Indications
Most dental procedures are performed under local anesthesia.
Its use is mandatory in the following cases:
- Treatment of pulpitis (first visit)
- Periodontal operations (closed and open curettage, gingivoplasty, elimination of gum recession, guided tissue regeneration)
- Prosthetics of vital (living) teeth with fixed structures (crowns, inlays, onlays, bridges)
- Tooth extraction, implantation, bone tissue augmentation, tooth-preserving operations (apex resection, root amputation, hemisection), making incisions for periostitis, pericoronitis, opening abscesses and phlegmons, removing cysts and tumors
In some situations, anesthesia is mainly used, but patients with reduced sensitivity can do without it:
- Treatment of caries, wedge-shaped defects, non-carious lesions, periodontitis
Procedures that most often do not require anesthesia, but particularly sensitive patients may require:
- Professional oral hygiene
- Restoration of pulpless teeth (both fillings and crowns or inlays)
- Removable prosthetics (if the gag reflex is increased, there may be a need for mucosal anesthesia)
Anesthesia is not recommended:
- Oral examination
- Preventive measures (fluoride varnish applications, fissure sealing)
- Teeth whitening
- Orthodontic treatment
Children often tolerate tooth preparation for caries much easier than an injection into the gum. Therefore, you should not necessarily give an injection on your first visit before starting treatment. It makes more sense to try drilling without anesthesia and switch to it only if the child complains of pain. Compassionate parents, do not worry that your child may experience hellish pain and refuse further treatment. Dentin sensitivity in children is less than in adults. The likelihood of getting psychological trauma from an injection is higher.
Diagnostic local anesthesia is used to identify the diseased tooth. When several adjacent teeth are severely damaged, it is difficult for both the patient and the doctor to determine the source of pulpal pain. In order not to depulpate them all, you can give one anesthesia and wait. If the pain has passed, it should be treated first; if not, anesthetize the next tooth and check the reaction.
Anesthetics with a high vasoconstrictor dilution of 1:100000
In pediatric practice, they are used only for a number of surgical interventions for the purpose of hemostasis. The duration of anesthesia is 75 minutes for dental pulp and 360 minutes for soft tissues.
Such outpatient interventions include the removal of an impacted, supernumerary tooth, apperculectomy, cystectomy, plastic surgery of the frenulum and vestibule of the oral cavity, and removal of a tumor. The use of anesthetics with high dilutions of epinephrine for other types of dental interventions is unjustified and disproportionate to the volume of intervention.
Types of local anesthesia in dentistry
Superficial (application) anesthesia
It is carried out by spraying, irrigating or lubricating the mucous membrane with a topical anesthetic (most often lidocaine). The main advantage is that it is painless (no injection is required). However, it is only effective for soft tissue anesthesia. It does not reduce tooth sensitivity at all. Therefore, the use of only superficial anesthesia in the treatment of small carious cavities or ultrasonic teeth cleaning is unjustified.
Often used to reduce pain before an injection.
Application anesthesia helps patients with an increased gag reflex (when taking impressions, for example).
To remove mobile baby teeth in children, superficial anesthesia is sometimes sufficient, but if the roots have not yet completely resolved, then such anesthesia is not enough - infiltration anesthesia is necessary.
Lubricating with ointment is preferable to spraying with a spray because it is easier to control the area of application. When splashed, the anesthetic can get onto the soft palate, creating discomfort and additional anxiety for the patient in terms of difficulty breathing (choking).
Infiltration anesthesia
It is carried out by injecting an anesthetic drug into the place whose sensitivity needs to be reduced. The anesthetic solution from the injection point spreads to nearby tissues (including dental nerves), temporarily eliminating pain and other sensations. When treating teeth, infiltration anesthesia is applied to the projection of the apexes (where the nerves enter the canals of the tooth). This type of anesthesia is preferred for the upper and lower anterior teeth. For lower chewing teeth, infiltration anesthesia is ineffective (due to the thick and dense bone tissue in this area).
The safest injection method of all. Possible minor complications include hematomas (bruises) and stomatitis at the injection site.
When anesthetizing single-rooted teeth (incisors and canines), one injection on the cheek side is sufficient. Multi-rooted teeth (molars and some premolars) require injections on both sides: buccal (labial, vestibular) and palatal (lingual on the lower jaw). On the palatal side, the injection is more painful than on the buccal side (since the mucous membrane of the palate is denser, and the injected solution injures the soft tissues more).
With periostitis, abscess and other acute inflammatory processes in soft tissues, the effectiveness of infiltration anesthesia decreases, and the pain of the injection increases. In such situations, conduction anesthesia is indicated.
Conduction anesthesia
It consists of blocking the sensitivity of the entire nerve trunk by introducing an anesthetic to the place where it exits the jaw to the surface. In this case, several teeth can be treated at once.
There are the following subtypes of conduction anesthesia in dentistry: mandibular and torusal (the lower teeth on one side are anesthetized), mental (lower premolars, canines and partially incisors), palatal (upper teeth on the palatal side), incisive (upper incisors and canines on the palatal side) , tuberal (upper molars on the buccal side), infraorbital (upper premolars and canines on the labial side).
Conduction anesthesia is not always successfully performed by the dentist. You have to do it again from time to time. Due to the technical complexity of the implementation: the doctor does not see the nerve trunk, the needle is brought to the average location of its location in the anatomical atlas, and a particular patient may have individual (quite different from the standard) anatomical features. The introduction of an anesthetic at a considerable distance from a large nerve does not allow achieving a complete block of sensitivity.
Even worse is a direct needle hit on a nerve during conduction anesthesia. In addition to sharp pain (as patients describe it - “electric shock”), subsequent loss of sensitivity is possible. Most often, mandibular or torus anesthesia is performed, so paresthesia of the tongue and lower lip (one half) is most common. Tingling, loss of taste, and discomfort may last for several weeks or months. Usually, sensitivity returns on its own without any manipulation, but in rare cases, paresthesia remains for life.
Therefore, conduction anesthesia is not recommended when safer infiltration can be used.
Intraligamentary anesthesia
It is carried out by injecting the drug into the periodontal ligament (located between the alveolus and gum on one side and the tooth on the other). To completely remove the tooth, several injections are required around the perimeter. Only one tooth is numbed. Effective for all teeth, but extremely painful. It is recommended to use it after preliminary infiltration anesthesia.
If the anesthetic is administered excessively, necrosis of the periodontal ligament (with subsequent tooth loss) is possible. If anesthesia is used to remove a tooth, this problem is irrelevant.
Intrapulpal anesthesia
It is carried out by injecting an anesthetic directly into the pulp of the tooth in case of pulpitis. This injection is very painful, so it is given only after preliminary infiltration, conduction or intraligamentary anesthesia. The tooth is still pre-drilled (otherwise you won’t be able to get to the pulp). The effectiveness is close to 100%, the analgesic effect does not last long, but usually this period of time is enough to remove the pulp.
Apart from pain, there are no complications.
Intraosseous anesthesia
It is achieved by introducing an anesthetic into the bone tissue surrounding the tooth after its perforation. Preliminary infiltration or conduction anesthesia is required. Due to the technical complexity of implementation, it is rarely used. Only if other types of local anesthesia have failed. About 90% effective, can block multiple teeth.
Modern anesthetic drugs in outpatient dentistry
Moscow Medical Academy named after. I. M. Sechenova
Department of therapeutic dentistry.
Elective abstract work on the topic:
Modern anesthetic drugs in outpatient dentistry.
Completed by: III year student, group 12
Faculty of Dentistry
Vyrypaeva Maria Glebovna
Teacher: assistant of the department Sokhova Inna Anatolyevna.
Content:
1. Introduction. Modern requirements for local anesthesia for dentists of all specialties. 2-4 pp.
2. Dosage forms of local anesthetic drugs and carpule technology. 4-7 pp.
3. Basic indicators of anesthesia when working with articaine anesthetics. 7-11 pp.
4. Conclusion 12 pages.
5. List of references used, 13 pages.
The problem of pain during various types of dental treatment has recently begun to be successfully solved with the advent of effective articaine anesthetics on the Russian market, but a number of problems associated with anesthesia remain unresolved, which make even experienced specialists worry:
- the problem of guaranteed pain relief for all categories of patients;
- problem of allergic reactions;
- the problem of individual differences in anatomical structure, etc.
Many unnecessary problems and complications arise from the incorrect use of effective anesthesia techniques, which often arise due to neglect of the use of aspiration testing. It is also necessary to adequately select an anesthetic according to the individual characteristics of the patient and his predisposition to allergic reactions.
Modern requirements for local anesthesia for dentists of all specialties.
The requirements for local anesthesia put forward by dentists - therapists, surgeons and orthopedists - are similar. Currently, increased demands are placed on anesthesia in dentistry. Anesthesia must be predictable, i.e. the doctor performing the anesthesia must be confident that the anesthesia will work on any patient and that the pain relief will be sufficiently deep. In this case, it is necessary that the anesthesia lasts long enough, i.e., as long as the manipulation requires, and it is also desirable to avoid repeated injections and the effect begins as soon as possible. It is important that the injection itself is also painless.
Anesthesia must be safe for the patient, that is, it must not cause allergic reactions, must not be toxic, and have as few adverse reactions and complications as possible. Should be safe enough for patients at risk with concomitant diseases.
It should be noted that the entire complex of put forward requirements is realistically feasible. This depends on many factors: firstly, on the qualifications, knowledge and experience of the specialist, secondly, on the initial psychosomatic state of the patient, thirdly, on the competent choice of the drug for local anesthesia and premedication (if necessary), fourthly, on the chosen anesthesia technique, etc.
If you take the first four factors wisely, then the ineffectiveness of anesthesia, individual characteristics of the maxillofacial area, possible toxic reactions, dental phobia, bleeding, hematomas and other pressing problems will recede into the background.
To directly implement effective and safe anesthesia, you basically need good tools, i.e. carpule injectors and carpule needles that would fit their threads and would be easy to use, a reliable anesthetic and, most importantly, knowledge, skills and some experience in performing various methods of local anesthesia.
According to the results of Russian studies, as well as foreign ones, ultracaine preparations fully satisfy modern requirements for a local anesthetic. Its only drawback is the absence in Russia of dosage forms without a vasoconstrictor; therefore, it cannot be used in those categories of patients (about 2-5% of patients) for whom a vasoconstrictor is contraindicated. It should be noted that before using it, you must read the section in the information insert on contraindications (mainly related to the presence of a vasoconstrictor), which is written in Russian. If the information insert for any drug is written in a language other than Russian, this means that this drug entered Russia illegally, and you may have problems with its use.
Dosage forms of local anesthetic drugs and carpule technology.
Not so long ago, the technology of local anesthesia included the preparation of local anesthetics by diluting concentrated solutions of local anesthetics and adding, if necessary, vasoconstrictors directly in the medical institution. In this regard, responsibility for ensuring the correct execution of all stages of preparing solutions fell entirely on the employees of the institution. As experience has shown, in most cases the preparation of solutions was carried out with errors and inaccuracies due to the lack of special equipment, which led to complications when injecting such solutions into patients.
The development of carpule technology is a revolutionary achievement in our specialty. The transfer of the production process of local anesthetics to factory conditions ensured sterility and high accuracy in compliance with all production technologies. By visiting some manufacturing companies, you can see that the modern process of producing anesthetics is fully automated and controlled at all stages, from water purification to the dilution of vasoconstrictors. Thanks to this, the dentist can be completely confident in the quality of the local anesthetics used.
The introduction of carpule technology also made it possible to transfer responsibility for the quality of drugs administered from the carpule to manufacturing companies.
In this case, the doctor only needs to comply with a number of mandatory conditions, which include the following:
- the local anesthetic drug must be approved for use by the Pharmacological Committee of the Ministry of Health of the Russian Federation;
- The delivery package must include a certificate of conformity for this batch of the drug, confirming its quality based on an examination. The lot number of the drugs is indicated on each package and carpul;
You can purchase local anesthetic drugs only if the seller has the following documents:
- license for pharmaceutical activities, which indicates his right to trade;
- registration certificate of the Ministry of Health of the Russian Federation for this dosage form, which gives the right for its clinical use in Russia;
- certificate of the State Standard of the Russian Federation, which gives the seller the right to import the specified drug.
In the absence of one of these documents, legal responsibility falls on the doctor and the institution where the complication occurred from the use of the drug.
Carpool technology.
Carpool technology consists of the following main components:
- standardization of dosage forms of local anesthetic drugs;
- factory production of drugs in a ready-to-use form, which includes both a standardized solution and standardized packaging;
- techniques for injecting drugs using special instruments (syringes, needles) and the order of their use.
When preparing drugs independently, both the composition and concentration of substances included in the solution could vary within significant limits. For the most effective and safe drugs based on articaine, there are currently only two dosage forms that differ in the concentration of the vasoconstrictor: a 4% solution of articaine with adrenaline at a concentration of 1:100,000 or 1:200,000. For safety and ease of use of the anesthetic, ultracaine carpules and packages are produced with clear color differences:
- green color – Ultracain DS with a vasoconstrictor concentration of 1:200000;
- blue color – Ultracain DS forte with a vasoconstrictor concentration of 1:100000.
In addition to a local anesthetic and a vasoconstrictor in certain concentrations, solutions in carpules also contain other components. As a filler, pyrogen-free distilled water is used with the addition of sodium chloride to create osmotic balance: the pH of solutions varies from 3.0 to 6.0. To prevent oxidation of the vasoconstrictor (adrenaline), an antioxidant is added - sodium bisulfite solution.
The presence of a vasoconstrictor and antioxidant reduces the pH of the solution. In addition, during long-term storage, sodium bisulfite is converted to sodium bisulfate due to oxidation, which is an additional factor in reducing pH. The lower the pH of the solution, the more likely the patient will experience a burning sensation when the drug is administered.
The doctor must know the composition and properties of the components included in the carpuled solution. A description of the contents of the carpules is indicated on the box or in the information leaflet. This information includes data on the percentage of the solution, the trade name of the drug, the batch number, the name and address of the manufacturer, and the presence of a preservative. When using the drug, special attention should be paid to the shelf life, avoiding the use of expired drugs.
To preserve anesthetic solutions, methylparaben is most often used, which has bacteriostatic, antifungal and antioxidant properties. However, it is a strong allergen. Recently, most companies have switched to new technologies that make it possible to produce carpuled solutions without methylparaben. The absence of parabens has significantly expanded the indications for the use of carpules. EDTA (ethylene diamine tetraacetic acid) is added to the solution of some anesthetics. This preservative is usually added to the solution to leach it out and to bind into an inactive form the heavy metal ions that enter the solution from low-quality carpool glass. This preservative itself is non-toxic.
It should be noted that carpuled forms of ultracaine do not contain methylparaben and EDTA; they contain only the minimum required amount of sodium bisulfite to maintain vasoconstrictor activity.
Basic indicators of anesthesia when working with articaine anesthetics.
When performing various types of anesthesia on the upper and lower jaw with modern articaine anesthetics, it is necessary to take into account a number of factors: type of anesthesia, recommended needles for anesthesia, recommended dose of anesthesia, latent period, duration of anesthesia in minutes, success of anesthesia, list of manipulations that can be performed under this anesthetic.
These indicators were obtained thanks to research in this area and the experience of specialists. The tables below give the standards recommended for the use of modern carpule anesthetics of the articaine series.
The main indicators of anesthesia when working with an articaine anesthetic on the upper jaw using infiltration anesthesia.
| Groups of teeth | Recommended cannula, diameter and length, mm | Amount of anesthetic in ml | Latent period in seconds | Duration of anesthesia, in minutes | Success of anesthesia, % |
| Incisors and canines | 0,3-0,4 length 25 | 0,4-0,5 | 60-70 | 20-25 | 97-99 |
| Premolars | 0,3-0,4 length 16-25 | 0,4-0,5 | 60-80 | 20-30 | 99 |
| Molars | 0,3-0,4 length 16-25 | 0,5-0,7 | 100-120 | 20-35 | 98-99 |
List of procedures: surgical intervention on soft tissues, preparation of hard tooth tissues for a crown, cystectomy, opening of subperiosteal abscesses, treatment of periodontitis and depulpation, removal of one or more teeth, resection of the apex of the tooth root, osteostomy, restoration, implantation surgery, as well as all dental interventions for sanitation of the oral cavity.
The main indicators of anesthesia when working with an articaine anesthetic on the lower jaw with mandibular anesthesia (premolars and molars) and infiltration anesthesia in patients under 50 years of age (incisors and canines).
| Groups of teeth | Recommended cannula, diameter and length, mm | Amount of anesthetic in ml | Latent period in seconds | Duration of anesthesia, in minutes | Success of anesthesia, % |
| Incisors and canines | 0,3-0,4 length 16-25 | 0,6 | 1,5 | 25-30 | 97-98 |
| Premolars | 0,4 length 42 | 1.7 (carpule) | 7,1 | 45-60 | 98 |
| Molars | 0,4 length 42 | 1.7 (carpule) | 6,7 | 45-60 | 98 |
List of procedures: surgical intervention on soft tissues, preparation of hard tooth tissues for a crown, cystectomy, opening of subperiosteal abscesses, treatment of periodontitis and depulpation, removal of one or more teeth, resection of the apex of the tooth root, osteostomy, restoration, implantation surgery, as well as all dental interventions for sanitation of the oral cavity.
The main indicators of anesthesia when working with an anesthetic of the articaine series on the upper and lower jaws when using intraligamentary anesthesia.
| Groups of teeth | Recommended cannula, diameter and length, mm | Amount of anesthetic in ml | Latent period in seconds | Duration of anesthesia, in minutes | Success of anesthesia, % |
| Incisors on the upper jaw | 0,3 length 10-12 | 0,12 | 30-40 | 18-27 | 80 |
| Incisors on the lower jaw | 0,3 length 10-12 | 0,12 | 30-40 | 18-27 | 90 |
| Fangs | 0,3 length 10-12 | 0,12 (1 injection) | 30-40 | 18-27 | 54 |
| Premolars | 0,3 length 10-12 | 0,18-0,24 (1 injection) | 30-40 | 18-27 | 93 |
| Molars on the upper jaw | 0,3 length 10-12 | 0,36 (3 injections) | 30-40 | 18-27 | 92 |
| Molars on the lower jaw | 0,3 length 10-12 | 0,24 (2 injections) | 30-40 | 18-27 | 92 |
List of procedures: treatment of caries and pulpitis, preparation of hard tooth tissues for a crown, tooth extraction for chronic periodontitis.
The main indicators of anesthesia when working with an anesthetic of the articaine series on the upper and lower jaws when using intrapulpal anesthesia.
| Groups of teeth | Recommended cannula, diameter and length, mm | Amount of anesthetic in ml | Latent period in seconds | Duration of anesthesia, in minutes | Success of anesthesia, % |
| Incisors | 0,4-0,5 length 16-25 | 0,2-0,3 | 15-30 | 10-30 | 95-96 |
| Fangs | 0,4-0,5 length 16-25 | 0,2-0,3 | 15-30 | 20-30 | 95-96 |
| Premolars | 0,4-0,5 length 16-25 | 0,2-0,3 (1 injection) | 15-30 | 20-30 | 95-96 |
| Molars | 0,4-0,5 length 16-25 | 0,2-0,3 (1 injection) | 15-30 | 20-30 | 95-96 |
List of procedures: depulpation and work with canals.
Conclusion.
After a detailed description of the most effective and safe methods of local anesthesia, I would like to dwell on an interesting observation. When surveying practicing dentists of various specialties: “What new things would you like to know in the field of local anesthesia?”, in most cases they were interested in information about new drugs. However, a new local anesthetic molecule appears once every 15-25 years, and a new dosage form of an old molecule appears once every 7-10 years. Currently, more than 100 drugs are used based on only 4-5 molecules (substances or active ingredients) with varying vasoconstrictor content.
The path to guaranteed and predictable anesthesia lies in increased attention and an individual approach to each individual patient, a thorough history taking, and the ability and willingness to provide the necessary emergency care measures. It is better to improve in methods and technologies of pain relief with the same drug from the articaine series, which is well known and studied, has a reliable carpule structure and a minimal amount of preservatives.
Bibliography:
- “Modern methods of pain relief based on articaine-containing drugs” S. A. Rabinovich, M. V. Lukyanov, O. N. Moskovets, E. V. Zoryan OID “Media Press” LLC
- “New in Dentistry” January 1999. Magazine.
- “Practical therapeutic dentistry” A. I. Nikolaev, L. M. Tsepov, Moscow, “MEDpress-inform” 2003.
- “Surgical Dentistry”, edited by T. G. Robustova, Moscow, “Medicine”, 2000.
10
Instruments for local anesthesia
The injection requires a syringe, a needle and a local anesthetic solution.
For several decades now, in dentistry, instead of disposable syringes, a reusable carpule syringe has been used. A disposable anesthetic cartridge and a disposable needle are inserted into it. They are used once, and the metal syringe itself is sterilized after each patient. Reuse of an incompletely used carpule is prohibited, since during the injection a reverse flow of blood or other liquid through the needle into the carpule is possible (there is a risk of infection of the next patient).
A special syringe gun is available for intraligamentary anesthesia. The same needles and carpules are inserted into it as into a carpule syringe. It allows you to more accurately dose the volume of anesthetic for a given type of anesthesia (but it is also possible to perform intraligamentary anesthesia with a regular carpule syringe).
The thickness of the needles used in carpule syringes is 0.3-0.5 mm. This is much thinner than disposable syringes (therefore the injection is much less painful). Length – 8-30 mm. For mandibular and torusal anesthesia, longer and thicker needles are used than for infiltration. To carry out intrapulpal and intraligamentary anesthesia, the needle can be bent (it does not break).
Carpula is a sealed glass cartridge with a rubber plunger. In dentistry, in most cases, the anesthetic solution, in addition to the anesthetic drug itself, contains a vasoconstrictor - a vasoconstrictor component that prevents the rapid elimination of the anesthetic through the general bloodstream. This is adrenaline (epinephrine). Its concentration is negligible - 1:100000 or 1:200000. When manually drawing such a mixture into a disposable syringe, add 1 drop of adrenaline to the anesthetic solution. However, the size of a drop is such a relative value that the concentration of this very active component can differ tens of times in different syringes. This creates many complications, even life-threatening situations for the patient.
The introduction of carpules with precise industrial dosages of components has greatly reduced the number of such complications. However, it should be noted that different manufacturers have different attitudes towards maintaining strict dosages of their own carpules. For the product of the Russian pharmaceutical industry, Brilocaine (manufacturer: Bryntsalovskiy Ferein), the anesthetic effect of two capsules from one package can be radically different: from complete absence of pain relief to super strong (“my legs froze,” according to the patient). Although the packaging states exactly the same ingredients as imported Ultracain, Ubistezin or Septanest.
Anesthetics with low vasoconstrictor dilution 1:200000
Indicated for most outpatient interventions in pediatric dentistry. 4% articaine 1:200000 provides anesthesia for soft tissues for 180 minutes and dental pulp for 45 minutes, which satisfies the protocol for most outpatient interventions.
Currently, anesthetics based on 4% articaine with epinephrine 1:400000 have appeared in European countries. They provide anesthesia for dental pulp tissue for 20 minutes and soft tissue for 1 hour. This anesthetic provides the duration of anesthesia required by the doctor and a short period of “numb” tissue, which is so important for pediatric patients. Currently, these anesthetics are not certified in the Russian Federation, but work is underway to introduce them into domestic dentistry.
It is also worth noting that there is no difference in the depth of anesthesia and effectiveness between anesthetics with vasoconstrictors 1:100000, 1:200000 and 1:400000. There is a difference only in the duration of local anesthesia of the dental pulp: 25, 45 and 75 minutes, respectively. Many dentists mistakenly divide anesthetics into “strong” (1:100,000) and “weak” (1:200,000). This statement is misleading.
For short-term interventions in children with concomitant pathologies, the use of anesthetics without a vasoconstrictor is indicated. However, their use does not guarantee complete safety and does not reduce the risk of complications. It is worth noting some of their pharmacological features. Vasoconstrictors are added to the local anesthetic solution not only to increase the duration of pain relief, but also to reduce their toxicity. The fact is that all anesthetics have a vasodilating effect and undergo fairly rapid absorption into the bloodstream. The addition of a vasoconstrictor slows the absorption of the anesthetic and prolongs its action. When using an anesthetic without vasoconstrictors, this effect does not occur. The anesthetic is forced into the blood, which can lead to a toxic reaction. This complication is possible if the permissible dosage is exceeded, which is different for anesthetics with and without a vasoconstrictor. In summary, it should be noted that anesthetics without a vasoconstrictor do not affect the functioning of the cardiovascular system, are less allergenic since they do not contain preservatives, but due to accelerated absorption they are toxic and safe to use only if the dosage is observed.
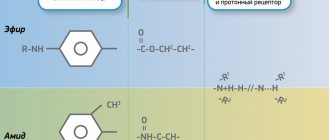
Local anesthetics
In Russia, 4 types of anesthetics are most widely used: novocaine, lidocaine, articaine and mepivacaine.
Novocaine (procaine) was synthesized in 1905 and became widespread throughout the world as the first non-narcotic anesthetic. It is a basic reference point - all subsequent anesthetics are compared in terms of effectiveness and toxicity with novocaine, whose indicators are taken as one. After the introduction of lidocaine, it lost popularity in developed countries. There is a high frequency of allergic reactions to novocaine.
Lidocaine was invented in 1943. Its effectiveness turned out to be 4 times higher than that of novocaine (with only twice the toxicity). Widely distributed throughout the world (1st place in the number of injections among anesthetics in the USA). However, like novocaine, it has a relatively high percentage of allergic reactions (including the development of anaphylactic shock). In addition, it is often used with increased concentrations of the vasoconstrictor 1:50000 and 1:25000, which increases its effectiveness, but increases the number of complications from the cardiovascular system. Indicated for pregnant women - FDA category B (see article Use of local anesthetics for dental treatment during pregnancy; safety for women in labor).
Articaine was synthesized in 1969. It began to be used in Germany, where it was registered under the commercial name "Ultracaine". This name of the drug is now no less popular than articaine, although it represents the product of only one, “Septanest”, “Alfacaine” and several other commercial names - this is the same as “Ultracaine”. The most common local anesthetic in Europe and Russia (it was approved in the USA only in 2000, 10 years later than here). 5 times more effective than novocaine. 1.5 times more toxic. According to the FDA classification, it is classified as category C.
Mepivacaine was developed in 1957. It is equivalent in effectiveness to lidocaine and inferior to articaine. It is noteworthy that, despite category C, it is often used for pregnant patients, due to the permission of non-adrenaline release forms (lidocaine and articaine carpules are sold only with a vasoconstrictor). Although in fact it is not the first choice drug for expectant mothers (see the article Is it possible to do local anesthesia during pregnancy?).
Adrenaline , also known as epinephrine, is not a local anesthetic, but is used in the vast majority of cases for dental injections. By narrowing the blood vessels, it helps preserve the anesthetic depot at the injection site, reduces its toxic effect on the body, and also reduces bleeding (which improves visibility during surgical procedures). Its use in pregnant women and patients with cardiovascular diseases (paroxysmal ventricular tachycardia, atrial fibrillation) is undesirable. Use with caution in patients with arterial hypertension, diabetes mellitus, and hyperthyroidism.
In addition to the anesthetic and vasoconstrictor, the solution may contain preservatives (methylparaben) and adrenaline stabilizers (sodium pyrosulfite). Both methylparaben and sodium pyrosulfite (metabisulfite) have a high frequency of allergic reactions, including the most dangerous - anaphylactic shock. This risk is significantly higher than that of the anesthetics themselves (and in principle there cannot be an allergic reaction to adrenaline). Therefore, methylparaben was completely abandoned in carpules - it is needed only when using large containers for preserving an unused solution after opening the ampoule. Sulfites are necessary to prevent the oxidation of adrenaline - they cannot be abandoned in carpules with a vasoconstrictor. Therefore, anesthesia without adrenaline is recommended for patients with multivalent allergies. The frequency (up to 5%) of sulfites provoking an attack of bronchial asthma is high, so anesthesia with adrenaline is also not recommended for asthmatics.
Types of infiltration anesthesia
- Straight. The area of tissue where the anesthetic was directly injected loses sensitivity.
- Indirect. The drug disperses throughout the surrounding tissues and has an analgesic effect on a wider area.
Drugs used
For infiltration anesthesia, special drugs are used in low concentrations. These include:
- Lidocaine.
- Novocaine.
- Procaine.
- Ultracaine.
More effective, but also more toxic anesthetic drugs include:
- Bupivacaine.
- Tetracaine.
- Ropivacaine.
Adrenaline can be used to enhance the effect of the painkiller. It promotes vasoconstriction and prevents the anesthetic from entering the blood.
When infiltrating anesthesia, specialists adhere to the principle of using sufficiently large volumes of solutions with low concentrations. This makes pain relief safe for the patient. For anesthesia, a 0.25-0.5% solution is diluted with novocaine or lidocaine. This concentration allows you to administer up to 400 ml of the product.
Local anesthesia in pediatric dentistry
Local anesthesia is not recommended for young children under 2-4 years of age. Even if it is possible to fraudulently persuade a child to take an injection, after it, as a rule, he will no longer open his mouth for further treatment. Up to 6-7 years of age, the optimal method is infiltration anesthesia (including for the treatment of lower teeth). At this age, the lower jaw is not yet so dense and there is no need for conduction anesthesia. Of the drugs for children, the optimal choice would be articaine with a low adrenaline content of 1:200000 - since long-term manipulations are still contraindicated for children (they quickly get tired of the treatment), there is no need for long-term pain relief for many hours.
Features of pain relief for permanent teeth
Treatment of permanent teeth in children certainly requires pain relief. The choice of pain relief method depends primarily on the child’s age and degree of development. Difficulties in pain relief usually arise in the treatment of mandibular molars, which is due to varying degrees of development of the cortical layer of the bones of the facial skeleton. In most cases, when treating uncomplicated caries of permanent teeth of the lower jaw in children under 12 years of age, infiltration anesthesia is sufficient. In children over 12 years of age, infiltration anesthesia is effective only in the area of incisors and premolars.
To treat the canines of the lower jaw in children over 12 years of age, mandibular anesthesia or mental anesthesia should be performed, the volume of injected anesthetic is 0.6-1 ml. For the treatment of first molars with short-duration interventions (15-20 minutes), infiltration buccal anesthesia is effective, with the volume of injected anesthetic being 0.6-1 ml. Infiltration anesthesia of the second molars of the lower jaw is not so effective; in most cases, complete anesthesia of the pulp tissue is possible only with the use of conductive mandibular anesthesia.
There are some peculiarities in conducting conduction methods of anesthesia of the lower jaw. First of all, their implementation must be justified from the point of view of nosology and the method of treatment chosen by the doctor. If possible, conduction methods of anesthesia should be avoided and preference should be given to safer infiltration techniques.
There are studies confirming that the diameter of the needle does not affect the reduction in the degree of pain of the anesthesia.
Mandibular anesthesia in children of different ages is carried out according to different intraoral landmarks. This is due to the different position of the mandibular foramen in relation to the occlusal plane of the teeth.
In children under 6 years of age, the mandibular foramen is located below the occlusal surface, so the needle is inserted at the level of the occlusal surface. Accordingly, in children 6-10 years old, the needle is inserted 5 mm above the occlusal surface, and only in children over 10 years old, mandibular anesthesia is carried out by analogy with adults. When performing mandibular anesthesia, an aspiration test should be performed in all cases to reduce the risk of intravascular injection of anesthetic. The anesthetic should be administered slowly.
Mental anesthesia is carried out taking into account the period of development of the dental system. Compared to adults, the mental foramen in children is located significantly anteriorly: in children under 4 years old - in the area of temporary canines, in children 4-6 years old - in the area of the first temporary molar.
Other methods of pain relief. In addition to conduction and infiltration methods of pain relief, which have already become traditional, periodontal and intraosseous techniques are now becoming increasingly widespread in dentistry. However, the question of the safety of their use remains open. In particular, when performing intraligamentary anesthesia, the distribution of the anesthetic passes through the cancellous substance of the jaw bones, reaching the periapical region. The vasoconstrictor has a long-term vasoconstrictor effect (Brannstrom M., Lindskog S., Nordenvall KJ, 1984; Tagger E., Tagger M., Sarnat H. 1994), the safety of which has not been studied for teeth during their formation.
Intraosseous anesthesia is not indicated for use in pediatric dentistry. There is a danger of injury to the tooth buds and the negative impact of the vasoconstrictor on the growth zones of periapical tissues. Also, the vibration and noise of the intraosseous injector can frighten the child or, even worse, provoke sudden movements that can lead to injury from the rotating elements. The author does not recommend intraosseous anesthesia in pediatric practice, although there are studies in the literature about their “highest” effectiveness in children (Sixou JL, Rogier ME, 2006).
If possible, conduction methods of anesthesia should be avoided and preference should be given to safer infiltration techniques.
However, the above methods cannot be completely denied in the treatment of permanent teeth with formed apices. In particular, the effectiveness of intraseptal, intraosseous and intraligamentary anesthesia in the treatment of mandibular molars is high (Medvedev D.V., Petrikas A.Zh., Tazova O.E., 2010; Petrikas A.Zh., Yakupova L.A., Medvedev D.V., 2010).
These techniques can be used as an independent method of pain relief for short interventions lasting 15-20 minutes. They can also be used additionally if the initial anesthesia is insufficient: treatment of acute pulpitis of the mandibular molars (Anisimova E.N., Rabinovich S.A., Butaeva N.T., 2013; Makeeva I.M., Erokhin A.I., Kuzin A.V., 2012), incorrect choice of anesthetic, the effect of which has expired.
The effectiveness of local anesthesia
The success of deep anesthesia depends on the anesthetic, the concentration of the vasoconstrictor, the type of anesthesia, the dose of the drug, the qualifications of the dentist and the individual response of the patient. 4% articaine with an adrenaline concentration of 1:100000 is the most effective. Conduction anesthesia provides better pain relief than infiltration anesthesia, but requires a more highly qualified doctor. (However, even the most experienced specialists have a certain percentage of failures). The patient's agitated panic state and prolonged pain tolerance for several days before the visit reduce the effectiveness of local anesthesia. Alcohol and drugs - even more so.
Technology of infiltration anesthesia behavior
- First, the area where the drug is administered is treated with an antiseptic.
- The doctor takes a comfortable position near the patient (on his right side).
- The doctor exposes the working area of the mouth by pulling back the cheek or lip. This action can be performed by hand or with a special tool.
- The specialist places the tip of the needle on the transitional fold, maintaining an inclination angle of 45° (relative to the alveolar ridge). The cut of the needle should be directed towards the jawbone.
- Next, the doctor carefully inserts the needle until it touches the bone tissue. The immersion depth can be 5-15 mm, depending on the jaw area.
- The anesthetic is smoothly injected from a syringe into the tissues of the oral cavity.
Dosage
The volume of one carpule is 1.7-1.8 ml. This amount is enough for most manipulations within one or two teeth. When treating a larger number of teeth (especially if they are located far from each other), several carpules and injections into different parts of the oral cavity are required.
A second injection of anesthetic into the same place is carried out if the first one is unsuccessful or after some time, when long-term treatment has not yet been completed and the anesthesia begins to wear off. The introduction of the same drug can help if conduction anesthesia is ineffective the first time. With other types of anesthesia, it is necessary to change the anesthetic itself to a more powerful one. It is impossible to increase the volume of the injected solution indefinitely - in case of an overdose, a toxic reaction occurs. For articaine with adrenaline and lidocaine with adrenaline, the maximum dose is 7 mg/kg body weight. One carpule (1.7-1.8 ml) contains 34-36 mg of 2% lidocaine or 68-72 mg of 4% articaine. Therefore, for a person weighing 70 kg, the maximum number of carpules at one time is: 14 for 2% lidocaine and 7 for 4% articaine.
Features of pain relief for temporary teeth
Of course, the choice of pain relief method depends on the planned intervention.
In the treatment of caries and pulpitis of temporary teeth, preference is given to infiltration methods carried out from the vestibular (buccal/labial) side, and there is no need for lingual or palatal anesthesia. This is explained by the predominance of spongy substance and a large number of nutrient openings in the structure of the jaw bones, facilitating the diffusion of local anesthetic.
In order to reduce the degree of pain of the injection and increase the level of comfort for the child, the following recommendations for local anesthesia should be followed:
- A preliminary distracting preparatory conversation with the child is necessary, during which the doctor uses terms that the child understands. In this case, the words “injection”, “syringe”, “anesthesia”, “removal”, “needle” are not pronounced.
- The child should not see (look at) the injection equipment. All instruments are presented by an assistant out of sight of the child.
- Application anesthesia should be performed so that the child does not feel the puncture stage of the mucous membrane.
- The rule must be observed: “one needle, one injection.” If the needle accidentally comes into contact with the bone tissue of the jaw, its tip is deformed; as a rule, it bends in the direction opposite to the bevel. A repeated injection with the same “dull” needle in another segment will involve applying pressure that is unpleasant for the child.
- The anesthetic should be injected slowly, 1 ml/min. Forced administration of the anesthetic leads to hydrodynamic tissue trauma, which causes pain.
- Two-stage injection of a portion of anesthetic. When performing infiltration anesthesia, the doctor initially injects a small amount of anesthetic? 0.1 submucosally, while a zone of tissue infiltration the size of a millet grain is visually determined. Next, the doctor talks with the child for 2-3 minutes.
- The subsequent administration of the main portion of the anesthetic is painless.
- The temperature of the anesthetic solution should be close to the child’s body temperature. To do this, do not store anesthetic carpules in the refrigerator. Before the injection, the doctor can “warm” the carpule in his hand or in running hot water.
The volume of injected anesthetic for infiltration anesthesia of temporary incisors and canines is on average 0.3 ml; for anesthesia of temporary molars, 0.5-0.6 ml is used. Subperiosteal anesthesia should not be performed as this will cause pain to the child and will not increase effectiveness. The needle should move submucosally towards the apexes of the roots of the teeth. In the upper jaw, when performing infiltration anesthesia, one should not insert a needle into the area of the frenulum of the upper lip, mucous strands in the area of temporary canines. These areas have an extensive network of nerves, providing hypersensitivity in these areas.
When performing an operation to remove temporary teeth of the upper jaw with a diagnosis of periodontitis, various combinations of infiltration methods are used. In the upper jaw, when removing incisors and canines, infiltration vestibular (0.5 ml) and incisal anesthesia (less than 0.2 ml) is used. In this case, classical conduction anesthesia with the advancement of the needle into the incisive canal is not carried out, but a certain amount of anesthetic is injected on the side of the incisive papilla, until signs of ischemia appear. If possible, painful incisal anesthesia should be avoided, which can be replaced with topical anesthesia or by inserting a needle into the vestibular interdental papilla and then moving it to the palatal side with a continuous supply of anesthetic.
The choice of dilution of the vasoconstrictor depends on the expected duration of the intervention and the presence of concomitant pathology in the child. As a rule, the duration of treatment for a child does not exceed 20-30 minutes.
When anesthetizing the first and second temporary molars, infiltration vestibular (0.5-0.6 ml) and palatal (0.2 ml) anesthesia is used. Palatal anesthesia can be replaced by the above-described approach through the interdental papilla. To reduce the degree of pain of local anesthetic injection into the hard palate, preliminary application anesthesia should be used.
When removing temporary teeth of the lower jaw with a diagnosis of periodontitis, a combination of conduction and infiltration methods is used. When removing incisors and canines, infiltration vestibular (0.3 ml) and lingual (less than 0.2 ml) anesthesia is used. Lingual infiltration anesthesia is performed in the area of the transition of the attached gum to the mobile mucosa of the floor of the mouth. The anesthetic is injected into the submucosal layer; the needle is not advanced to prevent intravascular injection. You can anesthetize the lingual mucosa by inserting a needle into the interdental papilla from the vestibular side and then moving it towards the lingual mucosa. When removing temporary first molars of the lower jaw, the above-described technique is used with the only difference that 0.5 ml of anesthetic is injected from the vestibular side of the tooth being removed. In the presence of local inflammation, it is necessary to perform conduction mental anesthesia. When removing the second temporary molars of the lower jaw with a diagnosis of periodontitis, either mandibular anesthesia (1 ml) or a combination of mental anesthesia (0.6 ml) and lingual infiltration (0.2 ml) is performed.
During the period of physiological change in occlusion, the removal of temporary teeth for orthodontic indications has some features. The most common mistake is removing a “moving” tooth under application anesthesia. The depth of application anesthesia is 2-3 mm of the mucous membrane, and the roots of the tooth may not be completely resorbed, and their removal will be painful. Application anesthesia can be used as an independent method only if the tooth is fixed by mucous membrane on one edge. In other cases, infiltration anesthesia should be performed. The anesthetic is administered before signs of gum ischemia appear; its volume is minimal.
Coming time
Intrapulpal and intraligamentary anesthesia begins to take effect within a few seconds. Application, infiltration, intraosseous - after 1-5 minutes. Conduction anesthesia is the most variable - from instant pain relief at the same second (if the needle hits the nerve) to half an hour. Sometimes patients, rising from the dental chair after completion of treatment, claim that “only now the freezing has really taken hold.”
Soft tissues are anesthetized before teeth. If the lip or tongue is already “frozen,” the teeth may still remain sensitive, and their premature preparation will be painful.
Operating principle of infiltration anesthesia
Infiltration anesthesia is one of the methods of pain relief.
It involves the introduction of an anesthetic into the skin or mucous membrane, as a result of which nerve impulses are blocked. This type of pain relief is known as “freezing.” The drug used by the doctor suppresses the nerve impulse that goes from the pulp to the brain. Therefore, the patient loses sensation in some parts of the face or mouth, such as the cheek, lip or tongue. Numbness occurs in the part of the face where the anesthetic is injected. The anesthetic is administered by injection. First, the drug enters a certain area under the skin, and then is distributed among the cells. The maximum duration of the anesthetic dose is one hour. Gradually the medication breaks down and sensitivity returns. If necessary, another dose of the drug may be administered. The anesthesia process is under the supervision of a specialist.
Distinctive features of infiltration anesthesia
Infiltration anesthesia differs from other methods of pain relief by its immediate action and the exact duration of the analgesic effect. The components of the drug are very quickly eliminated from the body and do not have a negative effect on it. Infiltration anesthesia is also characterized by a low concentration of medications used.
Indications for the use of infiltration anesthesia in dentistry
- Treatment of dental diseases (caries, pulpitis, periodontal inflammation).
- Surgical treatment of periodontal diseases (curettage, gum plastic surgery, elimination of defects and tissue regeneration).
- Dental prosthetics without pulp removal (installation of crowns, inlays, bridge structures).
- Treatment with surgical intervention (tooth extraction, implantation, tissue expansion, emptying of purulent cavities, opening of phlegmons, excision of cysts).
Contraindications
- An allergic reaction to a pain reliever.
- Mental disorders of the patient that prevent constructive communication with him.
- Excessive psychomotor agitation.
- Children under 10 years of age (relative contraindication).
- Asthma and other pathologies of the respiratory system.
- Using muscle relaxants to relax muscles.
- The presence of scars on the mucous membranes of the oral cavity, which prevent the uniform distribution of the drug.
- Inflammatory or purulent process in the area of anesthetic administration.
- The presence of malignant neoplasms or tumors suspected of cancer.
- Refusal of the patient to use this method of anesthesia.
Validity
The duration of anesthesia also depends on the anesthetic, the concentration of the vasoconstrictor, the type of anesthesia, the dose of the drug, the qualifications of the dentist and the individual response of the patient. Conduction anesthesia lasts up to 2-3 hours or more. Some patients note that the anesthesia wears off completely only in the evening (if the treatment was carried out in the morning). But this is with a strong anesthetic, a high concentration of adrenaline, a significant dosage, and close contact with the nerve trunk. In other situations, conduction anesthesia may not last even one hour. Infiltration anesthesia lasts 1 hour or less. Other types are even smaller.
Advantages of infiltration anesthesia
- This type of anesthesia is safe, as it allows the use of solutions in low concentrations.
- The effect of infiltration anesthesia is much faster than conduction anesthesia.
- The area where the anesthetic is administered loses sensation for a long period of time.
- It is possible to administer an additional dose of the drug if long-term treatment is necessary.
- The anesthetic drug is very easily eliminated from the body in a short time.
- Loss of sensation occurs not only in the nerve into which the anesthetic was injected, but also in neighboring nerves.