills, a rise in temperature, increased sweating and weight loss are added to the pain, and the pain begins to manifest itself especially strongly at night.
The most obvious symptom of osteomyelitis is pain against the background of general intoxication and poor health
In accordance with the infecting ability of pathogens, three types of osteomyelitis developing in vertebral structures are distinguished.
- Spicy.
- Primary chronicle.
- Chronic.
Table. Symptoms of osteomyelitis by type.
| ● multi-stage sharp pain, increasing in amplitude at night; | ● mild episodic pain syndromes; | ● mild pain of unclear localization; |
| ● excessive sweating; | ● chills; | ● rises to 37°C, usually in the evening; |
| ● strong rise in temperature to 39°C and above; | ● mild intoxication; | ● pain may intensify at night; |
| ● convulsive conditions; | ● slight temporary increase in temperature; | ● feeling of stiffness of the spine; |
| ● hypotension; | ● increased sweating; | ● sweating; |
| ● swelling of soft paravertebral tissues. | ● general state of lethargy; | ● slight swelling and numbness of the spine. |
| ● vascular tension; | ||
| ● pain in the back muscles. |
By the way. Almost always, patients mistake the primary chronic and stable chronic form for manifestations of osteochondrosis or other vertebral and joint pathologies, or diseases of internal organs such as the lungs and heart.
During its development, osteomyelitis inflames not only the bone tissue, but also spreads to the entire blood supply system in the spine. This can lead to sepsis, disability and death.
Occasionally, the infection involves nerve structures in the inflammatory process by moving into the spinal canal, causing the formation of an epidural abscess. It puts pressure on the nerves, and if the source of infection is located in the neck or chest area, it can result in paraplegia (paralysis of either lower or upper limbs in pairs) and quadriplegia (simultaneous paralysis of all limbs).
By the way. Victims of osteomyelitis most often become older men, especially those who experience frequent stress and excessive tension and have a large number of different diseases. This reduces immunity and makes it impossible to cope with bacteria that cause inflammation.
Victims of osteomyelitis are most often older men
When the disease takes a protracted chronic form, the number of purulent foci in the bone increases and their size also increases. New inflamed tissue may begin to grow, which comes into conflict with healthy tissue and infects it, expanding the area of infection. The bone marrow does not remain aloof from the inflammatory process, since the accumulating pus interferes with the normal functioning of the blood cells that provide it with nutrition.
Diagnostics
If you experience pain in the tooth area of unknown etiology, or changes in the gums, contact your dentist (he has a Leica M320 operating microscope in his arsenal), who will then refer you to a surgeon or orthopedist as necessary. At the initial stage of pathology, the doctor chooses to collect complaints and study them, visual and instrumental examination. The degree of mobility of the units and their pain, the state of the oral mucosa is determined.
It is important to distinguish the acute period of the disease from periostitis, cysts and periodontitis, so the experience of a specialist is very important.
This is a purulent infectious process, which means that general blood and urine tests will be of research significance. To type the pathogen, a tank is performed. sowing of pus.
In the chronic stage, bone changes are already noticeable, so X-rays (CT) are necessary, for which West Dental has a panoramic CBCT Pax-i3D. The image shows sequestration and the depth of the process.
Diagnostic procedures
Due to hidden symptoms, it can be difficult to diagnose vertebral osteomyelitis, especially in its early stages. Therefore, in case of any back pain, especially those of unclear etiology, you must immediately consult a doctor for instrumental examinations and laboratory diagnostics. In some cases, in order to carry out a bacteriological analysis and identify the type of bacterial culture - the causative agent, a puncture is required.
Spine biopsy
The beginning of the diagnostic process usually begins with the appointment of x-rays, which, by the way, may not show anything for up to four weeks after the onset of the inflammatory process.
Spinal osteomyelitis on x-ray
By the way. In order for a change in bone tissue to be visualized, it must be destroyed to at least 30%. However, X-rays show long before this a decrease in the intervertebral distance and destruction of the end plates if intervertebral structures are involved in the process.
MRI with contrast is more informative than x-rays. Since infection destabilizes blood flow, making it unstable and increasing in certain areas, contrast can show these areas by accumulating there.
Magnetic resonance imaging
Laboratory tests are blood cultures, which can be used to identify the causative agent of infection in order to select the necessary antibiotic therapy. But culture, unfortunately, reveals the pathogen in only 50% of episodes.
There are also inflammatory markers that make it possible to predict an existing infection with some accuracy. In particular, this is an indicator of the erythrocyte sedimentation rate, which is exceeded in 90% of cases of osteomyelitis. Decoding the leukocyte blood count is considered the most valuable and informative laboratory diagnostic method.
Leukocyte blood formula. Decoding
If the infectious process is confirmed, but the pathogen cannot be detected, a tissue biopsy is performed to prescribe the correct treatment. It is carried out with a needle under the control of a computed tomograph. If indicated, an open biopsy can be performed.
Complications
If you see a doctor in time, make a diagnosis and choose the right treatment, the prognosis will be favorable.
If you ignore all the conditions, complications will arise:
- Meningitis
- Abscess of the brain and lung.
- Orbital phlegmon.
- Sinusitis.
- Vein thrombophlebitis.
- Sepsis.
- Mediastinitis.
Pathological data require immediate assistance to prevent death.
The chronic process, with its long course, affects the soft tissue and bone areas of the maxillofacial area, and is accompanied by:
- traumatization;
- changes in the TMJ;
- the formation of adhesions in the joints and scars on the masticatory muscles;
Such disorders limit chewing movements or lead to immobility.
Secondary chronic
In children, rapid chronic inflammation is noted. After 3 weeks, acute symptoms disappear, but the child does not become healthier.
When it comes to chronic inflammation, there is an active process of destruction, as well as melting of the elements of bone substance. After which areas of necrosis form. In addition, thanks to the intraosseous structures and periosteum, bone tissue is actively restored. The peculiarity of this type of osteomyelitis is the presence of the rudiments of permanent teeth. If they are involved in pathology, they may then die, and their behavior will resemble sequestration.
Symptoms of chronic osteomyelitis
When the inflammatory process becomes chronic, acute symptoms decrease. 10 days after the disease began, the child feels better (appetite and sleep return to normal, fever and symptoms of intoxication disappear). But children still feel weak, they get tired quickly, they sweat profusely, and their skin is pale. Sometimes children say that their jaw hurts slightly on the side that is affected.
During the examination of such a patient, you can notice certain manifestations of the inflammatory process:
- over the place where the focus of osteomyelitis was, there are soft tissue infiltrates;
- pain is felt when the child's jaw is probed;
- There are fistulas in which pus is released. They can be multiple or single;
- lymph nodes in the neck and jaw increase in size and hurt;
- The sockets of the tooth that were removed do not heal well. It may also leak pus;
- teeth are very loose.
When the disease worsens, the symptoms resemble acute osteomyelitis.
Diagnosis of chronic osteomyelitis
An x-ray should be taken to confirm the diagnosis. It will allow you to see the foci of destruction, those rudiments of teeth that have died, sequestration. If the lesion is extensive, then jaw fractures may even be detected.
Treatment of chronic osteomyelitis
When it comes to secondary osteomyelitis of a chronic form, a conservative treatment method is used:
- antibiotic therapy. Which drugs are suitable? All this is determined after the patient undergoes a culture of the pus discharged from the fistulas. Thus, the type of microorganism that provoked the pathology and its sensitivity to different drugs will be determined;
- desensitizing therapy. This includes antihistamines, which will remove the allergic reaction and also increase the body's resistance;
- therapy that can be used to stimulate the immune system and strengthen the body as a whole;
- physiotherapy. For this purpose, UHF therapy and laser irradiation are performed.
To perform an osteotomy or sequestrectomy, you must have the following indications:
- sequesters that are large in size and do not undergo spontaneous lysis for a long time;
- there are rudiments of permanent teeth that have died. They support inflammation;
- there was a risk of amyloidosis of internal organs.
If the disease worsens, the treatment will be identical to that in the case of acute osteomyelitis. But the main method is surgical intervention, during which lesions with pus are opened and drainage is performed.
Treatment
The effectiveness of therapy depends on the initial causes of the formation of the inflammatory process. Therefore, in osteomyelitis of the jaw, comprehensive treatment is important, not only by a dentist, but it is recommended to go for a consultation with doctors of medical specialties.
- Sanitation of the oral cavity with antiseptic solutions. Further spread of infection to surrounding structures is prevented. Also, necrotic soft tissue formations are eliminated.
- Anti-inflammatory drugs. Minimize intoxication of the body.
- Immobilize the fracture, and if there is a tooth in it, then remove it.
- Taking antibiotics, regardless of provoking factors.
- Intraosseous lavage may be necessary and will provide positive results. Minimizes the occurrence of complications and quickly prevents the growth of a harmful process.
- In case of a fistula, sequestrectomy is performed - necrotic areas of bone tissue are eliminated under anesthesia, taking into account the extent of the damage.
- If the teeth are mobile, they are splinted.
- After eliminating symptoms and carrying out all interventions, physical therapy, vitamins and immunomodulators are recommended.
Prevention of such pathology consists only of timely and regular visits to the dentist’s office and treatment of pathological processes in the oral cavity. Do not treat yourself at home, so as not to make it worse. Also, it is necessary to strengthen the body’s immune system, avoid injuries and not let the pathological process become chronic.
Vertebral infection
Not so long ago, this disease was considered incurable, since it was impossible to remove the infection from the skeletal system. Today, the process is successfully stopped through an operation during which infected tissue is removed, associated with intensive antibacterial drug action.
Spinal osteomyelitis is treated surgically
By the way. Osteomyelitis often occurs in children, affecting the bones in the legs and arms. Adults mainly suffer from an inflammatory process localized in the bones of the spine. In some cases, if an adult patient has diabetes, the process begins to develop from the lower extremities, if there are trophic ulcers on them.
Infection of the vertebrae cannot be considered a common cause of back pain, especially if the patient is young and, in principle, healthy. But cases of the disease are becoming more frequent, and osteomyelitis (the second name is spondylitis) is gradually becoming an urgent problem.
By the way. The most common route of infection into the vertebral segments is hematogenous, which is carried out through the bloodstream. In some episodes of infection, microbes appear in the vertebrae after various medical diagnostic procedures, such as urological cystoscopy.
Etiology of causes of osteomyelitis
To understand how bone tissue becomes infected, it is necessary to remember how the blood supply occurs in the spine.
Initially, the body of each vertebral segment is isolated from the rest by a cartilaginous intervertebral septum. But along the ridge there are arteries that branch from the neck and carry blood to all vertebral tissues, and, of course, through the vascular network, to the vertebrae. The lumbar zone receives nutrition with blood passing through the arterial canals of the lumbosacral zones. Each vertebra is entangled with venous vessels that connect to form veins.
Blood supply to the spinal cord
In this way, viruses can penetrate the vertebra through both veins and arteries. As soon as the pathogens find themselves in the bone tissue, the inflammatory stage is activated, during which it dies.
Accumulating obsolete microorganisms that are not removed in a timely manner form purulent accumulations in the spinal tissue. The outer vertebral membrane is destroyed, and the process spreads to other parts of the spinal column.
Who is at risk
Bone tissue is designed to be resistant to infection. Therefore, for osteomyelitis to begin, additional factors contributing to the development of the disease are necessary. These factors weaken bone tissue, increasing its vulnerability and reducing resistance to infection.
- Injuries accompanied by bone fractures, when infection can easily be introduced into the vertebra both by the bloodstream and by the tissue located next to the fracture.
- An operation to reposition bone fragments or a deep puncture was performed.
- Impaired blood circulation in the event that blood vessels are damaged or the blood flow is unstable. A deficiency of immune cells occurs, which reduces the ability to resist infection.
- Disease diabetes mellitus.
- Weakening and pathology of peripheral arteries, which may be associated with smoking.
- Infections.
- Deep carious dental lesions.
- Hereditary hemoglobinopathy expressed by sickle cell anemia.
- Placement of a dialysis or medical catheter.
- Intravenous drug use.
Causes of osteomyelitis
By the way. Despite the fact that catheters are absolutely necessary in various situations - dialysis, emptying the bladder, administering medications into veins for a long time - they carry perhaps the highest risk of unsterility and possible infection.
Greatest risk of infection during catheterization
Based on this, there are groups of patients who are most susceptible to osteomyelitis:
- elderly people;
- patients with drug addiction;
- people whose immune systems are weakened.
Drug-dependent individuals are most at risk of contracting osteomyelitis
Long-term use of corticosteroids for rheumatoid arthritis and other diseases, diabetes accompanied by insulin dependence, AIDS, people who have received organ transplants, suffer from malnutrition, and have cancer - all these patients have reduced immunity and an increased ability to resist infection at the bone-cellular level.