Periarticular osteoporosis is a fairly “popular” pathology of the human skeleton. This disease is caused by degenerative processes in the bones. Moreover, not a single bone in the human body is immune from such a disease.
Periarticular osteoporosis
People often ask me to explain to them what it is - periarticular osteoporosis. The correct answer includes information not only about how the pathology develops, but also about methods of treating it.
What kind of disease is this?
This pathology is among the skeletal diseases diagnosed in humans. This disease is expressed in the destruction of the joint coupled with damage to the cartilage, as well as soft tissues located near the affected joint. The peculiarity of this disease is that it is quite large joints that are destroyed.
At first, the articulation of the bones hurts. Later, nearby soft tissues begin to become inflamed. This makes the arm or leg much less mobile. Then osteophytes (growths on the bones) appear, the joint begins to change shape, and the mobility of the limb decreases. Moreover, it can even be completely paralyzed.
This pathology is provoked by a deterioration in the absorption of calcium compounds by the musculoskeletal system and its subsequent weakening. And this happens due to old age, hormonal imbalances or other reasons.
Periarticular osteoporosis develops due to deterioration in the absorption of calcium compounds by the body
Currently, doctors distinguish two forms of osteoporosis, differing in the extent of the pathology:
- general, which occurs in at least a couple of areas;
- local, covering just one place.
The local form of this disease is called “local osteoporosis”.
This form is often diagnosed in the lower back, neck, joints - knee, elbow, and so on. If the disease is found in a joint, it is called “periarticular (aka paraarticular) osteoporosis.”
The main stages of the development of this pathology
There are three stages of pathology development in which the disease can still be successfully cured. Symptoms of the disease are determined by two factors - the stage of its development and the form of the disease itself.
Table No. 1. Phases of the disease
| Phases | Description |
| First phase | The pathology develops “insidiously”, without clear symptoms. At first you won’t even notice it if you don’t diagnose it by making an appointment with a specialist. |
| Second phase | It is possible that there are symptoms that can easily be confused with a lack of vitamins or simply chronic fatigue. Such as, for example, fragility and hair loss, nail splitting, yellowing of teeth, cramps during sleep, a more frequent pulse than normal. |
| Third phase | When the disease has already entered the incurable phase, pronounced symptoms can be noticed. For example, a painful joint begins to ache almost constantly. Small swelling may also appear there. And physical activity can cause a crunch in it. |
This stage is the last one at which medical assistance can still be provided. If the pathology continues to be ignored, it progresses, becomes neglected, and the patient may even become disabled. The disease can paralyze, deform and enlarge the affected joint, or even the entire rest of the arm or leg.
Features of the symptomatic picture
The symptoms of this disease depend on how widespread it is in the body. The main one is joint pain. They appear on the structure of the bones of the joint. The pathology cannot be noticed with the naked eye for a long time, but diseased bones deteriorate all the time.
And at the same time, with proper vigilance, signs of pathology can be noticed almost from the very beginning. These are the following:
- brittle nails;
- gray and falling hair;
- quickly accumulating fatigue;
- after physical activity, the joints ache and feel discomfort;
- teeth look sick;
- pressure surges;
- paroxysmal increase in heart rate;
- cramps in the leg muscles during sleep;
- hot temper.
Despite the fact that the disease does not manifest itself for a long time, it can be identified by some subtle symptoms
If the pathology is not cured immediately, it makes itself felt in the following ways:
- when moving, joints creak and crunch;
- they have incessant pain;
- the tissues near the joint swell, sometimes the skin turns red;
- stiffness of movement, which is most pronounced after sleep.
During the second degree of pathology, the symptoms of this disease in the affected areas are as follows:
- aching pain;
- crunching sound when moving;
- swelling.
In the third group, the following symptoms of the disease are immediately visible:
- increasing the size of fabrics;
- paralysis of diseased joints;
- changing the shape of the arms and legs.
Due to the gradual decrease in the working capacity of the limbs, up to its complete loss, and, consequently, the loss of the patient’s ability to move and care for himself, this stage is a serious reason for registering a disability for the patient. An advanced disease gradually deforms the joints, causing subluxations to appear in them.
The general form can also be identified by the appearance of the following signs:
- reduction of the patient's height;
- slouch;
- scoliosis.
Severity
There are several degrees of osteoporosis. They characterize the severity of the disease:
- Grade 1. Initial stage, at which there may be no clinical symptoms. Changes in bones can be detected during a random diagnosis for another disease. In some cases, brittle hair and nails and dry skin may occur.
- Degree 2. Destructive changes are isolated in nature. Changes are detected in one part of the skeleton. Most often this is the thoracic spine or lower extremities. Clinically, stage 2 osteoporosis is expressed in pain localized in the affected area. There may be convulsions and rapid heartbeat.
- Grade 3: Major changes are found in the bones. The bones become flattened, and when the spine is affected, a decrease in the height of the vertebrae is observed. In this regard, the patient's height decreases. Patients complain of severe pain and a hump forms on the back.
- Grade 4. The most severe stage of osteoporosis. Radiologically it is expressed in pronounced structural changes in the bones. The patient's height may decrease by up to 10 cm. Fractures occur due to minor injuries.
How can the further development of the disease be prevented?
First of all, you need to consider the following: it is the underlying pathology that should be treated, which is the cause of deformation of the bones near the joints. The main thing is to bring calcium metabolism back to normal, as well as restore bone mineral density.
The process and methods of treatment depend on the following factors:
- How severe is the mineral deficiency?
- how old is the patient from birth;
- what condition is his body in?
- Are there any other pathologies in it at the moment?
When inflammation of the joint reaches an acute phase, accompanied by deformation of the adjacent bones, the patient needs a protective regime, and the suffering limb should never be loaded in any way.
If the joint is fixed in a stationary state, this will make the healing of inflammation faster, and will also speed up the healing of the bones. The immobility of the joint can be ensured by applying plaster and splints.
One of the methods for treating pathology is fixing the affected area with splints, plaster or bandage.
In most cases, improving the condition of bones in such a pathology requires a lot of effort on the part of both parties - both doctors and the patient. The patient should be prepared to carefully carry out every day all the procedures that the doctor prescribes, even taking into account the fact that all of them will require a lot of effort, time and often also money.
The entire treatment complex consists of many stages. They have the following directions:
- relieving the patient of pain, which is achieved by using anesthetic drugs;
- relief from inflammation achieved through the use of non-steroidal antiseptics;
- if necessary, you can also use steroidal anti-inflammatory drugs, but only for a very short time;
- To restore density to the patient’s musculoskeletal system, calciotonin and bisphosphonates are used.
Markers of bone resorption
To assess the effectiveness of osteoporosis treatment, resorption (reabsorption) markers are used. Their reduction under the influence of therapy begins after 2–3 weeks and reaches normal after 3–6 months. Beta-CrossLaps (C-terminal telopeptides) are formed during the degradation of type I collagen, which makes up more than 90% of the organic bone matrix. Its measurement makes it possible to assess the rate of degradation of relatively “old” bone tissue. With a pathological increase in reabsorption in osteoporosis and in old age, type 1 collagen degrades to a large extent. This leads to an increase in the level of its fragments in the blood.
Currently, there is evidence of the effect of gene polymorphism on bone mineral density. Allelic polymorphism of the bone remodeling gene network is being studied to identify osteoporosis susceptibility genotypes. Widely distributed enzymes are acid phosphatases. Their level is analyzed to determine the degree of bone reabsorption and monitor antiresorptive therapy.
The use of various drugs for periarticular osteoporosis
Conservative treatment of this pathology includes the use of drugs from different pharmacological groups. Treatment of symptoms involves reducing pain, as well as relieving inflammation. This effect is achieved by using the following medications:
- non-steroidal antiseptics, for example, Diclofenac and Movalis;
- analgesics - “Pentalgin” and/or “Baralgin”;
- glucocorticosteroid hormonal drugs, but only in an advanced stage, and for a very short time - “Prednisolone” and its derivatives.
In this case, to carry out blockades inside the diseased joint, the drug is injected directly into its cavity.
Auxiliary techniques
The doctor may prescribe physiotherapeutic procedures. These are electro- and phonophoresis with antiseptic, anesthetic, vascular drugs, the use of therapeutic mud, paraffin baths, magnetic therapy, even quartz treatment. The latter is only dosed.
You should also pay attention to exercise therapy. The entire set of exercises is developed by a doctor who takes into account the patient’s age and the condition of his musculoskeletal system. It also determines how many exercises will be in the complex, as well as how often they should be repeated. Exercises should not tire the patient or give him unpleasant emotions. On the contrary, it will be good if they give him more strength and lift his spirits.
Exercise therapy is an equally effective method of treating periarticular osteoporosis
You can apply lotions of dimethyl sulfoxide (“Dimexide”), medical bile, and gently warm up the sore spot using warming and anti-inflammatory ointments.
When the patient is already reliably on the mend, doctors can recommend the following procedures:
- gentle painless massage with elements of light joint development;
- long-term use of chondroprotectors, for example, “Chondrolon” and/or “Teraflex”;
- courses of calcium supplements, including vitamins and antioxidants.
The complex treatment method also includes a change in diet. It should contain enough of the following products:
- dairy products;
- lean meat;
- fruits and vegetables;
- greenery;
- nutty.
In this case, the patient should eat fractionally, he should eat four to five small portions of food per day. At the same time, the following are strictly contraindicated:
- beer, vodka, wine and other alcoholic products;
- gas. beverages;
- everything is fried and fatty.
You can use it, but only a little:
- coffee;
- cocoa and products containing it (chocolate);
- sweet.
But he should consume as much kelp (seaweed) as possible, since there are a lot of microelements there.
ethnoscience
To treat this disease, there are also traditional medicine recipes. You can make bones stronger, ease pain, and prevent the development of pathology using the following means:
- mixtures that include eggshells and lemon juice;
- decoctions including parsley and dill;
- wraps with tinctures of comfrey and chamomile made with alcohol.
Some folk remedies will help get rid of discomfort caused by pathology
To normalize calcium levels, you can use the following traditional medicine:
- one piece of egg shell;
- one part propolis;
- two parts honey.
Fry the shells in the oven. Mix all three ingredients. Take the result 1 tsp. three times a day.
And here is another recipe that may be useful in the treatment of periarticular osteoporosis:
- one volume of fresh parsley/dill;
- ten volumes of boiling water.
Finely chop the greens, then pour boiling water over them. All this should sit for at least three hours. Take daily between meals, two to three times a day, one glass at a time.
You can also make lotions from tinctures/decoctions of horsetail, knotweed or comfrey. Use them like this for about 21 days.
How to protect teeth from falling out?
You need to pay more attention to your lifestyle and oral hygiene. The diet must be balanced; the diet must contain fresh fruits and solid foods that contribute to the natural cleansing of tooth enamel. After each meal, it is necessary to clean the oral cavity of food residues, and in the morning and evening, be sure to brush your teeth with a brush and toothpaste.
If no alarming symptoms have preceded it, and teeth begin to fall out, it is immediately recommended to undergo a full examination of the body. Perhaps he is trying to draw your attention to health problems with the help of teeth.
Warning
It is easier to prevent any pathology than to treat it, and osteoporosis is no exception. Moreover, preventing the disease is most important for those with a hereditary tendency towards it.
To avoid osteoporosis, it is enough to follow the general rules of a healthy lifestyle:
- include in your menu the maximum number of healthy products listed above;
- regularly give yourself some physical activity;
- take a walk every day;
- exclude from the diet all carbonated, sweet and alcoholic drinks, as well as strong coffee;
- follow the daily routine.
Sources
- Baranova I.A. Glucocorticoid-induced osteoporosis / I.A. Baranova // Practical pulmonology. - 2008. - No. 1. - P. 3-9.
- Baranova I. Caution: osteoporosis! / I. Baranova // Asthma and allergies. - 2004. - No. 4. - P. 18-19.
- Zulkarneev R.A. Prevention and treatment of osteoporosis / R.A. Zulkarneev, R.R. Zulkarneev // Kazan Medical Journal. - 2003. - T. 84. - No. 3. - P. 230-232.
- Lesnyak O.M. Diagnosis, treatment and prevention of osteoporosis in general medical practice. Clinical recommendations / O.M. Lesnyak, N.V. Toroptseva // Russian family doctor. - 2014. - P. 4-17.
- Postnikova S.L. Features of postmenopausal osteoporosis / S.L. Postnikova // General Medicine. - 2004. - No. 4. - P. 41-45.
- Rodionova I.V. Systemic osteoporosis and osteoporosis of the lower jaw / I.V. Rodionova [and others] // Nurse. - 2015. - No. 5. - P. 32-34.
Forecast of treatment results
For a considerable number of people, the diagnosis of “periarticular osteoporosis” is associated with disability. But more than half the success of treatment is determined precisely by the attitude with which the patient takes up the matter and how much effort the patient himself puts in, and not by the doctor and medications. So this pathology should be diagnosed in time so that the joints do not have time to become overgrown with thorns and growths.
It is important to detect the disease in time to avoid dire consequences
As soon as the patient is prescribed medication and rehabilitation, he is obliged to follow each recommendation as clearly and patiently as possible. But if there is even a slight deviation from at least one, only then can a person really become disabled, unable to even get out of bed. The prognosis of treatment is determined by when the pathology is diagnosed and how it is treated.
Answers to questions people ask
What is the specialty of a doctor who specializes in osteoporosis called?
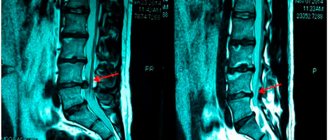
As soon as pain appears in the joints, you need to go to the clinic at your place of residence. There, describe all complaints to the local therapist. He will do an initial examination, after which he will issue directions for tests and x-rays. If osteoporosis, which is a consequence of a joint disease, is suspected, the doctor will prescribe densitometry, as well as consultations with colleagues and specialists in other, narrower areas of medicine. In this case, the patient’s “main” doctors will be rheumatologists. If necessary, he can be examined by an orthopedist or a traumatologist.
First of all, you need to contact a therapist - he will subsequently refer the patient to a doctor with a more narrow specialization
What is the reason that the development of osteoporosis goes hand in hand with rheumatoid arthritis?
There are several reasons for this:
- hormones and immunosuppressants that the doctor prescribes for the treatment of rheumatoid arthritis accelerate the development of osteoporosis;
- hormonal intra-articular blockades, used as painkillers and anti-inflammatory drugs, perform their tasks perfectly, but their side effect is the destruction of bones near the joints, so that they become brittle and brittle;
- Pain and decreased mobility are another reason why joints become weaker.
Is arthritis related to osteoporosis?
Calcium deficiency causes joints to deteriorate faster, making arthritis worse and more difficult to treat.
What is hidden behind the expression “joint replacement ”?
This is the installation of a prosthesis for a deformed joint. It requires a long rehabilitation.
Therapeutic exercise, gymnastics
Exercise therapy is a mandatory element of the rehabilitation of patients diagnosed with osteoporosis. Regular exercise can reduce the risk of developing fractures. Developed muscle tissue stimulates the strengthening of bone tissue. This protects it from increased fragility. As a result, exercise therapy helps not only strengthen bones, but also increase their density.
Women over 50 years of age are recommended to regularly perform exercises for both therapeutic and preventive purposes. The degree of load is determined individually. The patient’s age, severity of osteoporosis, and the presence or absence of concomitant diseases are taken into account.