Osteosynthesis of the jaw is a method of surgical treatment of bone fractures using special, most often metal, structures. Osteosynthesis surgery is performed if the fracture site cannot be secured with splints, and also when it is difficult to fix bone fragments. There are different methods of performing the operation, they can be used depending on the type of injury and its severity.
Osteosynthesis allows you to maintain the required level of blood circulation in the damaged bone, which means that such a fracture will heal faster. Not only the integrity of the bone is restored, but also its structure, and this will take only a few weeks.
During the rehabilitation period, it is important to follow certain rules and monitor your well-being and the condition of your bone tissue. Violations of doctor's instructions can lead to pain and even loss of chewing functions.
Indications for osteosynthesis
Osteosynthesis may be prescribed in the following cases:
- if there are not enough stable molars at the fracture sites;
- upon impact, the fragments moved significantly;
- broken jaw bone behind teeth. With such an injury, individual parts of the bone tissue are displaced;
- the injury occurred as a result of the development of inflammatory diseases that thin the bone tissue;
- in case of a fracture of the lower jaw, if too small or massive fragments have formed;
- if the branches and body of the jaw are incorrectly positioned relative to each other;
- it is necessary to perform reconstructive surgery or osteoplasty.
Types of osteosynthesis
There are several methods of osteosynthesis; the doctor decides what type of operation the patient needs. Most often, surgeons combine several methods with each other to achieve better results.
Osteosynthesis of the jaw can be:
- Open. It is usually used for severe fractures. During the operation, soft tissue is cut and bone fragments are exposed. They are connected to each other and non-functional small fragments are removed, compressed soft tissues and fascia are released. However, with such an operation, there is still the possibility of tissue peeling off from the bone, then the callus at the fracture site will not be formed correctly. And this can affect the patient’s quality of life. In addition, stitches remain on the skin and paresis (decreased activity) of facial muscles is even possible. Depending on the type of fastening device, it is possible that the incision on the face will have to be made again to remove the fastener.
- Closed. The doctor combines bone fragments without cutting facial tissue;
- Focal. The fixing fastener is applied directly to the fracture site;
- Extrafocal. Fasteners are placed on top of the skin, above the fracture site.
Orthognathic surgery. Osteotomy of the upper and lower jaw. Genioplasty.
In the 21st century, modern orthodontics has enormous potential for solving the problems of malocclusion, which are associated with the incorrect location of the skeletal structure of the upper and lower jaws. Malocclusion can be either congenital or acquired as a result of injuries.
By the age of 16-20, such a jaw anomaly becomes more pronounced, which creates a certain discomfort, both psychological and aesthetic. People become unsure of themselves, and their self-esteem begins to decline. But this is not only a matter of aesthetics; such a pathology contributes to the development of a number of joint diseases, tooth loss, respiratory dysfunction, etc. All problems associated with eliminating such facial disharmony, returning normal occlusion (bite) and facial aesthetics can be solved by orthognathic surgery .
At the Federal State Budgetary Institution Scientific and Clinical Center of Otorhinolaryngology, Federal Medical and Biological Agency of Russia, orthognathic operations are performed by employees of the scientific and clinical department of maxillofacial surgery. Our Center employs some of the best specialists in Russia in the field of orthognathic surgery - Ph.D. Senyuk A.N., Lyashev I.N., Mokhirev M.A. Nazaryan D.N. , who apply not only the most modern world techniques, but also use their own developments.
“We often have to correct the mistakes of doctors who, with insufficient experience working with such patients, or in the pursuit of profit, corrected malocclusion, which ultimately led to severe complications and patient dissatisfaction with the final result of treatment,” says the head of the department of maxillofacial medicine. Facial and Reconstructive Surgery, Ph.D. Nazaryan D.N.
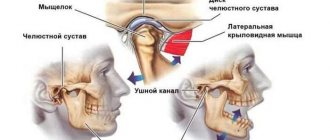
In their practice, our specialists carry out complex treatment, which includes orthopedic and orthodontic interventions, to achieve functional and aesthetic goals. Only an experienced specialist can determine that braces and orthodontic wires will not be able to relieve a patient with a skeletal jaw deformity from a protruding chin or a “ gummy smile ”, but on the contrary, they can lead to tooth dislocation and the development of the temporomandibular joint. We take a comprehensive approach to solving such problems, the essence of which lies in preliminary stage-by-stage preparation and preliminary 3D planning. Computed tomography, photography, plaster and STL models allow us to perform a complete preoperative analysis and simulated surgery. Orthognathic surgery allows you to move one or both of the patient's jaws back and forth, up and down. The treatment procedure takes place according to a pre-planned scheme, which involves moving the jaws, chin, soft tissues, eliminating dentoalveolar compensation, and aligning the dentition in relation to the main bone.
Orthognathic surgery is performed with maxillary osteotomy , where intraoral bone incisions are made above the teeth and below both eye sockets, allowing the upper jaw, including the palate and upper row of teeth, to be repositioned. This movement is positioned using a pre-made special splint, which will reliably guarantee its correct position of the lower jaw in relation to the soft tissues.
A mandibular osteotomy involves making bone cuts behind the molars, along the jaw, and downward so that the mandible can move as a single unit. As a result of this manipulation, the lower jaw, with the help of a titanium plate, smoothly moves to a new location.
The genioplasty operation is aimed at leveling the midline of the patient’s face, during which the chin part of the lower jaw is cut off and moved in the correct, harmonious direction.
All orthognathic operations are performed using intraoral access and do not have external incisions or scars. Such operations, in order to avoid relapses associated with continued jaw growth, can be performed on patients over 18 years of age, since it is believed that by this age the growth of a person’s jaws is completed. Orthognathic operations are performed under general anesthesia and, depending on the planning of the treatment requiring correction, can last from one to six hours.
In our Center, using specially made titanium plates, specialists fix all detachable parts of the jaw. After surgery, the following temporary symptoms are possible: postoperative swelling, bruising in the lips and cheeks, difficulty communicating in the first week after surgery, limited oral hygiene, numbness in the operated area, and a feeling of nasal congestion. In order to minimize risks and complications after surgery, the patient should follow the doctor's recommendations during the recovery period. After surgery, patients are recommended to eat semi-liquid food; there are no special dietary restrictions.
Thanks to Andrey Nikolaevich Senyuk in Russia, orthognathic surgery began to be carried out entirely using intraoral approaches, using preliminary preoperative planning in such a way that a precisely planned result in advance is achieved, coinciding with the final one both in terms of aesthetics and occlusion. It was he who organized the first international conference of orthofacial surgery in Russia.
Many years of experience in orthognathic surgery and deep knowledge of the problem will allow our highly qualified specialists to work wonders, as noted by the patients themselves), restoring self-confidence to patients and leading a fulfilling lifestyle. The surgical team of the department, headed by Doctor of Medical Sciences, Professor Karayan A.S., develops an individual treatment program for each patient, and attention and warmth from the treating staff are guaranteed to everyone!
Clinical cases
Example 1
| Diagnosis: combined deformation of the jaws, asymmetrical deformation horizontally. Planned: osteotomy of the jaws according to Le_Fort 1 and sagittal of the lower jaw. |
| On the 7th day: |
Other examples:
| BEFORE | AFTER |
The essence of osteosynthesis and what kind of procedure it is
With osteosynthesis, the doctor not only connects the fragments of the damaged jaw, but also securely fastens them with metal structures or glue.
Open focal osteosynthesis is carried out using:
- Bone suture. If the lower jaw or cheekbone is broken and the injury is recent, it can be fastened with a bone suture. For this, stainless steel, titanium wire or nylon thread is used.
During the operation, the doctor dissects the soft tissues of the face and fixes the fragments with wire. If the fragments are connected using a bone suture, the patient retains chewing function and can continue to care for the oral cavity. This method is contraindicated if the fracture site is inflamed or the patient has an infectious or purulent bone lesion.
- Installation of periosteal metal mini-plates. This method has proven itself in the treatment of all types of jaw bone fractures, except those in which a large number of fragments have formed. In this case, it is enough to make an incision only on one side. The doctor aligns the fracture sites, applies mini-plates to them and screws them on. Nowadays, mini-plates are most often fixed inside the oral cavity.
- Fixation with quick-hardening plastics. It is practiced only for fractures of the lower jaw. After exposing the bone fragments, the doctor makes a bone groove and places a special fixing compound in it. Excess plastic is removed with a cutter, after which the wound can be sutured.
- Osteoplast glue. This composition for fixing bone fragments is made of purified epoxy resin with an organic antiseptic - resorcinol. After application, the glue hardens in 8-12 minutes and reliably fixes the combined bone fragments. Nowadays this method is rarely used.
- Metal staples. For osteosynthesis, staples made of nickel-titanium alloy are used. At low temperatures, the alloy becomes plastic and is easy to shape into the desired shape. Then, at room temperature, the staple regains its previous shape. During the operation, it is first cooled, then inserted into the prepared holes on the bone fragments. As soon as the staples warm up, they straighten and securely fix the fracture site. Metal staples are especially convenient for fixing a fracture of the angle of the lower jaw.
Closed focal osteosynthesis is practiced for healing fracture sites where bone displacement has not occurred. Methods:
- Installation of Kirschner spokes. The doctor inserts metal needles into the bone fragments using a surgical drill. For reliable fixation, the needles are fixed into each fragment to a depth of up to 3 cm. There is no need to dissect soft tissues; the operation is performed through the mouth. This is a low-traumatic practice, but wearing needles creates a lot of inconvenience for the patient.
- Applying a surrounding suture. Applicable when the fracture gap is displaced forward or backward along the jaw. In this case, the suture passes through the central part of each bone fragment. If there are a lot of fragments, the operation takes a long time, but this is one of the most reliable methods of osteosynthesis. It allows the patient’s jaws to be restored even after very complex injuries.
Introduction
Injuries to the maxillofacial region continue to remain one of the pressing surgical problems, which is associated with an increase in the number of patients with fractures of the facial skull bones as a result of road accidents and domestic conflicts, the aggravation of this type of pathology, and the increase in multiple and combined injuries [1, 2]. According to specialized literature, the share of maxillofacial trauma in the structure of various injuries among the urban population is 3.2–8.0% [3]. Fractures of the lower jaw account for up to 85% of the total number of fractures of the facial skull [4–7]. The development and implementation of new methods for fixing bone fragments have significantly increased the effectiveness of surgical treatment in the category of patients under discussion; however, according to a number of authors, complications range from 5.2 to 38.4% of cases [8–11].
Many of the proposed methods are successfully used in everyday practice for performing osteosynthesis for facial skull fractures - titanium plates on the bone, bone suture with stainless steel or tantalum wire, Kirschner wires, a possible combination of bone suture and wires, fixing structures made of shape memory materials. The purpose of this article is to describe the clinical use of titanium nickelide (nitinol) shape memory brackets for mandibular angular fractures.
Clinical case
Patient T.
, 41 years old, was admitted to the clinic of maxillofacial surgery of the University Clinical Hospital (UCH) No. 2 of the First Moscow State Medical University named after. THEM. Sechenov with complaints of pain in the lower jaw on the right, aggravated by chewing and opening the mouth, swelling of the face on the right, and malocclusion.
From the anamnesis it was established that the injury was received as a result of a fight with an unknown person 8 hours before going to the hospital. The patient did not report any compression phenomena. He went to the trauma center, where an X-ray of the skull and intermaxillary fixation were performed using Tigerstedt dental splints. The patient was taken by an ambulance team to the clinic of Clinical Hospital No. 2 of the First Moscow State Medical University named after. THEM. Sechenov, was hospitalized on an emergency basis.
On admission: general condition is relatively satisfactory. Somatic status without features. Upon examination, pronounced swelling of the soft tissues in the parotid-masticatory, buccal and submandibular areas on the right was determined. It was difficult to gather the skin into a fold; local pain was noted on palpation. Regional lymph nodes are not enlarged. The symptom of direct and indirect load is positive in the area of the angle of the lower jaw on the right. Vincent's sign was positive on the right side. From the side of the oral cavity: opening is limited to 2 cm, there was a violation of the closure of teeth such as an open bite on the right. Ruptures in the mucous membrane of the alveolar part of the lower jaw in the area of 4.7–4.8 teeth, as well as the presence of hemorrhagic clots in the oral cavity, were visualized. Swallowing is free, moderately painful (Fig. 1, 2,
Rice. 1. Patient T.’s appearance during hospitalization.
Rice. 2. Orthopantomogram of patient T. during hospitalization. There is a violation of the integrity of the bone tissue in the area of the angle of the lower jaw on the right with the presence of tooth 4.8 in the fracture line. 3).
Rice. 3. X-ray of the skull of patient T. in a direct projection.
Based on complaints, anamnesis, clinical examination and x-ray examination, the diagnosis was made: “Fracture of the lower jaw in the area of the angle on the right with displacement of fragments.”
After additional examination and preoperative preparation, on the day of admission to the hospital, the patient underwent surgical intervention: osteosynthesis of the lower jaw in the area of the right angle using external access using titanium nickelide brackets.
The operation was performed as follows: with premedication under local anesthesia with Sol. Lidocaini 1% 20 ml, on the side of the fracture parallel to the edge of the lower jaw, retreating 2 cm in the area of the angle, a skin incision 4 cm long was made. The skin, subcutaneous fat, superficial fascia of the neck and m. Platisma. The masticatory muscle itself was cut off at the point of attachment to the angle of the lower jaw. The lower jaw in the area of the angle is skeletonized. After visualization of the fracture line, small bone fragments were removed, soft tissue interposition was eliminated, and blood clots were removed. Before performing osteosynthesis of the lower jaw, a loose bone fragment and tooth 4.8 were removed from the fracture line (Fig. 4),
Rice. 4. A removed bone fragment not connected to the periosteum, and tooth 4.8 from the fracture line. Reposition of bone fragments was performed. The bite was fixed in the patient’s usual position using rubber rods and osteosynthesis was performed using two Ω- and S-shaped titanium nickelide brackets under bite control (Fig. 5).
Rice. 5. Operation stage. Osteosynthesis of the lower jaw using Ω- and S-shaped titanium nickelide brackets.
The brackets were installed as follows: holes were formed bicortically on each fragment using a drill, then the legs of the bracket, pre-cooled to +1-3 °C, were bent to the sides (the bracket was activated) and inserted into the corresponding milling holes. When the bracket was heated to 35-36 °C, the original shape was restored - the legs of the bracket were brought closer together, which led to dosed compression of the bone fragments. The postoperative wound was treated with antiseptic solutions, and a latex graduate was installed. The wound was sutured in layers. Hemostasis was performed during the operation.
The postoperative period was uneventful. The patient was discharged for outpatient observation on the 7th day after surgery, after removal of the sutures. Mouth opening at the time of discharge was 3.0 cm.
On the 2nd day after surgery, control radiographs of the skull in a direct projection and orthopantomography were performed. The position of the bone fragments and fixation structures was correct, no secondary displacements were detected (Fig. 6,
Rice. 6. Orthopantomogram of patient T. after surgical treatment. 7).
Rice. 7. X-ray of the skull of patient T. in a direct projection after surgical treatment.
During a follow-up examination after 1 month, an increase in mouth opening to 4.2 cm was noted; the patient’s chewing function and appearance were completely restored (Fig. 8).
Rice. 8. a — appearance of patient T. 1 month after surgery; b — amplitude of mouth opening of patient T. 1 month after surgery. As a result of dynamic observation and interdisciplinary treatment together with a physiotherapist, the prescription of physiotherapy and vitamin therapy on the affected side, the sensitivity of the skin and teeth in the zone of innervation of the inferior alveolar nerve was restored after 6 months.
Over a three-year observation period with examinations once every 6 months, a stable state of occlusion, absence of pain in the lower jaw and neuropathy of the inferior alveolar nerve were noted.
Osteosynthesis using ultrasound
With the help of metal fasteners, the jaw bones can be fixed quite firmly. But during surgery, it is most often necessary to cut through facial tissue and the salivary glands or branches of the facial nerve can be damaged.
It is less traumatic to perform osteosynthesis using ultrasound. In this case, the bone-fixing devices can be inserted shallowly into the bone and a small amount of scars remains on the patient’s face.
The doctor uses low-frequency ultrasound on a titanium plate with spikes. A plate with holes for the dental bur is placed at the fracture site and adapted to the shape of the jaw. An instrument is then used to make shallow holes in the bone through the plate. After which low-frequency ultrasound vibrations are directed to the base of the spines. In this way, the spikes gradually sink into the bone tissue, reliably fixing bone fragments. In this case, an antiseptic solution is supplied through the instrument, which treats the wound.
The bone tissue around the spines becomes denser under the influence of ultrasound. This occurs due to the large contact area, reducing pressure on the bone due to the use of a spike and the internal compression force of the bone tissue.
Ultrasonic osteosynthesis can reduce the time of surgery and reduce the amount of postoperative trauma. The method gives fewer complications and provides a good cosmetic effect.