Bleeding is considered to be the loss of blood from the body. Bleeding can be both external and internal. Blood can flow both from body tissues damaged for certain reasons, and from natural orifices of the human body.
Healthy people can survive 15% blood loss without serious consequences. Blood from the mouth is a fairly rare phenomenon, and most often its occurrence indicates serious problems with a person’s health. What are the causes of blood from the mouth?
Why does blood appear on teeth and how to deal with the problem
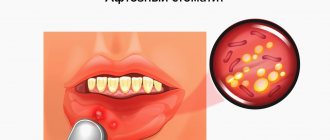
Bleeding gums are an alarming symptom that does not occur on its own, but is a sign of poor oral health. The problem cannot be left to chance. To find out the reasons for its appearance, you need to consult a dentist: if your gums are bleeding, this may indicate the development of a serious oral disease or an infection. In addition, the lack of timely treatment contributes to the appearance of bad breath, which will reduce the quality of life and lead to the development of complexes.
Survey
To identify the causes of vomiting with blood, a gastroenterologist prescribes a comprehensive examination, which is aimed at studying the morphological and functional features of the gastrointestinal tract. Instrumental studies have high diagnostic value; laboratory tests help determine the severity of hemodynamic and metabolic disorders. The examination plan includes:
- Endoscopic methods
. To accurately determine the location of bleeding and visualize the defect in the mucous membrane of the upper gastrointestinal tract, an endoscopy is performed. If necessary, during the procedure, coagulation of the affected vessel is performed, and a biopsy is taken from pathologically changed areas of tissue. - X-ray examination
. X-rays with oral contrast are performed only after vomiting has stopped and the condition has stabilized. The method is informative for diagnosing organic changes and hernial formations. Contrast leakage beyond the lumen of the gastrointestinal tract indicates perforation or fistula tracts. - Sonography
. An abdominal ultrasound is prescribed to quickly assess the condition of the abdominal organs. Sonography is used to identify space-occupying formations in the gastrointestinal tract, hernias, and diagnose liver diseases. To assess linear blood flow in the hepatic and splenic veins, Doppler sonography is performed. - Laboratory methods
. A general blood test is necessary to determine the degree of blood loss and the severity of anemic syndrome. If hereditary defects in the hemostatic system are suspected, an extended coagulogram is performed with determination of prothrombin time and other coagulation parameters. Sometimes serological tests are prescribed.
For possible primary disorders in the vascular system, contrast angiography is performed; radioisotope scintigraphy is recommended to assess the condition of the liver parenchyma. Additionally, macro- and microscopic analysis of stool is performed; to exclude intestinal bleeding, the Gregersen reaction to occult blood is informative. If hematemesis is combined with signs of hemorrhagic diathesis or general infectious syndrome, consultation with other specialists is required.
Before arrival
Causal factors for bleeding
Normally, the gums are pink, smooth, dense, and fit well to the teeth. Any changes, including the appearance of bleeding, should be cause for concern. Various reasons can provoke the occurrence of an undesirable symptom.
Oral diseases
Often the problem begins as a result of bacterial activity. Under favorable conditions, namely insufficient oral hygiene, they actively reproduce. Because of this, a soft plaque forms on the teeth, which calcifies over time. This is how tartar appears. These are already solid deposits that provoke the development of an inflammatory process, which threatens the appearance of the following diseases:
- Gingivitis. When the disease occurs, the marginal part of the gum and interdental papillae become inflamed. In addition to bleeding, redness and swelling are formed in those areas where the mucous membrane comes into contact with dental plaque.
- Periodontitis. The disease manifests itself as a result of untreated gingivitis. In this case, the pathological process moves to periodontal tissues - those that hold the tooth in the socket.
The appearance of gingivitis and periodontitis is possible not only in an adult, but also in a child. According to statistics, tartar occurs in 2/3 of all high school students, and 1/4 of school-age children experience gingivitis.
Other diseases
The cause of bleeding may be vitamin deficiency. It is difficult to determine which vitamins are lacking when it occurs, because an imbalanced diet in general has a bad effect on oral health. But it is worth introducing foods containing iron, vitamin C and potassium into your diet. If you have an unpleasant symptom, you must also exclude the following diseases and pathologies:
- disruption of the gastrointestinal tract and endocrine system;
- blood diseases;
- diabetes;
- AIDS;
- disruption of metabolic processes in the body;
- fragility of blood vessels;
- infectious diseases of the throat and nose;
- allergic reaction to medications, materials used in dentistry, toothpaste.
Bleeding gums are common in pregnant women and teenagers. This is explained by hormonal changes in the body. Expectant mothers often note that their gums hurt and swell. This condition is short-term and goes away on its own.
Common reasons
As already mentioned, blood in the mouth can occur due to poor oral hygiene. Incorrect brushing technique (strong, intense pressure) can lead to injury to the gums. Thus, using a hard toothbrush is a constant traumatic factor. Wisdom teeth are often difficult to clean. Due to problems with access, the brush hurts the gums. Bleeding may also occur for the following reasons:
- wearing braces or dentures;
- malocclusion;
- incorrect dental treatment of teeth or gums;
- smoking - bleeding occurs due to toxins that irritate saliva and weakened immunity in smokers;
- burn and injury to the mucous membrane with a sharp object;
- chipping of an old filling.
Taking certain medications can sometimes cause a decrease in the rate of saliva production. Since it resists bacteria, this can provoke a sharp development of pathogenic microflora.
Causes of vomiting blood
Peptic ulcer
Vomit like “coffee grounds” is characteristic of massive bleeding from a damaged vessel at the bottom of the ulcer.
The dark color is due to the reaction of blood hemoglobin with hydrochloric acid of the stomach, which is accompanied by the formation of hematin hydrochloride. A few days before bloody vomiting, an increase in dyspeptic disorders and abdominal pain is noted. With the onset of bleeding, the pain subsides. The leading symptoms are caused by blood loss and hypoxia: the patient feels dizzy, weak, the skin and visible mucous membranes become pale. In the case of a single release of more than 50 ml of blood, it can enter the intestines, which is manifested by black stools (melena) the next day after vomiting “coffee grounds”. With blood loss of up to 15% of the blood volume, the general condition is of moderate severity, severe weakness, tachycardia, and a drop in blood pressure are observed. Complaints of dry mouth and severe thirst appear. With the loss of large volumes of blood, fainting, disturbances of consciousness are typical, and the pulse becomes thready.
Vomit, stained with scarlet blood, is the first symptom of most stress ulcers with intense gastroduodenal bleeding. Bloody vomiting occurs suddenly in the absence of pain in the epigastric region, which is associated with the predominance of symptoms of the underlying pathology. Weakness quickly increases, dizziness appears, the skin turns pale, and the pulse quickens. Bloody vomiting after night and morning “hungry” abdominal pain is also complicated by Zollinger-Ellison syndrome, in which multiple bleeding ulcerative defects of the gastric mucosa are formed.
Diseases of the gastroduodenal zone
Inflammatory processes, structural anomalies of the upper digestive tract and tumor formations can serve as predisposing factors for vomiting “coffee grounds”. The symptom occurs when the pathology is long-standing, when the mucous membrane is completely affected and the vessels are involved in the process. The difference from bleeding with ulcerative defects is the persistence of pain after vomiting. The causes of bloody vomiting are:
- Acute erosive gastritis
. Vomiting is preceded by moderate pain in the epigastric region, nausea, belching of air, and loss of appetite. With small hemorrhages, streaks of blood are found in the contents of the vomit; with extensive damage to the organ and massive bleeding, vomiting “coffee grounds” with black tarry stool (melena) begins. Similar symptoms are found in hyperplastic gastritis. - Hemorrhagic gastritis
. Inclusions of blood in vomit are characteristic of acute profuse bleeding. Vomiting develops against the background of pain in the epigastrium, which intensifies immediately after eating. Before the attack, severe nausea is felt for some time. With chronic blood loss, a metallic taste in the mouth, frequent dizziness, and shortness of breath when performing usual physical activity are possible. - Gastric diverticulum
. Bloody vomiting is a late sign of diverticulosis. This complication usually occurs when the disease persists for a long time and indicates an erosive process that damages the arteries. Before vomiting or simultaneously with it, a sharp pain is felt in the epigastrium. The next day, the stool usually becomes dark and tarry. - Acute gastric dilatation
. Repeated vomiting of gastric contents, and then masses mixed with bile and blood, begins after the sudden appearance of severe diffuse pain in the abdominal cavity and indomitable hiccups. More than 7-8 liters of vomit are released per day, while attacks occur spontaneously without the conscious efforts of the patient. There is gas retention and bloating. The condition is somewhat alleviated in the knee-elbow position. - Benign tumors
. Vomiting “coffee grounds” and melena are the first symptoms of massive bleeding in gastric leiomyoma, which, due to its slow progression, remains latent for a long time. Large bleeding polyps of the stomach are characterized by the presence of individual streaks of blood in the secreted vomit against the background of other dyspeptic disorders. - Erosive bulbitis
. Bloody vomiting indicates severe bleeding from an eroded vessel in the wall of the duodenal bulb. Due to significant blood loss, disturbances in general health are possible - weakness, pallor, fainting. Unlike most other pathologies, tarry stools often precede vomiting; less often, melena occurs after an attack.
Diseases of the esophagus
Esophageal pathology is accompanied by vomiting with the discharge of bright scarlet blood (hematemesis). The symptom is characteristic of inflammatory processes, in which the vulnerability of the mucous membrane increases, and superficial or deep defects are formed. Hematemesis is provoked by trauma to the wall of the esophagus by foreign bodies, iatrogenic damage during medical procedures. Among the main reasons for the development of symptoms are:
- Mallory-Weiss syndrome
. Bleeding is provoked by prolonged vomiting or hiccups, during which the smooth muscles of the gastrointestinal tract wall and the abdominal muscles are greatly strained. Against the background of the next urge to vomit, a sharp burning pain is felt in the area of the xiphoid process, after which profuse vomiting of blood begins. The symptom is also detected in cases of rupture of the esophagus of another etiology (burns, thoracoabdominal trauma). - Acute esophagitis.
The prerequisite for bleeding and vomiting is the formation of erosions or ulcers of the esophagus due to the protracted course of the inflammatory process. With the onset of the attack, sharp pains in the chest, typical for damage to the esophagus, intensify, occurring after eating and in a horizontal position. Signs of posthemorrhagic anemia appear - weakness, fatigue, dizziness. Before vomiting, belching of air, heartburn, and nausea are observed. - Hiatal hernia
. Vomiting blood is one of the signs of strangulation of the hernial sac. It occurs suddenly or against a background of nausea and is combined with sharp chest pain, which can radiate to the shoulder blades and neck. The patient's general condition is severe - shortness of breath is pronounced, the skin becomes cyanotic, the pulse quickens to 100 or more beats per minute, and blood pressure drops. - Perforation of the esophagus
. With a through defect of the organ wall, repeated vomiting with impurities of fresh blood is typical, then the vomit takes on the appearance of “coffee grounds.” Severe pain is noted, which in intensity resembles a myocardial infarction or perforation of a stomach ulcer. When air enters the cellular space of the mediastinum and neck, subcutaneous emphysema develops and breathing becomes difficult. - Tracheoesophageal fistula
. Bloody vomiting is provoked by the presence of an acquired anastomosis between the esophagus and trachea, which contributes to the destruction of the vessels of the mucous membrane. The symptom is often accompanied by breathing problems - coughing, suffocation, hemoptysis. The possible presence of a trioesophageal fistula as a cause of vomiting is indicated by moderate chest and epigastric pain, coughing up pieces of food, and a tendency to frequent diseases of the lungs and bronchi. - Esophageal carcinoma.
Vomiting usually occurs when the tumor is large and partially covers the lumen of the organ. The symptom is combined with difficulty swallowing solid food, a constant sensation of a foreign body (“lump”) behind the sternum, hoarseness, and a constant dry cough. The presence of blood streaks in the vomit is characteristic of the late stage of the disease with ulceration and disintegration of neoplasia.
Portal hypertension
The main cause of vomiting blood with increased pressure in the portal vein is varicose veins of the esophagus. These vessels have a specific feature: they do not collapse, so blood loss is abundant (up to 30-40% of the blood volume), which is life-threatening. Children may experience fountain vomiting with the release of bright red blood, which is an unfavorable prognostic sign. Portal hypertension with vomiting can be caused by pylephlebitis, congenital fibrosis of the liver, and structural anomalies of large venous vessels of the abdominal cavity.
Bleeding from the esophageal veins is characteristic of the decompensated stage of the disease. At the same time, in the initial stages of portal hypertension, nausea, periodic heartburn or belching, and stool disturbances are disturbing. As the pathological process progresses, patients notice swelling in the lower extremities, and an expanded venous network is clearly visible on the skin of the anterior abdominal wall. Dull pain is felt in the left hypochondrium, which is caused by an enlarged spleen.
Infectious diseases
Vomiting blood occurs in the hemorrhagic form of dengue fever or yellow fever. These viral infections affect the vascular wall and disrupt the blood coagulation system. Against the background of high fever and general infectious syndrome, uterine, nasal, and gastrointestinal bleeding occurs. Bloody vomiting can begin with the intestinal form of anthrax, in which case it is combined with melena, excruciating abdominal pain. The discharge of blood with vomit is typical for the initial period of the plague, which affects all organ systems.
Hemorrhagic syndromes
Regurgitation of vomit containing blood is a typical sign of gastrointestinal bleeding in hemorrhagic diathesis. More often, vomiting “coffee grounds” complicates the course of thrombocytopenic purpura and hemorrhagic vasculitis. In addition to dyspeptic disorders, such patients complain of a macular or papular rash on the limbs and torso. Massive nasal and intestinal bleeding, triggering the gag reflex, are pathognomonic for rare hereditary pathologies - Wiskott-Aldrich syndrome and Randu-Osler-Weber disease.
Acute conditions
In children, vomiting blood may be a sign of systemic intoxication due to extensive burns or neurotoxicosis. Such conditions, in addition to regurgitation, are characterized by an extremely serious condition of the child, disturbances of consciousness, and dysfunction of the cardiovascular and respiratory systems. Repeated bloody vomiting, detected on the second or third day of post-resuscitation illness, acute peritonitis, cardiogenic shock, indicates gastrointestinal bleeding due to the developed hemorrhagic syndrome.
Pathology of ENT organs
Vomiting of “coffee grounds” is observed with heavy nosebleeds, which are accompanied by ingestion of blood. This often results in dizziness, weakness, unpleasant taste in the mouth, and nausea. Massive blood loss provokes fainting, tachycardia, and severe pallor of the skin. The release of vomit in the form of “coffee grounds” is also characteristic of combined burns of the pharynx, which are combined with damage to the underlying parts of the gastrointestinal tract, ammonia poisoning (if ingested), causing destruction of the mucous membrane.
Complications of pharmacotherapy
Sometimes bloody vomiting is a consequence of gastrointestinal bleeding, provoked by so-called ulcerogenic drugs - drugs that contribute to the formation of erosive and ulcerative defects in the mucous membrane of the digestive organs. As a rule, patients report long-term, sometimes uncontrolled use or high dosage use of the following groups of medications:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
: aspirin, indomethacin, butadione. - Glucocorticosteroids
: prednisolone, dexamethasone. - Direct oral anticoagulants
: dabigatran, apixaban, rivaroxaban. - Antigout drugs
: atophan, zinchofen. - Antihypertensive sympatholytics
: reserpine. - Psychostimulants
: caffeine, some narcotics (cocaine, methamphetamines).
Symptoms accompanying gum disease
Pathologies that cause blood from the mouth may be accompanied by a number of other unpleasant symptoms:
- swelling of the gums;
- pain when pressing or eating solid foods (sometimes the pain is quite severe);
- itching and discomfort in the gum tissue;
- bad breath;
- tooth mobility (with advanced dental diseases).
Even if nothing bothers you throughout the day, and blood appears only when brushing your teeth, this may indicate a problem.
Bleeding in lung cancer: features
Lung cancer is considered one of the most common cancer pathologies among men. In most cases, it develops against the background of chronic inflammatory diseases of the respiratory system. The main risk factor is considered to be tobacco abuse over many years. The source of bleeding in cancer is damaged blood vessels or the tumor itself, which is in the decay phase.
Signs of the disease are a prolonged dry cough that cannot be treated. After a few months, hemoptysis occurs. In addition, fever, severe weakness, shortness of breath and weight loss are noted. Bleeding can have a different volume: from small (50-100 ml) to profuse (more than 0.5 liters). In most cases it is accompanied by a cough. In this case, there is a high risk of aspiration and the development of hemorrhagic shock.
How to quickly stop bleeding from gums
What to do if you need to quickly stop bleeding from your gums? For this purpose, you can use one of the following methods:
- Rinse your mouth with cold water or mint mouthwash. Decoctions of herbs - chamomile, oak bark, fir, calendula - help reduce the manifestations of unwanted symptoms.
- Apply a cotton swab soaked in chlorhexidine to the bleeding area. You need to press it tightly and wait until the bleeding stops.
- Glue a special protective homeopathic strip. You can buy it at the pharmacy.
No matter how long your gums bleed, you cannot put off a visit to the dentist. The problem will not go away on its own, but will only get worse.
How to eliminate constant bleeding gums
To carry out successful treatment, it is important to find out why the gums are bleeding. You should not self-medicate, since the problem requires an integrated approach, which consists in eliminating the cause and restoring the health of the gums. Only a doctor can tell you how to treat a disease that causes bleeding. Different techniques may be needed.
Professional teeth cleaning
If dental plaque provokes complications in the form of bleeding, it is necessary to thoroughly clean your teeth. This does not mean ordinary hygiene procedures at home, but hardware cleaning in a dental office. The doctor uses ultrasound to crush the tartar, the particles of which are washed out with a mixture of water and air. You need to carry out a hygiene procedure twice a year. Unfortunately, not all patients comply with such recommendations.
Air Flow technology is used to remove soft deposits. In this case, finely dispersed soda is supplied along with water. After the procedure is completed, the teeth are polished, which further prevents the accumulation of plaque.
Such actions are sufficient for diagnosed gingivitis. The doctor will also tell you what to do to restore the mucous membrane. This may include rinsing or taking certain medications. Professional teeth cleaning is used if gingivitis has progressed to periodontitis. But this is only the beginning of treatment. Let's talk about ways to eliminate the disease further. If periodontal pockets have formed, you will need powerful ultrasound devices, such as Vector. In this case, the periodontist should deal with oral hygiene.
Rinse with solutions
Antiseptic treatment of the oral cavity can be carried out in the form of rinses based on the following agents:
- "Furacilina";
- "Rotokana";
- "Miramistina";
- "Chlorhexidine";
- alcohol solution "Chlorophyllipt".
Soda-saline solution also helps. You can add a few drops of iodine to it. It is better to use solutions through an irrigator - this increases their effectiveness. In case of bleeding, you need to use special toothpastes, including Parodontax, Lakalut, Colgate Total Pro. The compositions should not have a bleaching effect.
Drug therapy
To eliminate bleeding gums, the doctor may prescribe ointments and gels. They are applied to the problem area after rinsing the mouth. The following drugs are in demand in dental practice:
- "Metrogil Denta" - has antibacterial and anti-inflammatory properties, often prescribed for stomatitis, after tooth extraction;
- “Asepta” is a propolis-based gel that quickly relieves inflammation;
- "Kamistad" is a drug available in two forms (for children and adults);
- "Elugel" is a strong antiseptic that effectively fights pathogenic environments.
For inflammatory processes, the doctor may prescribe medicinal bandages, antibiotics (in some cases), and a course of vitamins.
Gum curettage
For periodontitis with the formation of deep periodontal pockets, the following surgical techniques are used:
- Closed curettage. To carry out the procedure, the doctor uses a special instrument – a curette. With its help, the doctor cleans the roots of the teeth. The tool penetrates to a depth of 3 mm.
- Open curettage. The technique is used when the deposits are deeper. It involves the following actions: peeling of the gums, cleaning and antibacterial treatment, suturing.
The disease can be cured using an integrated approach. Therefore, it is important to follow all doctor’s recommendations even after the procedure.
2. Reasons
Of all diseases of the hematopoietic system, the oral mucosa (OM) is most sensitive to two groups of diseases, one of which concerns red blood cells (erythrocytes) and the hemoglobin associated with them, the other - white blood cells, or leukocytes.
The group of anemia includes a number of diseases and pathological conditions in which the number of red blood cells decreases and the hemoglobin content in the blood decreases.
The group of leukemias includes malignant diseases of the hematopoietic system, in which the proliferation (abnormal multiplication and growth) of blood cells or bone marrow, as well as the activity of the hematopoietic parenchyma, precedes the maturation and differentiation of blood cells (i.e., their acquisition of one or another functional type), therefore, a large number of altered, atypical, immature leukocytes - leukoblasts, myeloblasts, etc. - appear in the blood.
Both anemia and leukemia, with all their etiopathogenetic and clinical diversity, which certainly deserves separate consideration, affect the state of the oral mucosa in more than 90% of patients, and often a preliminary diagnosis is made precisely on the basis of specific changes in the oral mucosa.
Visit our Oncology page
Preventive measures
To avoid gum problems, you must follow a number of simple rules:
- Perform high-quality and correct hygiene procedures aimed at oral health. It is necessary to select care products that will not injure the mucous membrane. You should brush your teeth morning and evening. Use dental floss with caution. Instead, you can use an irrigator, which will help effectively remove food debris. Your toothbrush should be changed every three months.
- Balance your diet. The body must receive all the necessary vitamins and minerals. To strengthen teeth and gums, it is important to eat solid plant foods, such as apples and carrots.
- Give up bad habits, in particular smoking. Toothpicks should be used with caution.
- Regularly undergo preventive examinations at the dentist - at least twice a year. This will allow timely detection of oral diseases.
Paying close attention to your oral health will help you maintain a beautiful and healthy smile for many years.
"Diclofenac"
Another NSAID drug. Relatively safe, good pain relief.
Tablets are recommended for toothache. They contain from 25 mg to 100 mg of diclofenac sodium.
The medicine is prohibited:
- children under 6 years of age (if the dosage is more than 25 mg), and adolescents under 18 years of age (if the dosage exceeds 100 mg);
- for erosions and ulcers of the digestive organs;
- if the patient is intolerant to non-steroidal anti-inflammatory drugs.
Contraindicated for pregnant and lactating women.
Prescribe with caution to people with heart, kidney and liver failure.
- Bleeding in the middle of the cycle: causes
Diclofenac will relieve pain faster and more effectively if you take it half an hour before meals. The maximum dose per 24 hours is 150 mg, divided into 2 to 3 doses.