Dental restoration through implantation followed by prosthetics is the most popular procedure in modern dentistry. Despite the seemingly high cost, implantation is completely justified and pays for itself after a couple of years by solving several problems at once. New artificial teeth perform all the stated functions, have an impeccable appearance and are indistinguishable from real teeth. High-quality dental implants last for decades; a fixed prosthesis does not cause discomfort and has good strength.
Dental implantation – what is it?
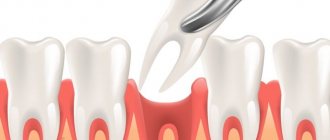
Patients often imagine the implant as a self-tapping screw, which is screwed into the bone, and a ceramic crown is placed on top, like a cap. And that's almost right. A dental implant is a rod that the doctor inserts under the gum and implants it into the bone. This is an artificial root, the basis of the future tooth. The second part of the structure is the aba between the base and the crown.
The implant is made in 99% of cases from a toxicologically inert titanium alloy. The popularity of the material is due to the following:
- due to the absence of a negative reaction from the body, titanium is an alternative to gold;
- upon contact with air, an oxide film is formed on the surface, facilitating survival;
- the titanium abutment connects well with composite cements and porcelain, so the result of implantation will be durable, almost indistinguishable from a real tooth with a “natural” crown;
- The titanium rod has a small thickness and weight; its installation allows you to maintain diction.
Basic terms
- A dental implant is a structure that is installed into the jaw bone during surgery and replaces the roots of the teeth, and also serves as a support for prosthetics;
- An abutment is a supragingival structure that imitates a tooth stump. It can be integral with the implant (non-separable design) or as a separate structure (demountable design);
- The healing abutment is a supragingival intermediate structure. Essential for creating a beautiful natural gum margin. (in the case where the abutment and implant are a single whole, not used);
- Osseointegration is a direct structural and functional connection between living bone tissue and the surface of the implant implanted into it.
Benefits of dental implantation
The main advantage of dental implantation: the adjacent tooth is not ground down (prepared), the treatment is local, only in the area of the missing tooth. Also important for patients:
- An implant in the bone prevents its resorption (bone without functional load quickly atrophies).
- Artificial teeth on an implant are practically no different from your own.
- Implantation can sometimes be performed immediately after tooth extraction. This is a one-step technique.
- Implants replace missing teeth of any length.
- Implants serve as the basis for a fixed (or removable) prosthesis. Instead of 3 missing teeth, you can install 2 implants, and the middle part with a narrower chewing surface to redistribute the load - a bridge.
- In some cases, replacing a tooth with a dental implant allows you to replace a removable denture with a fixed one.
- This is the best fulcrum for a removable denture, fixation improves, and the functional value of the denture increases by 20-25%.
Important: a dental implant in the bone, unlike a tooth, is installed rigidly in the bone and has no degree of mobility. Therefore, they try not to make an “implant-bridge-tooth” design.
Dental implantation allows you to restore several teeth at once
Expert opinion
Emir Romanovich Omerelli
Maxillofacial surgeon, implantologist
Experience: more than 13 years
The only option when a patient should refuse implantation in favor of another method is the presence of contraindications. If the matter is about the financial side of the issue, you should use convenient tools - for example, installment payments, but still get implants. In the long run, this choice will be more profitable. Since implants last a lifetime in 99% of cases.
Indications for dental implantation
Dental implants are installed when the formation of the skeleton is complete and bone growth has stopped. The upper age limit is individual. In orthodontics, there are cases where implantation was carried out for people 70-85 years old. If the patient is relatively healthy, the implant can be installed.
Implantation is indicated if:
- one tooth is missing, and next to it all are healthy (intact) or with limited defects;
- 3 or more teeth are missing in a row, up to complete absence;
- there is an allergic reaction to plastic;
- the patient has illnesses or psychological reasons due to which he cannot wear a removable denture.
Who should I consult?
At the ROOTT center, diagnostics and consultation with any doctor are FREE.
Vladimir Aleksandrovich Voznyuk
maxillofacial surgeon, implantologist
Experience: more than 33 years
Make an appointment
Igor Yurievich Malinovsky
Maxillofacial surgeon, implantologist
Experience: more than 11 years
Make an appointment
Emir Romanovich Omerelli
Maxillofacial surgeon, implantologist
Experience: more than 13 years
Make an appointment
all specialists
Leave a review
Contraindications to dental implantation
Absolute contraindications:
- Acute infectious diseases.
- Systemic bone diseases (for example, autosomal dominant osteoporosis type 2), osteogenesis imperfecta, Paget's disease.
- Blood diseases (polycythemia, leukemia).
- Recent radiation therapy to the head and neck.
- Malignant and benign tumors in the upper, lower jaw and soft tissues of the oral cavity.
- Incomplete teething, incomplete growth of skull bones.
- Mental instability.
- Drug addiction and alcoholism.
Relative contraindications to dental implantation:
- Age under 20 years. The body is growing, the implant will interfere with the normal development of the jaw. In addition, there is not enough bone tissue for implantation.
- Unsatisfactory condition of the oral cavity (rehabilitation required).
- Immunological or hematological diseases, decompensated diabetes mellitus.
- Smoking more than 15-20 cigarettes per day.
- Bruxism and other parafunctional habits. After implant placement, patients are advised to use plastic mouth guards at night.
- Long-term use of antibiotics, antidepressants, anticoagulants.
- Hormonal imbalance (menopause), because During this period, the bones become more loose.
- Pregnancy, after childbirth and during lactation. Due to hormonal changes, implant installation is possible no earlier than six months after the end of breastfeeding.
When a tooth is missing for a long time, the bone tissue is resorbed. About 20 years ago this was considered a reason for refusal, but now, before implantation, surgery is performed to increase bone volume.
Bone tissue augmentation allows implants to be installed even several years after tooth loss
If we are talking about implantation in the lower jaw, it is moved to the side to prevent the threat of damage to the mandibular nerve. Due to the possible rupture of the nerve, such an operation is performed very rarely and only in a hospital.
In various forms of periodontal disease, there is no gum tightly covering the tooth. After implantation, food particles will get into the “pocket”, which will lead to inflammation of the bone tissue. Therefore, the gum is formed:
- using a flap transplant from the palate;
- by deepening the vestibule of the oral cavity between the cheek and teeth (vestibuloplasty).
Medical consultation is recommended for people with endocarditis, heart failure, pathology of the endocrine system (thyrotoxicosis, diabetes mellitus, etc.). In case of hemorrhagic diathesis, blood clotting disorders (prothrombin time, or Quick reaction index (more than 30), implant installation is carried out in a hospital setting
Causes of pain after implantation
The most common reason for the development of pathology is the penetration of infection into the wound during or after surgery - for example, when using insufficiently sterile instruments or materials, the penetration of pathogenic bacteria through the edges of a loosely sutured wound, or when the sutures come apart. In some cases, with insufficiently qualified implantation, damage to the nerve structures of neighboring tissues occurs, which causes intense aching pain, which is practically uncontrollable by analgesics.
Another possible cause is the formation of a blood clot between the implant and the gum tissue, resulting from a damaged blood vessel or a bleeding disorder in the patient. Normally, after surgery, the patient experiences a subtle aching pain that goes away within 3 days, as well as slight bleeding, swelling and swelling at the operation site.
All this is a consequence of surgery and the reaction of the body’s immune system to it and goes away in 3-5 days. If the pain is severe, acute, there is severe swelling of the gums, fluid is released from under the installed structure, and all this continues for more than 5 days - this is a signal that you need to seek help from a doctor.
Types of implants
Fixed implantable prostheses can be intraosseous or extraosseous.
Intraosseous
If you look at the implant carefully, like an orthodontist, you can distinguish not 2, but 3 parts:
- supporting;
- transgingival;
- the largest is intraosseous.
The intraosseous shape of implants is different, repeating or not repeating the shape of the tooth root. It is by these criteria that the types of dental implants are most often classified.
The shape of the intraosseous part of the prosthesis is usually made in the likeness of a tooth root. Then healing after implantation will be quick, and the chewing load will be distributed evenly in the jaw.
Lamellar
The surface of these implants is textured and (or) corrugated. There is also a macro-relief resembling a snake. To allow bone tissue to grow through the prosthesis after implantation, holes are provided in the structure. Their total area does not exceed a third of the area of the intraosseous part.
There are:
- non-separable;
- collapsible, with internal or external thread for installing the head.
Root-like
Root-shaped (endosseous) implants include:
- cylindrical. The intraosseous part is smooth, with a small surface area. It is characterized by the lowest biomechanical performance in the shear test, so the cylindrical part is made textured (bioactive coating). They are produced only collapsible;
- screw. With different thread profiles, detachable and one-piece. The surface can be smooth or rough;
- basal. Longer, with a thread at the end to secure itself in the deep layers of bone.
Mini-implants that are installed for a limited time are also classified as root-shaped. This is not to say that they are thinner or shorter than regular ones. They have a simplified and slightly lighter design for people with osteogenesis disorders.
If the root-shaped implants are not connected to each other, their rotation can occur even after a period of bone tissue regeneration. The most common causes are medical manipulation and chewing load. Therefore, their design includes anti-rotation locks (anchors, holes, longitudinal grooves, etc.).
Types of root-shaped implants
Combined
The intraosseous part of the implant can also be a combination of cylindrical and plate-shaped:
- the central part is a cylinder;
- “lateral roots” - 2 asymmetrically or symmetrically located plates.
This type also includes disc, transmandibular (designed with a bracket and 2 pins) implants. Implants of a combined form are usually detachable.
Extraosseous
For osteoporosis or osteonecrosis of the jaw, extraosseous implants are sometimes used for patients in the older age group.
Subperiosteal
These prostheses are used for the rehabilitation of patients with significant atrophy of the jaw bone tissue. They are screwed into the periosteum on the side of the gum.
Intramucosal
They are used when there is a lack of bone tissue, when the patient refuses augmentation, sometimes as a temporary measure. A small, mushroom-shaped magnet is inserted into the gum. In the future, it serves as the basis for removable orthodontic structures.
Stabilization
When implanted, the prosthesis is mounted on the natural root of the tooth, takes root well, but is considered temporary, since the “base” dries out with age, like any bone tissue.
The advantage of implants of the “Impro” system (Germany) for internal prosthetics
German implants confidently lead in speed and ease of engraftment, reliability and service life. Other benefits:
- the possibility of installation at any density of jaw bone tissue (if necessary, they are implanted simultaneously with the sinus lift);
- one-piece orthopedic platform;
- minimal risk of rejection;
- maximum identity with the natural root;
- possibility of implantation in both the lower and upper jaw;
- wide choice of sizes;
- possibility of express implantation;
- uniform distribution of load on the jaw bone;
- prevention of bone tissue atrophy during service;
- smaller list of contraindications for implantation than its analogues;
- affordable price of intraosseous dental implantation system;
- unlimited service life and lifetime warranty.
There are several types of dental implants of the Impro system:
- for classical implantation;
- for express implantation into the socket of a newly extracted tooth;
- for instant loading (installed without large incisions and drilling under the root of the implant);
- mini implants.
The use of German implantation systems “Impro” allows not only to ideally restore the aesthetic and functional components of the dentition, but also guarantees the patient rapid healing of bone tissue due to special surface treatment (three-dimensional etching).
Stages of dental implantation
Installing an implant is a lengthy process. It is necessary for it to take root in the bone, so restoration of the dentition takes 3-6 months.
Planning and preparation
Preparation and planning of surgical intervention is:
- X-ray examination (orthopantomogram, targeted images, determination of projection distortions). A steel ball is fixed in the area of the proposed permanent prosthesis, and the length of the implant is selected based on the images.
- Determination of the thickness of the alveolar process of the upper and lower jaw using an osteometer (under anesthesia), determination of the profile of the alveolar process or part of it at the site of the proposed implant on diagnostic plaster models. Based on these data, the diameter of the implant is selected for future implantation.
- Making a diagnostic plaster model with the restoration of missing teeth (from wax or plastic), taking into account intermaxillary interaction, on the basis of which a radiopaque plastic template is created.
- Computed tomography examination. Before scanning, all removable metal dentures are removed; dental implantation will be successful if the patient is scanned motionless with his mouth slightly open.
- Creation of a 3D model of the jaw. Axial sections are obtained on a CT scan, then a computer program creates a three-dimensional image and necessarily visualizes the neurovascular bundle. Since teeth, bones, and soft tissues have different densities, based on research data, the program provides the ability to visualize the outer skin and internal structures, as well as turn off the visibility of various anatomical objects.
- Determining the type of implants and their installation sites, taking into account the qualitative and quantitative composition of bone tissue (planning the surgical stage of implantation). Taking into account the bone density readings, the optimal location for placing the implant is selected, and the distribution of chewing load is assessed. As a rule, the largest implant that can fit in a given volume is selected.
- Jaw prototyping. Checking the relationship of installed implants with antagonist teeth or opposing implants.
- Use of a surgical prototype guide. When the location of the prosthesis is strictly limited (complex anatomical conditions), the implant is positioned at a certain angle. Then, using rapid prototyping, a special surgical template is made, in which titanium cylinders are installed for drilling strictly at a given point and at the correct angle. If there is a deficiency of bone tissue, sinus lift surgery is planned.
Surgical stage
Dental implantation surgery is performed under anesthesia:
- infiltration, familiar to most local “freezing”;
- conduction, when the anesthetic is injected into the paraneural space.
Most pain during implantation is associated with the crushing of blood against the cancellous bone, as well as increased pressure on the nerve endings. To reduce pain during and after surgery, patients with high blood viscosity are advised to take instant aspirin (500 mg) 30 minutes before. before the start of the operation. In addition, when installing an implant, a constant level of bleeding is important (for this purpose, the bone bed is often washed out). Blood fills the voids between the surface of the implant and the bone, improving osseointegration (engraftment of the implant into bone tissue).
Dental implantation begins with an incision with a disposable scalpel and tilting the mucoperiosteal flaps to the sides. According to the wide flap technique, the incision is made in the middle of the alveolar ridge, and the interdental gingival papillae are carefully dissected. Thanks to this technique, there is no need to make a vertical incision, which leaves a visible scar during healing.
Another cutting technique for implantation is the use of a circular mucotome knife. This ensures minimal invasiveness (penetration of pathogenic microorganisms through the wound) and increases the resistance of the epithelium adjacent to the implant to pathogenic effects. There are no stitches for this incision. Any preparation is carried out with copious cooling with sterile saline solution.
The location and position of the prosthesis depend on the defects of the dentition and anatomical conditions. For example, when multiple implants are installed in an edentulous upper jaw, they will have a fan-shaped divergence due to the anatomical shape and inclination of the jaw itself. Read more about the features of upper teeth implantation here.
If the alveolar bone is well preserved when installing a prosthesis during implantation, several rules are followed:
- The distance between implants is at least 2-3 mm. Otherwise, the bone remodels and atrophies.
- The implants are installed at a slight angle to each other in order to evenly distribute the vertical load and reduce the concentration of excess stress.
- The tilt of the implant is mesio-distal.
- During implantation, bone tension is taken into account (the difference between the size of the prepared bone bed and the diameter of the subosseous part of the implant). The diameter of the endosseous part should be 0.2-0.5 mm larger. Then it is possible to avoid mobility of the implant and achieve rapid osseointegration.
Be sure to ensure that there is blood in the implant bed. This avoids the formation of air cavities between the bone and the implant. Understanding this fact is a guarantee of peace of mind during implantation.
Remember: dental implantation necessarily involves the formation of blood clots. This is the norm, you should not be afraid of blood.
Before inserting the implant, its surface is moistened with saline solution to reduce friction. If the implantation is one-stage, very often a gum former is immediately installed instead of an obturation screw. During two-stage implantation, mucoperiosteal flaps are hermetically sutured.
Orthopedic stage
The gingival cuff former is replaced with a support head. On the day of implantation, it is possible to manufacture and fix a provisional orthopedic structure (or 1-3 days after surgery). Then an impression is made using impression material, and then the prosthesis itself. This is done by an orthodontist who completes the restoration of the dentition.
The entire sequence of actions (cast, making a jaw model, crown or prosthesis frame) is absolutely similar to making a crown. Production time depends on the material and volume of work.
Postoperative period
On the 11th day after implantation, the sutures can be removed. In areas remote from surgery, patients keep their mouth clean and use chlorhexedine-containing products to rinse. Temporary removable dentures can begin to be worn on the 14th day, but the longer the patient goes without it, the better.
The soft lining, which gradually becomes denser, is changed after 6-8 weeks. In addition, for some implants it is necessary to tighten the transocclusal screws, so a dentist’s control is required after 6 weeks, and then after 3 - 5 months.
How to reduce pain after implantation?
It is necessary to understand that after surgery the body needs time and energy to recover, so it is important to carefully listen to the doctor’s recommendations and strictly follow them - refuse solid food during recovery, chew on the other side of the jaw, do not drink alcohol or smoke, do not go to the sauna and a sauna in the first month after implantation.
You must brush your teeth carefully, using a soft-bristled brush, try not to injure the tissues of the oral cavity, avoid physical impacts (impacts, shocks), observe good hygiene, promptly use medications (including antibacterials) prescribed by your doctor, and do not take other medications. without consulting a doctor.
To reduce pain, you can use cold lotions (with ice) in the first hours after implantation. They are used no longer than 20-30 minutes to avoid tissue hypothermia.
Regularly (especially after eating) rinse your mouth with water and antiseptic solutions (for example, chlorhexidine-based).
Healing gels (such as Metrogyl Denta) or cotton swabs moistened with an antiseptic solution (chlorhexidine) can be applied to the area of the gums where the sutures are located.
You can use analgesics (ketanov, paracetamol, ibuprofen, nimesil), observing dosages and intervals between doses. Their effectiveness is enhanced by drinking plenty of fluids.
Among folk remedies, it is allowed to use a decoction of chamomile, eucalyptus, calendula, plantain, as well as a pulp of fresh aloe leaf. You can rinse your mouth with decoctions (or tincture diluted in water) or moisten cotton swabs and apply to the sore spot.
Attention! Any means are used only as prescribed by a doctor or in agreement with him! Carefully follow the requirements and recommendations of the implantologist and do not self-medicate. And if the pain is too severe, consult a doctor.
Types of implantation
Based on the mutual influence of implants and oral tissues (hard, soft), several types are distinguished.
Endodonto-endosseous
Dental implantation, which uses a pin and various fixation elements in bone tissue. The pin is placed in the dental canal, so for the orthodontist, due to special manual skills, this is one of the most difficult implantations.
Endosseous
Otherwise, intraosseous. The most popular implantation, with good results of engraftment and distribution of occlusal load. The implant is inserted into the bone through a mucoperiosteal flap. The intraosseous part is made in the form:
- screw;
- plates;
- cylinder.
In addition to prosthetics of 1 tooth, this type is used in the all-on-four and all-on-six implantation method in the case of complete absence of teeth. Implants (4 or 6) will be the basis for attaching the bridge. The new All-on-3 (Trefoil) implantation method has been used since 2017, 3 implants are used, the acrylic prosthesis is permanent, manufacturing takes 1 day. Also suitable for full dental implantation.
Implants for endosseous implantation
Subperiosteal or subperiosteal
Dental implantation is recommended when alveolar bone degeneration is evident. First, an impression is made from the bone, and an implant is made from it. Then it is installed under the mucoperiosteal flap. For an orthodontic surgeon, such implantation is a top flight, since due to limited space and bone structure, it is difficult to choose a rational design that will not subsequently affect the dentition and correctly distribute the chewing load. With the advent of 3D modeling, the percentage of unsuccessful implantations has decreased, however, in difficult cases it is better to contact a dental clinic with extensive experience, since significant difficulties arise during the installation process.
Intramucosal
It is also called insert implantation. The implant resembles a button, very small. The bone is not drilled; installation occurs in the mucous tissue of the alveolar processes. The risk of installing an implant is minimal
Submucosa
In the literature for dentists, there is a second name - submucosal type. The easiest type of implantation, the risk of surgery is reduced to zero. Magnets are inserted into the transitional fold, creating a valve zone and retention (holding) of removable dentures.
Transosseous
When the atrophy of the lower jaw is clearly expressed, implants are installed through it in the intermental region and secured to the basal edge.
Cost of different types of implantation
An important factor in choosing the type of implantation is the price. To make it easier for you to decide on the method of installing implants, we have indicated in the table below the approximate cost of all types of implantation that are in demand in modern dentistry. Therefore, you will not find prices for endodontic-endosseous, subperiosteal and transosseous techniques in it, since these types of implantation are no longer used.
| Type of implantation | Price for installation of one implant |
| Endosseous (intraosseous) implantation | 20 -35 thousand rubles. |
| Basal implantation | from 35 thousand rubles. |
| Intramucosal implantation | from 20 thousand rubles. |
| Laser implantation | 40 -60 thousand rubles. |
| Express implantation | from 40 thousand rubles. |
Techniques
Basic surgical techniques in orthodontics include one-stage and two-stage implantation.
Two-stage
Standard implantation, which can be performed in any dental office.
Stage 1
The gum flaps are cut and moved back, clearing the bone for the implant. An axial guide channel is created with a 2-2.5 mm drill, and it is expanded with a drill of a larger diameter.
When the root portion of the implant is screw-shaped, the bone is manually threaded using taps. Then the endosseous element is screwed in using the implant lead.
If cylindrical implants are used, the bed is formed using a reamer or a special cutter. When using combined implants, first the cylindrical part is formed using fissure burs, and then preparation for the plates is carried out.
The intraosseous part of the implant is installed just below the height of the alveolar ridge. To protect against bone tissue getting inside the implant, the canal is closed with a plug, the gum flaps are raised and sutured.
Stage 2
It is carried out no earlier than 2-3 months, when it becomes clear that the root-like part of the implant is successfully engrafting. After activation of local anesthesia, the gum is excised again and the plug is removed. After flushing the canal, the upper part of the implant is screwed in. Additional incisions are sutured.
Two-stage implantation technique
One-stage
It differs from the two-stage procedure in that after implantation the entire implant protrudes into the oral cavity. It is installed by cutting the gum, or in a simplified way. This is the so-called bloodless implantation technique (no stitches are applied):
- The mucous tissue and periosteum are excised with a perforator.
- The bone bed is prepared with a drill, circular saw, or fissure bur.
- The implant is installed.
These methods of dental implantation give the same long-term results. If there are any doubts about the patient’s compliance with hygienic requirements for the cleanliness of the oral cavity, they resort to a two-stage procedure. Then the possibility decreases:
- accumulation of food plaque and bacteria on the surface of the implant;
- development of the inflammatory process;
- implant rejection.
If oral hygiene is maintained, the implant is installed in one go.
According to the form they are distinguished:
Cylindrical
Thanks to the porous structure, a strong connection with the surrounding bone tissue is ensured. Currently, cylindrical implants are produced dismountable, designed for a two-stage application method.
Screw
In order to have an idea about these implants, let's look at the structure of the jaw bone.
The cortical plate is a kind of shell, the strongest, consisting of 95% mineral salts.
Spongy bone is the main layer of bone tissue, represented by crossbars and septa with many small vessels (capillaries). It is in this section that the roots of the teeth are located.
The basal layer is a continuation of the spongy layer, but the septa are located closer with a small number of vessels. Maximum strength and thickness .
Screw implants have a number of advantages:
- Cone shape;
- They are installed in place of the roots of natural teeth, that is, in the spongy layer. When chewing, they also transfer the load to the surrounding bone tissue, thereby maintaining metabolic processes in it at the proper level. It turns out that this type of implant is the most physiological;
- The presence of threads, which increases the area of contact with bone tissue, and, consequently, faster osseointegration is noted;
- They can be collapsible or non-removable, one- and two-stage, have a smooth, rough surface or a coating of bioactive materials;
- They come in different diameters and lengths, which expands the indications for their use.
One of the main conditions for the use of screw implants is the presence of a sufficient volume of high-quality bone. But even if there is a lack of it, it is possible to establish them with the help of additional operations (sinus lifting, bone grafting, etc.). Only the duration of treatment and recovery will change.
In today's market you can see many implant manufacturers. Let's take a look at the leading representatives.
How are dentures attached?
Fastening the prosthesis after implantation depends on whether it will be removable or not.
Fixed prosthetics
In this case, the prosthesis is installed by an orthodontic surgeon once. Fastening can be using locking mechanisms or dental cement.
For cement
The prosthesis is attached to the head of the implant using dental cement. There are no holes for screws - the dentition looks solid. Fast production and low costs, coupled with speed of installation, made cement fastening widespread.
Flaws:
- Such fastening poses a risk of an inflammatory process under the prosthesis if cavities remain in the cement fixation between the gum and the prosthesis.
- If it is necessary to remove the prosthesis, parts of it may be damaged.
- If the intramaxillary space is small, a small abutment is placed, the fastening becomes less reliable, and there is a risk of losing the crown.
- Difficult to remove remaining cement.
On attachments
The prosthesis is securely attached to the implants using clasps and attachments. The shapes of the locks are different; they can be located on the outside of the crown or on the inside.
Removable dentures
Removable dentures are attached differently.
Screw fixation
The prosthesis can be attached with a screw to the implant:
- to the intraosseous part;
- to the head.
If a custom abutment is made, it is secured with a lateral screw.
- Advantages of screw fixation:
- If necessary (broken, chipped abutment), it is easy to unscrew and replace.
- Does not interfere with contouring implants during soft tissue restoration.
- The reason for the screw breaking is the incorrect distribution of the chewing load; for the orthodontist this is a clear signal with a ready-made sequence of actions.
Flaws:
- Some increase in gum volume.
- Visibility of access holes (they are covered with filling material).
- A larger channel for the root part of the implant in the bone.
Push-button fastening
To secure the prosthesis, 2 implants are sufficient; push-button locks in the form of a ball or coupling are used.
Magnetic fixation
Usually magnets are soldered to the abutment. This fixation holds the prosthesis well when opening and closing the mouth, however, when chewing (horizontal movements), the prosthesis may move to the side, because the magnet cannot resist the horizontal shear force. Frequent shifts are one of the causes of complications of dental implantation, as they loosen the implant.
Beam mount
The design splints several implants (2-4), preventing their loosening. Therefore, the fixation of the prosthesis is strong, much better than a push-button one. Sometimes beam fastening is combined with telescopic or locking elements, and expanded with additional beams. Then the pressure on the gums decreases and the likelihood of inflammation decreases.
Prosthesis with beam type fastening
Telescopic system
The prosthesis with cylindrical or conical holes in the crowns is simply placed on top of 4 implants. This is one of the massive designs; when you wear it, your facial features change slightly. But with such fastening there are practically no complications of the mucous tissue under the prosthesis.
Which dental implantation method to choose?
The method, implant and type of prosthesis are selected individually after an examination; it is not chosen by the patient (although his wishes are listened to), but by a collegial surgeon, orthodontist and dental technician. Therefore, you need to contact specialists with many years of experience.
They take into account indications and contraindications for dental implantation based on X-ray and other studies, and simulate the implantation process using dental computer programs. However, they usually offer several options (crown - metal ceramics or zirconium dioxide, type of prosthesis, etc.), since the price of dental services depends on the materials used.