Oral dermatitis is a local skin lesion, which consists of small papules (pimples), usually localized around the mouth, which determines the name of the disease. Another name for this disease is perioral dermatitis. Most often, this type of dermatitis is diagnosed in young women, less often in older women, but can also occur in children and teenage boys. Oral (perioral) dermatitis is an unpleasant cosmetic problem, which can still be eliminated if the cause of its occurrence is correctly identified and an effective treatment regimen is selected.
Medical is a clinic that diagnoses and treats many diseases, including dermatological ones. The treatment regimen in each specific case is selected individually, taking into account the characteristics of the patient’s body.
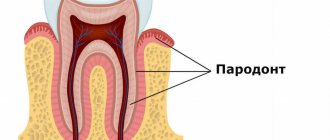
Perioral dermatitis
Perioral dermatitis on the face is a disease that affects the skin.
It appears in the form of small pimples that form in the area of the lips and mouth. It is accompanied by unpleasant itching, redness and negative consequences, which can be eliminated through a medical examination and properly selected treatment. In each specific situation, based on the results of the consultation, doctors recommend the patient medications that are relevant to his case. These include specialized pastes, ointments, sometimes hormonal drugs, as well as therapy that quickly eliminates burning and other symptoms. For perioral dermatitis, medications (ointment, tablets, cream) are selected based on medical diagnosis and tests. You can purchase the necessary medications for treatment on our website “Pharmacy 911”.
Skin care
To relieve itching and prevent infection of the affected skin, you need to properly care for your skin:
- It’s better not to take a shower, but to take a cool bath for about 10 minutes; use medicated bathing products with a soft base that cleanse but do not dry the skin;
- moisturizing and softening – the skin should not be dry to prevent flaking and cracking; regularly apply a moisturizer recommended by a dermatologist;
- Do not let your child scratch the affected areas to avoid infection - apply anti-itching products to the atopic areas.
Cream or gel relieves discomfort during an exacerbation and allows you to sleep, eat, and play peacefully. Apply the drug to cleansed skin, treat atopic lesions and the areas around them. Do not exceed the recommended dosage and frequency of use.
Causes of perioral dermatitis
Various factors become prerequisites for the occurrence of the disease. It is generally accepted that the disease can occur in waves, during which the irritation on the skin passes and reappears. Doctors often identify hormonal changes as the cause of perioral dermatitis. Symptoms appear as a result of:
- the use of drugs based on corticosteroids, which provoke the occurrence of rosacea, acne, blackheads and other cosmetic problems
- pregnancy, when the body is at the stage of serious changes and hormonal changes. Dermatitis often worsens before the onset of menstruation.
- using inappropriate decorative cosmetics
- the use of pastes with fluoride, which provoke irritation of the epidermis
- chapping after walking in the cold or sunbathing
- infectious diseases
- problems with immunity. They are usually caused by not getting enough vitamins.
Having discovered a corresponding problem, it is better to immediately go to see a doctor and find out how to treat perioral dermatitis on the face in adults.
Etiology and pathogenesis
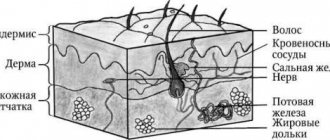
The main role in the pathogenesis of atopic dermatitis is played by hereditary determinism, that is, heredity. It is a number of hereditary mutations in genes that lead to disruption of the skin barrier and defects of the immune system. The patient also has hypersensitivity to allergens, an increased number of inflammatory mediators and a number of pathogenic microorganisms such as Staphylococcus aureus and Malassezia furfur.
The pathological reaction of the body, which provokes atopic dermatitis, occurs as a result of the interaction of three factors:
- skin barrier dysfunction;
- disturbances in the functioning of the immune system;
- influence of environmental factors.
In addition to the factors described, skin barrier dysfunction can be affected by:
- Reduced levels of ceramides (lipids), which protect the skin from aggressive environmental influences.
- An increase in proteolytic enzymes - substances that are responsible for the speed of cell reaction to external stimuli.
- Exposure to proteases from house dust mites or Staphylococcus aureus.
Violation of the protective barrier leads to high skin permeability to allergens and toxins. As a result of their penetration into tissues, a pathological immune response occurs. It comes from Th2 (T helper cell type 2), a special type of cell that enhances the adaptive immune response. They activate B lymphocytes that produce immunoglobulin E (IgE), which results in an allergic reaction.
During an immune response, characteristic itching and rash appear on the skin. Constant scratching stimulates the production of anti-inflammatory cytokines, which in turn cause chronic inflammation. As a result, the epidermis intensively absorbs allergens, which provokes microbial colonization of the skin.
Symptoms of the disease
The first sign that you need to undergo an examination is the appearance of small blisters (papules) in the mouth and chin. In severe cases, they can spread throughout the face, reaching the cheeks, nose, eyes and temples. Papules are filled with clear liquid. Color varies from flesh-colored to pink to bright red depending on the stage of the disease. Pimples appear singly or in groups. The skin in these areas becomes rough. Bursting, papules form crusts. If you accidentally touch one, pigmentation will eventually remain on the skin.
Patients do not always experience serious pain. The sooner treatment of perioral dermatitis on the face in children and adults begins, the easier it is to get rid of the disease, and the lower the risk of unpleasant consequences. When you notice the first symptoms of the disease, make an appointment with a dermatologist.
How is the diagnosis made?
To rule out or confirm allergic contact dermatitis, your doctor will perform a skin test. It consists of applying samples of common common allergens and those found in your workplace to the skin. If redness and inflammation occur, then there is an allergy to the applied substance.
In rare cases, a biopsy (analysis of a tissue sample) of the skin is required to rule out other diseases (psoriasis or other inflammatory dermatoses).
If the diagnosis of irritant contact dermatitis is confirmed, then treatment will have three directions:
- Avoid exposure to irritant.
- Restore damaged skin.
- Relieve inflammation.
If contact with an irritating substance cannot be excluded, then you can wear a respirator, goggles, overalls or, for example, latex gloves with an inner cotton layer. This is necessary so that sweat is absorbed by the fabric and does not harm the skin.
Risk groups and similar diseases
Signs of the disease are most often found in women, but children and adolescents periodically experience them due to weakened immunity. In place of the blisters, ulcers often form. When spread over the entire face, it becomes a threat to vision, which is especially important in the situation with children. Therefore, when checking with a specialized doctor about how to treat perioral dermatitis in children, it is worth paying a visit to an ophthalmologist.
In the case of teenagers, the disease may not be detected immediately, because, experiencing hormonal changes, boys and girls often encounter skin problems. Blackheads and acne affect most people, so it can be difficult to notice papules at an early stage. Patients prone to allergies also rarely accurately diagnose the disease. Perioral dermatitis in children is often attributed to hormonal imbalance.
Atopic dermatitis and infant formula nutrition
Of course, most modern mothers, despite any difficulties, will try to feed their baby with their milk. If the mother is healthy and does not take antibiotics or any other chemotherapy drugs, then breastfeeding is the best thing she can give her baby.
There are cases:
- The mother herself suffers from allergies or food intolerance to some foods, which force her to maintain such a strict diet that it becomes a real torment for both her and her child. But the rashes still continue;
- There is simply no milk.
In these cases, it is necessary to transfer the child to artificial feeding. The main thing you must learn and remember from this part of the article is that the so-called hypoallergenic mixtures are LOW allergenic, and not completely non-allergenic. That is, hypoallergenic formulas (HA) are intended for feeding children with a predisposition to allergies, but not for children with obvious diathesis.
Diagnosis of perioral dermatitis
Having noticed the first signs of the disease, having felt unpleasant symptoms, you need to make an appointment with a specialized specialist. The initial appointment with a doctor consists of an examination, a description of the medical history based on the patient’s complaints and information about the individual characteristics of his body and possible reactions.
Before treating perioral dermatitis, tests are one of the mandatory procedures. They allow you to identify the prerequisites for the development of the disease and accurately diagnose it, without confusing it with herpes, rosacea and other skin lesions. You will need:
- Dermatoscopy. Gives an assessment of the epidermis and helps assess the course of the disease
- Scrapings. Determine the infectious nature if the symptoms have a corresponding origin
- Allergy tests. Demonstrate the level of skin sensitivity to staphylococcus and streptococcus
As a result of the examination, the doctor explains to the patient how to cure perioral dermatitis, clinical recommendations are entered into the disease record. A course of medications and therapy is prescribed.
Allergic and atopic reactions of the skin and oral mucosa
Allergic contact dermatitis occurs in patients with hypersensitivity to a specific substance that acts as an allergenic trigger. Allergens can be: chemical salts of chromium, nickel, cobalt, turpentine and its derivatives, formaldehyde resins, cosmetics, insecticides, synthetic detergents, medications (antibiotics, sulfonamides, novocaine, formalin). Contact dermatitis (cheilitis) can be caused by cosmetics. Allergic contact stomatitis develops in prosthetic wearers with intolerance to materials, such as plastic.
In allergic contact dermatitis, cheilitis, stomatitis, erythema, papular and/or vesicular, bullous and urticarial elements are determined against the background of pronounced swelling of the connective tissue. Subjective sensations are noted - itching, burning, a feeling of heat in areas of contact with one or another irritating substance. However, in some patients, clinical manifestations may extend beyond the zones of exposure to allergenic agents.
Toxic-allergic dermatitis (toxidermia)
It most often develops under the influence of drugs and foods. Clinically common drug and food toxicoderma is manifested by a variety of rashes: true polymorphism of rashes. The appearance of numerous spotted, urticarial, papular, papulovesicular and, less commonly, pustular elements of the lesion, accompanied by itching, is possible. Sometimes total erythroderma develops.
Often the mucous membranes are involved in the process, on which edema, erythematous, hemorrhagic, and vesicular-erosive elements occur. The rashes are localized in areas susceptible to injury or throughout the entire oral mucosa.
The acute phase of the disease is characterized by intense itching, papules and vesicles located on an erythematous base. They are often accompanied by severe excoriations and erosions. Fixed toxicdermia may develop, the cause of which is most often the use of medications, for example, sulfanilamide erythema. One or more swollen hyperemic spots, round or oval in shape, appear, in the center of which a bubble may form. After the drug stops working, the inflammatory phenomena subside, and the stain persists for a long time. In case of repeated application of the same allergen, the spot again becomes hyperemic and undergoes a similar evolution. Fixed toxicoderma is localized on smooth skin and mucous membranes.
The acute phase of the disease is characterized by intense itching, papules and vesicles located on an erythematous base. They are often accompanied by pronounced excoriations and erosions, and the release of serous exudate. The subacute phase is accompanied by erythema, excoriation and peeling against the background of lichenification of the skin. In the chronic course, thickened plaques on the skin, an accentuated skin pattern (lichenification) and fibrous papules are observed.
Atopic dermatitis
The concept is collective in nature and includes terms denoting allergic inflammation of the skin (“Beignet’s pruritus”, “atopic neurodermatitis”, “childhood eczema”, etc.), with the exception of urticaria and contact dermatitis.
The term “trigger” is used to refer to the causes that cause the appearance and exacerbation of atopic dermatitis. Factors identified from the anamnesis can be both truly allergenic (protein substances) and non-allergenic irritants (non-protein chemicals: food additives, clothing dyes, overheating, dry air, scratching the skin, stress). They cause the classic pattern of “atopic” reaction of the immune system (allergen-antibody interaction, usually with the participation of class E immunoglobulins). Non-allergenic factors either intensify an existing allergic reaction or cause inflammation and symptoms of dermatitis on their own.
In patients with long-term chronic atopic inflammation, changes can exist simultaneously in different areas of the skin and mucous membranes.
Mild atopic dermatitis: mild itching, slight hyperemia, slight exudation, slight peeling, single papules, vesicles, slight enlargement of lymph nodes (up to the size of a pea). Moderate: Moderate to severe itching that disturbs sleep. Multiple lesions of the skin and mucous membrane with severe exudation or lichenification, multiple scratches and hemorrhagic crusts. The lymph nodes are noticeably enlarged (to the size of a bean).
Severe course: the itching is severe, painful, often paroxysmal, seriously disturbing sleep and well-being. Multiple, confluent lesions, severe exudation or lichenification, deep fissures, erosions, multiple hemorrhagic crusts. Almost all groups of lymph nodes are enlarged to the size of a hazelnut (in very severe cases - to the size of a walnut).
Diagnostic criteria for atopic dermatitis (stomatitis) combine the subjective sensation of itching and objective signs: dermatitis; presence of allergic status in close relatives; widespread dry skin; development of dermatitis before 2 years of age.
Laboratory tests include immunological, serological, allergological tests. An increased level of concentration of total serum immunoglobulin E and eosinophilia in peripheral blood may indicate atopic genesis of stomatitis. Skin tests (prick, scarification and patch tests) play an important diagnostic role in identifying allergens that cause exacerbation.
Intradermal tests are performed with inhalant allergens in difficult diagnostic situations. Intradermal tests with food products are strictly prohibited due to excessive sensitivity and the possibility of provoking an anaphylactic reaction.
Diagnostic criteria for atopic dermatitis combine the subjective sensation of itching and objective signs: dermatitis; presence of allergic status in relatives; widespread dry skin The application test is simple and accessible: the test substance is applied to the skin of the inner (flexor) surface of the forearm. The results of application tests are assessed during the first hour (immediate reaction) and after 24-48 hours (delayed reaction) based on skin hyperemia, itching, swelling, weeping at the site of application of the substance. Contraindications to skin testing are exacerbation of atopic dermatitis, acute intercurrent infections, chronic diseases in the stage of decompensation, pregnancy, tuberculosis, mental illness, collagenosis, malignant neoplasms.
Special allergy tests are based on genetic predisposition to atopy, which is determined by a significant number of factors: interleukins, especially IL-4 and IL-13, other cytokines, dendritic cells, Langerhans cells. In this regard, in a blood test during atopic reactions, an increase in the number of activated T-lymphocytes and Langerhans cells, and increased production of IgE by B-cells are noted.
In patients with atopic dermatitis, radioallergosorbent test (RAST), enzyme-linked immunosorbent assay (ELISA), multiple allergosorbent test (MAST) and other in vitro methods are used to detect specific serum IgE. Patients with suspected infection of the skin and mucous membrane are examined to identify viruses or bacteria that cause complications. The most common fungal flora, herpes virus, dermatophytes, streptococci, staphylococci.
Three fundamental positions in the treatment of atopic dermatitis:
- Therapeutic and cosmetic skin care.
- External anti-inflammatory therapy.
- Elimination of causative factors causing exacerbation (allergenic and non-allergenic triggers).
General rules for caring for the skin of patients with atopic dermatitis: eliminating dry skin and restoring the damaged lipid layer of the skin; exclusion (limitation, as far as possible) of exposure to irritating factors on the skin.
To eliminate dry skin, various moisturizers and emollients are used. For the purpose of softening, cosmetics based on physiological lipid mixtures should be used. Ceramides, free fatty acids and cholesterol are in a ratio (from 1:1:1 to 3:1:1, respectively). At the same time, many cosmetic products contain water, i.e., both moisturizing the skin and restoring its lipid composition are achieved (Mustela cream). A moisturizer and emollient must be applied to the skin as often as required so that the skin does not remain dry “for even a single minute.” As a rule, in the first days, 5-10 times the application of products to the skin is required, and subsequently the frequency of treatment is reduced to 3 times a day.
Antibacterial and antifungal drugs are used both independently and in double combination (glucocorticosteroid and antibiotic or antifungal agent), as well as in triple combination (glucocorticosteroid, antibiotic and antifungal agent): pimafucort, triderm, acriderm GK.
The following drugs have an anti-inflammatory effect: ASD III fraction, sulfur, tar, naftalan oil, zinc oxide, salicylic acid, dermatol, ichthyol. For the treatment of dermatitis in the acute stage, liquid forms of external antiseptics and combined action preparations (Castellani liquid, fucorcin, preparations containing salicylic acid, and others) are used as disinfectants and disinfectants, especially in cases of secondary infection and weeping of lesions.
The following drugs have an anti-inflammatory effect: ASD III fraction, sulfur, tar, naftalan oil, zinc oxide, salicylic acid, dermatol, ichthyol Anti-inflammatory activity is exerted by external glucocorticosteroids of “increased safety”: advantan (methylprednisolone aceponate), afloderm (alclomethasone dipropionate), lokoid ( hydrocortisone 17-butyrate), elocom (mometasone furoate). Advantan is applied to any area of the skin, including folds and face (once a day). Afloderm is used 1 to 3 times a day. Lokoid is used to treat dermatitis of any localization (1-3 times a day). Elokom can be applied to the skin of the face once a day.
Treatment with external glucocorticosteroids is the most effective method of treating children with atopic dermatitis. Therapy with external corticosteroids should be carried out long-term, until complete remission of the disease occurs.
Atopic cheilitis
It can occur independently or accompany the general picture of atopic dermatitis - a chronic lichenifying inflammation of the skin that occurs as a result of an allergic reaction that is triggered by both atopic and non-atopic mechanisms. The disease begins acutely, causing itching and clearly demarcated pink erythema, and sometimes there is swelling of the red border of the lips. Crusts appear at the scratch site. Acute phenomena subside, lichenification develops: the red border is infiltrated, covered with small scales and thin grooves. Small cracks form in the corners of the mouth. The process does not spread to the mucous membrane and Klein's area, but it involves the skin around the lips.
Atopic cheilitis occurs over a long period of time, exacerbations occur mainly in the autumn-winter period, and remission occurs in the summer. Atopic cheilitis in children manifests itself quite clearly: swelling of the skin in the perioral area, infiltration and peeling of the red border of the lips, radial striations. Papular rashes in the corners of the mouth are characteristic. Manifestations of atopic cheilitis and its relapses have cosmetic consequences (changes in color, lip architecture), disrupt the child’s nutrition, and interfere with the sanitation of the oral cavity. By the end of puberty, most people experience self-healing, but minor rashes may persist, mainly in the corners of the mouth. In some cases, psychosomatic disorders may occur.
Depressive reactions in patients with somatic and neurological diseases, which are based on factors including objective signs of bodily suffering, are also characteristic of dental patients.
In some cases, patients believe that character changes due to an aesthetic defect affect communication with loved ones or career growth. A special group in this regard is represented by actors, singers, teachers, and doctors. Excessive fixation of attention on individual anatomical features contributes to the emergence of psychogenic disorders, which may be the result of the idea of “losing one’s physical attractiveness” and inferiority in the eyes of loved ones. They can form as a result of diseases or conditions accompanied by changes in appearance. For example, the removal of front teeth leads to malocclusion (reduction of the lower third of the face), speech, and deterioration in the aesthetics of the dentition. The patient tries to talk less, stops smiling, and develops withdrawal. Soft tissue defects in the perioral area can lead to similar manifestations.
In some cases, patients believe that character changes due to an aesthetic defect affect communication with loved ones or career growth. A special group is represented by patients whose dental diseases can directly affect their professional activities: actors, singers, teachers, doctors. Their reactions are often of a violently emotional or hysterical nature; as a rule, there is a discrepancy between the severity of the condition and the psycho-emotional behavior of the patient. A person’s self-esteem of his own morphological characteristics depends on gender, age, and constitution. Young people, as well as unbalanced individuals, react more sharply to aesthetic flaws.
Nosogenic depression should be differentiated from psychogenic depression, when primary mental state disorders lead to refusal to communicate with the dentist. Complex treatment of nosogenic depression is carried out by a psychologist or neuropsychiatrist: medication, reflexology, physiotherapy (electrosleep). The dentist is required to comply with medical ethics and deontology, attentive attitude towards the patient, the ability to convince him of the effectiveness of modern methods of treatment in dentistry, and high-quality sanitation of the oral cavity.
Diagnostic criteria for atopic dermatitis include the mandatory presence of itchy skin (red border of the lips) and three or more of the following signs: the presence of dermatitis in the area of the flexor surfaces of the extremities; bronchial asthma or hay fever in close relatives; widespread dry skin; the first manifestations of dermatitis before 2 years of age. To clarify the diagnosis, consultation with an immunologist, allergist, or dermatologist is required.
Skin tests can be performed on almost all allergens. To exclude possible anaphylactic reactions, testing with allergens to which hypersensitivity is obvious should not be used.
Atopic cheilitis occurs over a long period of time, exacerbations occur mainly in the autumn-winter period, and remission occurs in the summer. In some cases, psychosomatic disorders may occur. To assess the allergic reaction in vivo, a mucosal test is performed on an intact area of the mucous membrane of the upper lip or hard palate. Removable dentures are made of plastic, on the inner surface of which there are 2 recesses. One is filled with an aqueous solution of the suspected allergen, the second with a physiological solution, the prosthesis is fixed on the teeth to create contact between the mucous membrane and the test substance. After 15-25 minutes, the prosthesis is carefully removed and the intensity of the reaction is determined after 1, 24 and 48 hours.
General treatment of atopic cheilitis requires the appointment of hyposensitizing therapy, including the use of antihistamines (suprastin 0.025 - 2-3 times a day; fenkarol 0.025-0.05 - 3-4 times a day; tavegil 0.001 - 2 times a day; loratadine ( Claritin) 0.01, Zyrtec (Cetrin) 0.01, Zaditen 0.01 - 1 time per day). In a number of patients, histaglobulin has a good therapeutic effect, which is prescribed in courses of 6-8 injections intradermally 2 times a week in increasing doses, starting from 0.2 ml to 1 ml, sodium thiosulfate orally or intravenously, sedatives (trioxazine, seduxen, melleril and etc.). In case of persistent atopic cheilitis, corticosteroids can be prescribed orally for 2-3 weeks: prednisolone (children 8-14 years old, 10-15 mg/day, adults, 15-20 mg/day) or dexamethasone, which is more effective. Corticosteroid ointments are prescribed locally (1% hydrocortisone acetate cream (hydrocortisone), 0.1% hydrocortisone butyrate ointment and cream (Laticort), 0.1% mometasone ointment and cream (Elocom), 0.5% - prednisolone ointment, 0.1% triamcinolone acetonide ointment (fluorocort), 0.025% fluorcinolone acetonide ointment and gel (flucinar).Bucchi rays have a positive effect.
Spicy, salty, spicy foods, alcohol should be excluded from the diet, and the amount of carbohydrates should be sharply limited.
Conclusion
The manifestation of allergic, toxic-allergic, and atopic reactions on the skin is often accompanied by pathological changes in the oral mucosa and the red border of the lips. Diagnosis of diseases requires not just a thorough examination, but specific laboratory tests to identify the etiological factor. Local and general treatment, including impact on individual links of etiopathogenesis, ensures the achievement of a positive result.
Treatment of perioral dermatitis
A confirmed diagnosis usually requires an integrated approach. The treatment regimen involves a complete refusal of cosmetics, as well as corticosteroid drugs. The patient is advised to use antihistamines to relieve burning and itching. Herbal lotions are used to help reduce inflammation. Reflexology is used to stop symptoms by pressing on specific points or placing special needles.
Having weakened the symptoms, you can resort to the use of antibiotics to get rid of the infection if it is diagnosed during the examination. For perioral dermatitis, medications are prescribed by a doctor taking into account age, body characteristics, allergies and pregnancy. Strengthening the immune system and restoring the balance of intestinal microflora are important. The latter may require a specific diet. Avoid fried, spicy and fatty foods, snacks, sweets and fast food. Give up alcohol and cigarettes.
How to choose products that are right for your child
A dermatologist may recommend not one, but several drugs to choose from. They have a similar mechanism of action, but their prices may differ significantly. It depends on the active and auxiliary substances, manufacturer, and release form. When choosing a cream for a child’s atopic skin, you need to take into account possible individual intolerance to individual components.
You need to purchase drugs from well-known manufacturers with a good reputation: Russian, European, American. It is equally important to contact large pharmacy chains that work directly with manufacturers and control the quality of drugs on sale - this will protect you from purchasing counterfeit drugs. Consider the age of the child: choose creams and gels with a pleasant smell so that the child enjoys going to the shower.v
When choosing drugs for oral administration, it is preferable to buy syrups, powders, drops, rather than tablets and capsules that are difficult for a child to swallow.
Prevention
Treatment with ointment for perioral dermatitis is not always a panacea. In some cases, the disease can return, so the course of taking medications can be long. Any irritant often leads to the appearance of the disease. Following simple recommendations will help you avoid possible risks:
- Check the composition of cosmetic products and treat their choice with special attention
- Don't neglect personal hygiene
- Strengthen your immunity
- Eat right and monitor your digestive health
- Be aware of allergies
- Monitor hormonal balance during pregnancy, in case of possible changes due to nervousness, illness or other reasons
Perioral dermatitis detected at the first stage is the easiest and fastest to treat, so remain sensitive to the body’s signals and begin the fight against the first symptoms of the disease in a timely manner.
Causes
A genetic mutation by itself cannot provoke the development of AD, since the disease occurs due to a number of provoking factors. These include:
- Atopenes (environmental allergens that provoke the production of allergic antibodies). They can be food (for example, milk, wheat, soy), pollen (wormwood, alder, ragweed), dust (bed mites, animal hair).
- Allergenic foods (spicy foods, alcohol, sweets, smoked foods, etc.).
- Medicines (vitamins, antibiotics, sulfonamides).
- Emotional stress.
- Frequent hypothermia.
In addition, we can identify factors that play a key role in exacerbation of the disease. This:
- Air pollution.
- Harmful working conditions (for example, if during work contamination occurs with solid oil particles or the skin is exposed to aggressive detergents).
- Viral infections (HIV, infectious hepatitis, etc.).
- Diseases of the gastrointestinal tract (pancreatitis, infectious gastritis).
- Pathologies of the endocrine system (thyrotoxicosis, dysmenorrhea, etc.).
Important! It is impossible to become infected with atopic dermatitis from another person. The disease is not transmitted by contact or airborne droplets.
Bibliography
- Adaskevich V.P. Perioral dermatitis: clinical picture, diagnosis, treatment / V.P. Adaskevich // Dermatology. – 2008. – No. 1. – P. 17–20.
- Grashkin V. A. Diagnostic criteria, epidemiology and substantiation of clinical and pathogenetic types of perioral dermatitis / V. A. Grashkin, M. S. Gromov // Voenmed. magazine – 2010. – No. 10. – P. 32–45.
- Rodionov A. N. Dermatocosmetology. Lesions of the facial skin and mucous membranes. Diagnostics, treatment, prevention / A. N. Rodionov. – St. Petersburg. : Science and technology, 2011. – 912 p.
- Karelina O. Yu. Perioral dermatitis: treatment with azelaic acid / O. Yu. Karelina, Yu. M. Karelin // Klin. dermatology and venereology. – 2006.
First complementary feeding for atopic dermatitis
You can start introducing the first complementary foods to children with diathesis from 5 months.
The first courses of complementary feeding are vegetable purees: zucchini, cauliflower or broccoli. A peculiarity of children with manifestations of diathesis is the slower introduction of complementary foods: for the first 3–4 days, the child is offered 2–3 grams of a new product in the first half of the day, gradually increasing its amount to 40–50 grams over 7–10 days.
The second type of complementary feeding will be: dairy-free rice or corn porridge, buckwheat porridge, but in cases where, after the introduction of certain porridges (sometimes with buckwheat), the child’s rashes may worsen, an earlier transition to meat complementary feeding (turkey, rabbit, horse meat, lamb) is possible ). Fermented milk products are contraindicated for children with diathesis, at least until 10 months of age. By the age of 10 months of a child’s life, the first fermented milk product should be cottage cheese, and only 2–3 weeks after that – kefir or yogurt, while the first fermented milk products in a child’s life should not contain flavoring additives.
Popular questions about perioral dermatitis
How can you get perioral dermatitis?
Dermatitis is not contagious, as it is an individual reaction of the body to the use of fluoride-containing pastes, inappropriate cosmetics and drugs containing corticosteroids. In the case of diagnosing infectious preconditions for a disease, it is worth finding out its nature, but it will not become a reason to limit communication.
How does perioral dermatitis manifest?
The disease is characterized by the formation of papules, blisters filled with colorless liquid, which spread around the mouth and along the chin, rising to the eyes. Dry skin, itching and burning accompany the disease, but in the first stage patients experience minimal discomfort.
Is it possible to cure perioral dermatitis?
The disease is easily treatable if you follow your doctor’s recommendations, use the necessary medications and avoid products and products that can cause perioral dermatitis. Depending on the extent of the damage, the course can take from several days to several months.
Bathing
After a light shower to thoroughly cleanse your entire body, apply Atopic Bathing Gel to damp skin from head to toe, massage lightly and rinse thoroughly. Dry your baby with a soft towel using blotting, but not rubbing, movements. After water treatments, apply Atopic skin softening cream for daily care. Apply it several times throughout the day: after washing your hands and washing your face.
When taking a bath, the water temperature should not exceed 36 degrees. Place your child in the water and offer him toys or other entertainment. After 5-7 minutes, apply Atopic Bathing Gel from head to toe and rinse well. After bathing, use Atopic cream for daily care, and if itching bothers you, let the cream absorb, and then treat the affected skin with an anti-itching drug.