The influence of swallowing function on the formation of the dental system
Swallowing is a complex set of motor reactions that move food from the mouth through the esophagus to the stomach. The swallowing reflex is innate. Normally, 22 muscles of the maxillofacial region, sublingual region and pharynx take part in the act of swallowing. A child is born with a well-developed swallowing mechanism, which in the first months is called infantile. Due to the contraction of the muscles of the lips, cheeks, and tongue, when sucking, negative pressure is created in the baby’s mouth and milk enters the mouth, and the tongue, located between the toothless gingival ridges, directs the milk into the oropharynx. Before the first teeth erupt, this infantile type of swallowing, in which the tongue rests on the lips, is the physiological norm. But as baby teeth erupt, sucking is replaced by chewing, and the child’s type of swallowing changes to somatic: during somatic swallowing, the tongue is located in the anterior third of the hard palate, while the back of the tongue pushes food into the larynx.
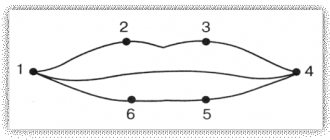
If we analyze in more detail the biomechanics of this process, the act of swallowing as a whole consists of two phases: first, with movements of the tongue, food is delivered to the cutting surface of the teeth, where it is mixed with saliva, then, with contraction of the muscles of the floor of the mouth (hyoid bone, larynx and back of the tongue), it is pressed , rising from front to back to the hard and soft palate, pushing it towards the pharynx. The first phase of swallowing is voluntary and is associated with the action of the tongue and the muscles of the floor of the mouth. Once food passes the throat, swallowing becomes involuntary. The first phase of swallowing takes 0.7-1 s, and the second (passage of food through the esophagus) - from 4-6 to 8 s.
It is important to note that during the correct act of swallowing, the tip of the tongue should normally rest against the anterior third of the hard palate. If a child constantly consumes liquid or semi-liquid food, despite the presence of teeth, then a full act of chewing is not formed, and the transition from the infantile type of swallowing to the somatic one does not occur. At the moment of swallowing, a child with an infantile type of swallowing places his tongue between the upper and lower rows of teeth, which contributes to the formation of an open bite. In this case, the perioral muscles are involved in the act of swallowing, i.e. the lower part of the orbicularis oris muscle, the mentalis muscle and the neck muscles noticeably tense, which is easy to detect by asking the child to swallow saliva.
With the infantile type of swallowing, the child’s tongue gets used to only the simplest movements, so the lingual muscle develops poorly. As a result, macroglossia is often mistakenly diagnosed, while the child’s tongue is simply not sufficiently developed and mobile. Improper swallowing is very often combined with oral or mixed breathing. That is why the problem of correcting myofunctional disorders in such children is especially acute. If swallowing function is impaired, a specific treatment plan is outlined. First you need to teach your child to swallow correctly.
Exercises to normalize the function of swallowing Sitting in front of a mirror, keep your head straight, shoulders slightly back and slightly lowered, chest out, stomach tucked, knees bent, legs and heels together. The exercises are performed at a slow pace on a count of 1-2-3-4 and repeated 10 to 15 times daily. Exercise 1. Half-open your mouth, lick your upper and lower lips, running your tongue from one corner of your mouth to the other. Try to reach the nasal septum and chin with your tongue. Run the tip of your tongue along the lingual and then along the vestibular surface of the teeth, as if counting them, click your tongue, to do this, suck your tongue with your lips closed to the hard palate, and, slowly opening your mouth, rest the tip of your tongue on one or the other cheek. Exercise 2. Place the rubber ring from the pipette on the tip of the tongue, lift the tongue up and press it to the anterior part of the hard palate in the area of the palatine folds. Clench your teeth without closing your lips, swallow saliva without changing the position of the tip of your tongue and the rubber ring. Repeat the exercise 5-10 times 3 times a day. Perform the same exercise not with a ring, but with water, which must be swallowed. Exercise 3. Raise the tongue up and place it at the anterior part of the hard palate, then move it along the arch of the hard palate in the anterior part and as far back as possible to the soft palate. Exercise 4. Click your tongue, imitating the sound of a horse's hooves. Perform 50-60 times. Exercise 5. Clench your teeth, close your lips, rest the tip of your tongue on the hard palate - in the projection of the roots of the central incisors, swallow saliva. A trainer is very effective for correcting infantile swallowing. With each swallowing movement, the tongue of the apparatus reflexively reminds the child of the correct position of the tip of the tongue, which is reinforced during night wear and contributes to the restructuring of the infantile type of swallowing into the somatic one.
The use of myofunctional preventive trainers for the correction of swallowing and breathing dysfunctions in children in mixed dentition. Long-term disruption of nasal breathing in childhood not only negatively affects the development of the chest skeleton, but also leads to deformation of the facial skeleton: the upper jaw develops incorrectly, its lateral parts come closer together, the hard palate becomes narrow and high. As a result, the upper dentition narrows, causing crowding of the upper and then lower jaw teeth. In addition, in children with mouth breathing, the viscosity of saliva increases, oral hygiene deteriorates, which leads to the development of acute caries and periodontal inflammation. This problem, caused by the consequences of mouth breathing in children, is very common in the practice of pediatric dentists. Normalizing nasal breathing is only possible through comprehensive treatment from a pediatrician, otolaryngologist and orthodontist or pediatric dentist.
A few words about the physiology of the process. The air inhaled through the nose, passing through the nasal passages, undergoes a number of significant changes. It is moistened, warmed, cleaned, and disinfected. However, there are a number of conditions when breathing through the nose is difficult. This happens if catarrhal or hypertrophic processes occur in the nasal cavity. It is noted that the number of microorganisms penetrating into the lower respiratory tract with proper nasal breathing is reduced by 10 times compared to their number with oral breathing. Therefore, impaired nasal breathing contributes to sore throat, acute respiratory diseases, bronchitis, and pneumonia. Free nasal breathing is necessary for normal gas exchange in the blood, since when breathing through the mouth, the amount of oxygen entering the human body is only 78% of its normal volume. A prolonged lack of oxygen in the body can contribute to the development of anemia. The blood and lymphatic vessels of the nose are closely connected with the vessels of the brain, and therefore, with prolonged difficulty breathing, both in the nasal cavity and in the brain tissue, blood circulation is disrupted.
Normalizing nasal breathing most often prevents the growth of adenoid tissue, which is why many children undergo surgery. But does adenectomy lead to complete restoration of nasal breathing? We decided to answer this question by treating orthodontic disorders accompanied by oral breathing using silicone trainers - so-called trainers, intended for the treatment of children of both preschool and primary school age suffering from malocclusions, bad habits, and impaired nasal breathing.
We examined 222 children aged 6-8 years. Control examinations of children were carried out once every 3 months. It was recommended to wear the preorthodontic trainer 1 hour a day for active myotraining and put it on at night. Children with nasal breathing dysfunction were additionally offered breathing exercises. Parents were given detailed instructions on the use of this technique. The treatment plan using a trainer was determined for each child individually, depending on his psycho-emotional status. In addition, all children were trained in rational oral hygiene, the status of which was recorded during each examination using the OHI-S index. The acid resistance of enamel was determined by the TER test on a ten-point scale (from 10 to 100%). All research data are statistically substantiated and reliable.
During the initial examination, 87 children out of 222 examined showed mouth breathing, 81 had infantile swallowing, and 54 children had concomitant pathology. In almost all children, the hygiene index ONI-S at the initial examination was 2.4 (low level), and the test for enamel resistance was close to 72%, which indicates a low level of enamel resistance. In 43 patients with infantile swallowing, correction was performed using a pre-orthodontic trainer. After 6 months after the start of treatment, function returned to normal in 51% of children. After 12 months Correct swallowing was achieved in 30% of children who used a myofunctional trainer for correction.
For comparison, the remaining 38 patients observed with swallowing dysfunction were prescribed a course of myogymnastics. What is significant is that these children did not experience significant changes during the year.
Of the 87 patients with habitual mouth breathing, 42 used a preorthodontic trainer to correct dysfunction, and after 6 months. approximately half of these children learned to breathe through their nose. A year later, the function returned to normal in 80% of children who used a trainer for correction, while in 45 patients with the same pathology who did not wear a trainer but performed breathing exercises for the same time, there was no practical improvement.
In children with concomitant pathology (simultaneous dysfunction of swallowing and breathing), who wore the trainer for a year, objective signs significantly improved, but complete elimination of dysfunction occurred only in 30% of patients. In such children, it is necessary to first normalize nasal breathing and only then devote time to restoring swallowing function. The period of adaptation to the trainer for this group lasted almost 2 times longer. Children with concomitant pathology who did not use the device did not experience any improvement over the course of a year. All children with concomitant pathology were recommended breathing exercises and given an additional course of myogymnastics.
Based on the results of the study, the following conclusions can be drawn. 1. The use of a preorthodontic trainer has high clinical effectiveness and contributes to the successful correction of breathing and swallowing dysfunctions in children in mixed dentition. 2. Correction of myofunctional influences in the pre-orthodontic period can be carried out by pediatric specialists (dentists and pediatricians, speech therapists) in combination with breathing exercises and myogymnastics.
Compiled by a pediatric dentist, Ph.D. honey. Sciences E.A. Satygo (St. Petersburg).