| Way | Detailed description |
| Surgical method or extracapsular removal | The classic method of tonsil removal, which until recently was used throughout the world. The doctor uses a scalpel and wire thread. The tonsils are excised entirely, leaving difficult-to-heal wounds. Very long rehabilitation. Currently, the method is used in rare cases, for example, when there are contraindications for other methods or there is simply no necessary equipment. |
| IR laser or thermal welding | The tonsils are still excised, but this time with a powerful infrared laser (IR laser). The bottom line is that the laser hits the target and does not heat neighboring tissues. At the site of dissection, immediate tissue adhesion occurs, which entails minor blood loss and more comfortable rehabilitation. |
| Electrocoagulation | The electrical method is used quite rarely, as unpleasant consequences are possible. The excision takes place under the influence of high-frequency current, while the blood vessels are instantly sealed, and blood loss is minimal. However, electrocoagulation produces extremely high temperatures, and adjacent tissue may suffer thermal burns. |
| Carbon dioxide laser | An original method in which the tonsils simply evaporate (evaporate) under the influence of a laser. The tonsils can be reduced or removed completely. With this method, blood loss is insignificant, and recovery is comfortable. |
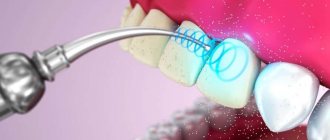
| Ultrasonic removal | A laser is used again, which many doctors call an ultrasonic scalpel. In this case, the tonsils are exposed to high-frequency ultrasound (over 26 kHz), which is like a sharp scalpel. Damaged vessels are sealed (coagulated). Recovery after the procedure is quite fast. |
| Cryodestruction | The tonsils are not excised using this method. Liquid nitrogen is used, which completely freezes the lymphoid tissue. The procedure itself is painless, but the rejection of frozen tissue occurs over time and is quite unpleasant. There is a possibility of repeating the procedure. |
| Microdebrider | Not the most humane type of procedure. Excision occurs with a special device (microdebrider), on the head of which sharp blades are placed. Rotating at great speed, they cut off the tonsil. Partial excision is possible. The recovery is quite long. |
Safe and least traumatic methods are thermal welding, coblation and electrocoagulation. This is due to the almost complete absence of blood during the operation and subsequent problem-free healing. However, laser-based methods are not used if the child is under 10 years old. It is extremely difficult for a child of this age to sit still, which can cause serious burns to the healthy tissues of the pharynx.
Any method of tonsillectomy is not complicated; doctors have long honed such skills and techniques. The procedure itself usually takes no more than one and a half hours. The pain is treated with local anesthesia, and in extremely rare cases with general anesthesia.
The most difficult moment of the entire operation is associated with the child himself. Complete immobility is required; for this, parents can be invited to the procedure. You need to try to calm the baby down and explain that there is nothing wrong with this - the procedure is completely painless.
A correctly performed procedure does not negatively affect the child’s health. Problems can arise if healthy tonsils are removed, as they are an important part of the body's defenses. But if the tonsils themselves are a source of infection, it is hardly worth refusing the operation. If tonsillectomy does occur, during the recovery period after surgery, Imudon® helps protect against infections2.
Imudon® is the only* local immunostimulant in the form of lozenges. A detailed regimen of use is presented in the instructions for the drug.
Symptoms of inflammation of the tonsils
Inflammation of the tonsils is accompanied by the following symptoms:
- Sore throat that gets worse when swallowing;
- Inflammation of the tonsils is observed on one or both sides - they become swollen and change color to dark crimson, white plaque and ulcers may appear;
- Body temperature rises. However, it is not always high and can only be observed in the evening;
- The person experiences weakness and headache, similar to the usual pain associated with colds;
- In advanced cases, a skin rash or exacerbation of other chronic diseases may appear;
- In the absence of timely treatment, inflammation of the tonsils provokes disruptions in the functioning of the heart and kidneys.
When is surgery needed?
In the recent Soviet past, removal of adenoids was a completely ordinary operation. And in America, almost all children under six years of age had their adenoids (or tonsils) removed. Nowadays, adenoid removal is performed much less frequently, because such an operation is associated with a number of unpleasant consequences for the body.
Modern doctors recommend removing tonsils only in a few cases:
- If a person gets tonsillitis (acute inflammation of the tonsils) more than four times a year, and the disease occurs with high fever and general weakness of the body.
- The occurrence of chronic tonsillitis against the background of constant tonsillitis (irreversible changes in the functioning of the tonsils and their constant inflammation.)
- The development of purulent abscesses (ulcers) against the background of this disease affecting the larynx area.
- When there is an unconscious closure of the airways by large tonsils (snoring during sleep, which causes short-term cessation of breathing).
- A sharp weakening of the immune system.
Chronic tonsillitis, which is one of the main reasons for surgery to remove tonsils, is a pathological condition of the body. The natural functions of the tonsils to protect against infections are lost during such a disease, and the tonsils themselves become the focus of inflammatory processes.
Progressive chronic tonsillitis can provoke diseases of the heart, joints and disrupt all the body's defenses. It can also cause rheumatism and severe kidney disease.
But early tonsillitis can be easily treated with conservative methods (washing, lubrication, physiotherapeutic procedures, etc.). If treatment for chronic tonsillitis fails, the inflammatory process goes too far and the damaged tonsils no longer contain healthy lymphoid tissue.
In this case, doctors recommend surgery. An operation to completely or partially remove the palatine adenoids is called tonsillotomy.
How to treat inflamed tonsils?
The presence of a simple sore throat is not an indication for tonsil removal! There are many treatment methods that avoid invasive intervention:
- Antibiotics. It would not be amiss to remind you that the course of antibiotics must be taken completely in accordance with the doctor’s recommendations, without skipping a single dose of medication and without abandoning treatment at any stage.
- Washing with various agents with an antibacterial effect. You may even be prescribed a simple solution of chlorhexidine, which will definitely not cause harm, but may well be a good medicine.
- Application of special solutions. This could be Lugol's solution or propolis - the doctor prescribes one or the other based on your individual characteristics.
- Physiotherapy. Ultrasound, magnets, electrophoresis - all this can be a completely sufficient method of treatment without any surgery.
- Maintaining a healthy lifestyle, strengthening the immune system and avoiding hypothermia, although not a treatment method, is an excellent method of preventive intervention in the development of severe pathologies.
You can also read our article on the treatment of chronic tonsillitis.
What are tonsils and why are they needed?
Tonsils are connective lymphoid tissue, which is entirely permeated with lymphocytes and cells, which are the main and important part of the body’s immune system (macrophages). There are six tonsils in our body: pharyngeal, palatine, lingual and tubal.
The palatine tonsils also have a hematopoietic function; in the accumulations of lymphoid tissue, lymphocytes (white blood cells) are formed, which are the main basis of immunity. The most important part of our immune system is the tonsils, the removal of which does not have a very good effect on the body as a whole.
Experts say that tonsils (or adenoids) are so important to the body that even a half-dead and collapsed tonsil produces more immunoglobulin than the rest of the immune system.
Due to the porous structure of the tonsils, all pathogenic microbes, when trying to enter the body, are surrounded by cells of the immune system and destroyed. Adenoids are a serious barrier to infections, and if the body itself cannot cope with the disease, then inflammation of the tonsils begins.
When should you have your tonsils removed?
And yet, under certain circumstances, surgery cannot be avoided.
1. Extreme difficulty breathing
. If none of the usual treatments have sufficiently relieved the inflammation, swollen tonsils will continue to compress the throat and block the passage of air. The result is problems with the heart and blood vessels and a lack of sufficient oxygen in the brain. The consequences of this condition can be dire and irreversible.
2. Recurrent tonsillitis
. Inflammation that appears every week and constant treatment with antibiotics can provoke a decrease in immunity and cause serious harm to many organs. Sometimes it is better to remove the tonsils, lowering local immunity, but thereby saving the rest of the body.
3. Severe forms of tonsillitis
. The patient's condition may be so severe and dangerous that there is no time left for treatment with other methods. There is a danger of airway obstruction, and this is a matter of life and death.
In all other situations, surgery is not only not necessary, but can also be the beginning of more serious diseases.
Indications and contraindications for tonsillectomy
The procedure for removing the tonsils is recommended for children if:
- frequent relapses of tonsillitis - more than 5-7 exacerbations in 2 years;
- attacks of sleep apnea;
- purulent complications with every inflammation of the tonsils;
- impaired swallowing function;
- danger of developing secondary complications - kidney, liver, heart failure, rheumatism;
- difficulty breathing;
- decompensated form of pathology.
In some cases, doctors perform not complete, but partial removal of the tonsils - tonsillotomy.
Contraindications to the procedure are divided into absolute and relative (temporary). Absolute contraindications include:
- severe hematopoietic diseases;
- diabetes;
- severe mental and psychoneurological disorders;
- active pulmonary tuberculosis;
- severe renal, liver and heart failure.
Conditions in which tonsillectomy will have to be temporarily postponed include:
- acute infectious diseases accompanied by fever and general intoxication;
- caries, stomatitis, which increase the risk of infection during surgery;
- skin rashes of various origins - dermatitis, herpes, exacerbation of atopic dermatitis.
The list of possible contraindications may include other conditions. It all depends on the age and health characteristics of the individual patient, which are fully assessed by the doctor before planning the operation.
Surgical methods for removing tonsils
Previously, tonsils were removed in the simplest surgical way - using a scalpel and wire thread. Today this method is practically not used.
There are many modern methods for removing tonsils, and here are just the most popular:
1.
IR laser
. Instead of a scalpel, a laser beam is used, which immediately solders the sutures along the edges and ensures quick rehabilitation with minimal blood loss.
2. Electrocoagulation
. It works in the same way as a laser, but it heats up neighboring tissues and can lead to undesirable consequences in the form of burns. However, cases are rare, and in general the method is quite safe.
3. Ultrasound
. High-frequency ultrasound cuts off inflamed tissue and instantly heals sutures. Fast recovery and minimal blood loss also indicate the safety of this method.
4. Cryodestruction
. Freezing tonsils with liquid nitrogen. The tissue is not cut off, but frozen and gradually falls off. The procedure is painless, but recovery takes a long time and can be unpleasant.
Possible consequences of surgery for children
The likelihood of adverse events after removal of the tonsils is minimal, especially if the operation was performed in a specialized clinic. In rare cases, complications after tonsillectomy include:
- discomfort when swallowing;
- minor bleeding;
- damage to surrounding tissues during thermal excision methods;
- pain in the first time after surgery.
For the most part, all these phenomena go away on their own as the tissue heals. If the wounds have healed and the discomfort and pain have not disappeared, additional diagnostics are carried out.
The most dangerous complication is bleeding.
- In case of minor bleeding from small vessels, it is enough to treat the surface with antiseptics.
- In more serious cases, the vessel that is the source of bleeding is identified, a clamp is applied, and the bleeding tissue is sutured.
- In case of massive bleeding, tamponade is used: a gauze swab is inserted into the oral cavity and pressed against the palate under strong pressure. After 3-5 seconds, the tissue is removed to see the source of the bleeding, and then it is eliminated using a clamp and stitching. The patient is additionally administered drugs that accelerate blood clotting.
To prevent infection, a course of antibiotic therapy is prescribed before and after surgery.
Consequences of tonsil removal
One of the most unpleasant consequences is weakening of the immune system throughout the body. As mentioned above, the tonsils are a natural protective barrier that blocks the passage of many bacteria and viruses into the lungs. After their removal, infectious diseases, flu and colds may occur more often. The same new coronavirus will have easier access to your respiratory tract.
The rehabilitation itself, even with the most painless surgical methods, can become an unpleasant surprise: swelling in the bronchi, soreness, crusting and the sensation of a foreign body in the throat. No doctor can answer for sure how long this will last - everything is too individual.
Please do not resort to surgical intervention unless absolutely necessary and clearly prescribed by a doctor. The tonsils are an important organ in our body, and its presence protects us from many unpleasant diseases. Contact only trusted ENT specialists and start treatment as early as possible.
Take care of your health!
Recovery period after removal of tonsils
Complete rehabilitation occurs 2–3 weeks after the operation. During this time, the child and his parents need to follow certain measures that will help prevent the development of a new infection and injury to the palate.
- In the first 6–8 hours after removal of the tonsils, you should not give your child food or drink.
- Subsequently, for 3–6 days, the child’s diet should consist of soft, pureed foods that are easy to chew and swallow.
- You should not give babies sour, very sweet, excessively hot and salty foods.
- Cold drinks, meals and ice cream can only be offered if children have been exposed to cold foods without any consequences before surgery.
- Take medications prescribed by your doctor every day.
- Limit communication with other children, strangers and distant relatives during rehabilitation.
- Avoid visiting crowded places, swimming pools, baths, and ponds to reduce the risk of re-infection.
In the absence of complications and good health, children after tonsillectomy can lead a normal lifestyle. It is advisable to somewhat limit physical activity in the first week of rehabilitation and carefully monitor that children do not damage the palate with foreign objects.
Preparing for tonsillectomy (removal of tonsils)
In preparation for the operation, a clinical examination is carried out to ensure the safety of the surgical intervention: determination of blood group and Rh factor, blood test, urine test, determination of HIV and Australian antigen, sanitation of the oral cavity, in young children - chest x-ray to exclude thymomegaly; a thorough examination to diagnose diseases that may complicate the course of the operation and postoperative period; On the eve of the operation for children, a certificate is obtained from the clinic stating that there is no contact with carriers of childhood infections.
Several weeks before surgery, you should not take aspirin or medications containing it. It impairs blood clotting and increases the risk of bleeding. You need to tell your doctor if you are constantly taking any medications, if you are allergic to anything, if you have had reactions to a blood transfusion, if you have an increased tendency to bleed.
You should not eat or drink anything before the operation. This must be especially monitored if you plan to operate on a child. A light dinner is allowed the night before.
Surgery to remove tonsils
The operation is usually performed under general anesthesia. In extreme cases, tonsillectomy is performed under local anesthesia. For this, a solution of ultracaine is usually used. General anesthesia is usually performed using a combination of inhaled and intravenous anesthetic.
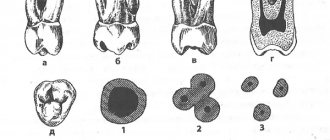
Classic tonsillectomy is as follows: after infiltration of the paratonsillar region, through an arcuate incision along the edge of the anterior arch, the upper pole of the tonsil is bluntly isolated with an elevator and grasped with forceps or a clamp. Then the tonsil is isolated with an elevator to the lower pole. The separated tonsil is removed with a special loop. Bleeding is stopped by tamponade of the niche, coagulation of blood vessels, or application of ligatures. The duration of a tonsillectomy is usually 20-30 minutes.
The numerous methods of tonsillectomy that exist today do not fundamentally change the essence of the operation. The use of lasers, radiofrequency surgery, microdebrider, and ultrasonic scalpel is aimed at reducing tissue bleeding and has virtually no effect on healing time or the severity of pain in the postoperative period.
IF YOU DECIDE TO HAVE AN OPERATION, YOU NEED TO CHOOSE THE TECHNIQUE THAT IS BEST IN THE DOCTOR YOU TRUST.
Is it necessary to remove adenoids and tonsils from an adult?
An ordinary person whose snoring prevents him from getting enough sleep cannot even think that this is due to overgrown tonsils. It is even less accepted that hearing impairment in an adult is the result of adenoid hypertrophy. It cannot be any other way, because many are sure that these diseases are characteristic only of childhood. With the otorhinolaryngologist of the Medical Center for Diagnostics and Treatment, Rimvydas Tolochka, we are in a hurry to debunk the myths rooted in society and find out whether adenoids, as well as tonsils, which have a more common name - tonsils, can poison the life of an adult?
– People very often don’t even realize how much these tonsils affect the health of already mature people. Hypertrophy of the adenoids and palatine tonsils is not exclusively a “childhood” disease, as many believe.
When talking about adenoids, such a vision of the issue is not surprising, because it was believed that by the age of 16, adenoids, even if they were present in childhood, disappear. However, adenoid tissue does not disappear anywhere and can grow at any age. The appearance of adenoids after puberty is an immune reaction. It occurs most often with a runny nose. When mucus drains into the nasopharynx, the pharyngeal tonsil reacts and the adenoids enlarge slightly. The runny nose went away in a week - good, if it lasts, becomes chronic, or turns into sinusitis, then the adenoids have no choice but to increase in size. Therefore, I strongly recommend that anyone who has had sinusitis or suffers from a chronic or allergic runny nose see a doctor.
The myth that adenoids are an exclusively childhood disease has taken root, including due to poor diagnosis. Previously, they were detected less frequently in adults, since doctors until recently had a very meager set of examination tools. The part of the nasopharynx where the adenoids are located in adults, due to its different structure compared to children, is less accessible. Therefore, the problem remained unnoticed. Not so long ago , new endoscopic research . The doctor inserts an endoscope tube into the nasal cavity and carefully examines the nasopharynx, thanks to which he can make a more correct diagnosis. This is how adenoids began to be discovered in adults.
Fortunately, the clinical manifestations of adenoid hypertrophy speak for themselves - a constantly stuffy nose, a feeling of lack of air, the patient often breathes through the mouth. Large adenoids lead to hearing loss. However, to confirm the diagnosis, you need to go to a high-level medical center, compare the Medical Center for Diagnostics and Treatment in Vilnius, where the doctor has quite expensive endoscopic equipment and can confidently say: “Yes, these are adenoids, and not a polyp, for example, or a tumor "
Conservative treatment of adenoid hypertrophy is pointless. There are no medications or physical treatments that could reduce or prevent their occurrence. You can only get rid of them surgically.
There is no hope that enlarged adenoids in an adult will disappear after some time, but they completely poison life, especially at night, when a person assumes a horizontal position and blood rushes to the head, contributing to increased swelling. This often results in snoring and apnea, which can cause problems with blood pressure and the heart and do not allow a person to fully rest, which results in feelings of fatigue, weakness, and headaches.
With the tonsils, not everything is so simple. People are accustomed to thinking that if it hurts, is inflamed or there is swelling - there is a disease, if it does not hurt or there are no visible changes - the tonsils are fine. In what cases do we, otolaryngologists, insist on surgery?
The tonsils are organs of the immune system consisting of lymphoid tissue. All their functions in the human body are not completely clear, but the main role is to protect the body from pathogenic microflora and released toxins, and to create local immunity. An increase in the size of these lymphoid formations is more often detected in childhood, but the possibility of the development of hypertrophic processes in adult patients cannot be excluded.
The exact cause of swelling of the tonsils , as well as the adenoids, is not fully understood. Their increase is most often associated with chronic tonsillitis or inflammation of the tonsils and their surrounding tissues. At the moment when the body cannot cope with the excessive load of infections, be it bacteria or viruses, and often a combination of both, the lymphoid tissue that permeates all these organs, unable to cope with the constant “attacks” of viruses and bacteria, begins to increase in size. Sometimes secondary factors such as smoking and pollution or dry air cause enlarged tonsils. Almost everyone can manifest such inflammations. However, this is largely a problem of heredity and decreased immunity.
Hypertrophied tonsils are sometimes discovered by chance, during a simple routine examination, and the patient may not experience any pain at all, as with a sore throat. Enlarged tonsils form improper nasal breathing, which leads to a cascade of pathological changes: swelling and nasal congestion (vasomotor rhinitis), concomitant damage to the auditory tube, middle ear, drying out of the mucous membrane (due to breathing through the mouth). During sleep, snoring and apnea occur, which in turn affects the quality of life, as it interferes with proper rest.
Severe hypertrophy of the tonsils in adults is an indication for surgery . However, in medical practice there are cases when the tonsils are not enlarged, but doctors also insist on their removal.
We receive such “requests”, for example, from cardiologists. The fact is that the tonsils, as organs of the immune system, produce antibodies in the fight against viruses and bacteria. Unfortunately, antibodies do not always correctly recognize the “enemy”; sometimes they attack the cells of their own body, this could be the heart muscle or, for example, joints.
An operation to remove tonsils is an extreme measure, but it is simply necessary, including in case of chronic tonsillitis, when up to several dozen (usually about 30) types of microorganisms - fungi and bacteria, most often streptococcal strains - can be found in the tonsils. In chronic tonsillitis, inflamed tonsils are a breeding ground for infection. The waste products of microbes from the tonsils can enter the blood, causing intoxication.
It manifests itself as fatigue, muscle and joint pain, headaches, decreased mood, and low-grade fever. Recently, it was possible to prove the effect of chronic tonsillitis on reproductive function in women.
To determine whether the tonsils are affected, we at the Medical Center for Diagnostics and Treatment take a throat swab for culture , a bacterial test performed to identify the type of bacteria. Moreover, I recommend carrying out such an analysis more than once. Since it is quite difficult to grow a microbe in laboratory conditions, the first negative result cannot serve as a 100% guarantee of diagnostic reliability.
The patient himself cannot decide whether to remove the tonsils and adenoids. Each situation requires a detailed, scrupulous examination. To summarize my story, the main thing that influences the doctor’s decision is the presence of complications during hypertrophy, or the presence of a permanent source of infection. Operations to remove adenoids are called adenotomy, and tonsils are called tonsillectomy. The technique of performing operations for adults is no different from operations for children. They are performed under general anesthesia to avoid the effect of the patient being “present” at the operating table. The most reliable, in my opinion, is classical surgery. Currently, laser removal is also practiced, but I do not favor this method, since it does not give the desired result - to get rid of the source of infection forever. After operations to remove tonsils and adenoids, patients who follow all doctors’ recommendations recover fairly quickly.
Despite modern, high-quality equipment, many people are afraid and try to postpone the operation indefinitely, probably hoping that it will “go away on its own.” Unfortunately, any chronic infection, just like chronic tonsillitis, not only does not go away, but without treatment can lead to complications and decreased immunity.
After talking with the patient, it turns out that most often the fear is fueled by another myth, that after the tonsils are removed, immunity will disappear . The palatine tonsils are included in the lymphoid-pharyngeal ring along with the sublingual and pharyngeal tonsils - a total of six tonsils. If you remove two of them from this chain, which are already changed anyway and are themselves a source of infection, then the other tonsils become active, take on their immunoprotective functions and compensate for everything. We explain in detail the consequences of late removal of affected palatine tonsils to everyone who, after diagnosis, refuses to undergo surgery. For example, joint pain in such patients may only decrease, but not go away completely. Most patients understand all our recommendations and trust our experience and professionalism, thanks to which they quickly return to a full, healthy life.
For patients from Daugavpils, registration and information by phone in Latvia5, in Lithuania: +370 5 247 63 69, +370 618 05 337 or by email